Abstract
An enlarged arterial diameter is associated with an increased risk for cardiovascular disease. This study examined the relationship of noninvasively measured brachial artery cross-sectional area with cardiovascular risk factors and arterial stiffness in a middle-aged male population. Absolute volumetric changes of the brachial artery were measured with a newly developed oscillometric method during a general health examination in 387 men (mean age: 38±9 years) without known cardiovascular disease. Based on the measurement, the estimated area (eA) of the brachial artery at end-diastole was obtained. Brachial artery volume elastic modulus (VE) and brachial–ankle pulse wave velocity (baPWV) were simultaneously measured as indices of arterial stiffness by the same device. The relationships of eA with cardiovascular risk factors, including age, obesity, hypertension, dyslipidemia, impaired fasting glucose/diabetes mellitus (IFG/DM), hyperuricemia, smoking and their associated continuous variables, as well as VE and baPWV, were examined. Overall, the mean eA was 12.9±2.9 mm2. The eA was significantly higher in subjects with obesity, hypertension or IFG/DM than in those without each of these risk factors. In a multiple linear regression analysis, body mass index (β=0.31, P<0.001), age (β=0.25, P<0.001), systolic blood pressure (β=0.16, P=0.004) and pulse rate (β=−0.13, P=0.005) were independent determinants of eA. In contrast, neither VE nor baPWV were selected as independent determinants of eA. In conclusion, enlarged brachial artery cross-sectional area was significantly associated with cardiovascular risk factors such as age, body mass index and systolic blood pressure, but it was not associated with increased arterial stiffness.
Similar content being viewed by others
Introduction
Enlargement of arterial diameter is thought to be an initial step toward the progression of atherosclerosis.1, 2 Previous studies have shown the relationship between the diameter of the brachial artery and conventional cardiovascular risk factors,3 including metabolic syndrome.4 Brachial artery diameter is also positively associated with brachial intima–media thickness5 and negatively associated with brachial flow-mediated vasodilation.6, 7, 8 Interestingly, enlargement of brachial artery diameter is shown in subjects with coronary artery calcification8 and in those with increased carotid intima–media thickness.3, 9 In a population-based cohort study, brachial artery diameter predicted the risk of cardiovascular disease (CVD).10 Taken together, these observations suggest the usefulness of measuring brachial artery diameter in clinical and epidemiological settings for identifying individuals with impaired arterial function, those with atherosclerosis and those at high-risk for CVD. However, one major limitation of measuring brachial artery diameter is that, to date, ultrasonography has been almost the sole noninvasive method and, in fact, it requires particular examination techniques.11
Recently, a new device based on an oscillometric method has been developed for the measurement of brachial artery cross-sectional area, which is virtually identical to the diameter. This measurement does not require any particular expertise, indicating the potential for wider application of measuring brachial artery cross-sectional area using this oscillometric device. However, clinical and epidemiological data on the relevance of the measurement has been lacking so far. The objective of this study was to measure the brachial artery cross-sectional area using the oscillometric device and to examine its relationship with cardiovascular risk factors in a middle-aged male population without known CVD. This study also examined the relationship between brachial artery cross-sectional area and arterial stiffness, which is a well-known risk marker for CVD independent of conventional cardiovascular risk factors.12
Methods
Study population
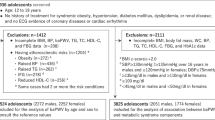
This study was conducted during an annual health examination at a semiconductor manufacturing plant in Kanagawa, Japan, in 2011. Out of 403 male workers who underwent a complete health examination, 15 were excluded because the oscillometric measurements did not succeed. An individual with ankle–brachial blood pressure (BP) index ⩽0.9 was also excluded. We initially intended to exclude subjects with CVD, but there were no such subjects. Finally, this included 387 subjects (mean age: 38±9 years; range: 20–62 years). There were 36 female workers who also underwent the health examination, and oscillometric measurement was successful in 33 female workers. However, to obtain statistical results for a more homogeneous population and because of their relatively small number, we did not include the results of the female workers in the main analysis. The study was approved by the Ethics Committee of Nippon Medical School, and all participants gave written informed consent.
Data collection
All participants underwent anthropometric and BP measurements and blood sampling in a temperature-controlled room maintained at 22±2 °C. Body weight and height were measured and body mass index (BMI) was calculated as the weight (kg) divided by the square of the height (m2). Obesity was defined as BMI ⩾25.0 kg m−2.
The brachial systolic and diastolic BP were measured by well-trained staff members with mercury sphygmomanometers and an optimal cuff size for the arm circumference. BP measurements were taken on the right arm with the subject seated after at least 5 min of rest. Hypertension was defined as systolic BP ⩾140 mm Hg, diastolic BP ⩾90 mm Hg or current use of antihypertensive medications.
Blood samples were obtained from the antecubital vein after overnight fasting. White blood cell counts were measured using an automatic cell counter. Standard enzymatic methods were used to measure the serum low-density lipoprotein (LDL) cholesterol, triglycerides, uric acid and plasma glucose levels and hemoglobin A1c (HbA1c). The serum high-density lipoprotein (HDL) cholesterol level was measured using a direct method. Dyslipidemia was defined as LDL cholesterol ⩾140 mg dl−1, HDL cholesterol <40 mg dl−1, triglycerides ⩾150 mg dl−1 or current use of antidyslipidemic medications. Hyperuricemia was defined as uric acid ⩾7.0 mg dl−1 or current use of uric acid-lowering medications. Impaired fasting glucose (IFG) was defined as fasting plasma glucose ⩾110 mg dl−1 and diabetes mellitus (DM) was defined as fasting plasma glucose ⩾126 mg dl−1, HbA1c ⩾6.5% or current use of glucose-lowering medications.
A self-reported questionnaire was used to check subjects’ smoking status, which was categorized as current or no smoking. Current smoking was defined as cigarette smoking on a regular basis (at least once daily) at the time of study participation.
The 30-year risk of incident CVD according to the Framingham CVD risk prediction algorithm13 was calculated on the basis of age, BMI, systolic BP, smoking and DM status and use of antihypertensive medication. The estimated risk is shown as a percentage and categorized as low (<10%), intermediate (10–20%) and high (>20%).
Oscillometric measurement
Brachial artery absolute volume was measured using a newly developed device, the Health Chronos TM-2771 prototype (A&D Company, Tokyo, Japan). This device consists of a main unit and four cuffs for oscillometric BP measurement and plethysmography at the right and left brachial and tibial arteries. The outsides of the occlusive cuffs are composed of a hard material to avoid expansion with increases in arterial volume, so that the changes in the cuff pressure (CP) accurately reflect volumetric changes of the artery.
To measure brachial artery absolute volume, the device initially sought the lowest CP that indicated complete collapse of the brachial artery (volume=0) at end-diastole. The brachial artery plethysmogram was recorded at this CP. During the measurement, air for calibration flowed from the main unit into the cuff. This calibration makes it possible to determine the absolute volumetric changes of the brachial artery from the plethysmogram under the condition of cuff inflation (Figure 1a). Thereafter, the CP was gradually decreased and the calibrated plethysmogram was recorded several times at regular CP intervals.
(a) A brachial artery plethysmogram with calibration (arrow). (b) A representative pressure (blood pressure (BP)−cuff pressure (CP) difference)–area (cross-sectional area) curve. Estimated area (eA) of the brachial artery is obtained when the BP−CP difference is identical to diastolic BP (DBP). Volume elastic modulus (VE) of the brachial artery is calculated as the change in the BP−CP difference (ΔP1) per 1% increase in cross-sectional area at P1 (AP1), where P1 is defined as P0+40 mm Hg and P0 is defined as the point with the lowest CP indicating complete collapse of the brachial artery.
The main unit next described a pressure (BP−CP difference)–area (brachial artery cross-sectional area) curve as an approximate logarithmic curve (Figure 1b), using the data obtained from the plethysmogram. The brachial artery cross-sectional area was calculated as the brachial artery volume divided by the brachial cuff length. Estimated cross-sectional area and volume elastic modulus (VE) of the brachial artery were obtained from the pressure–area curve. The eA was defined as the cross-sectional area at the point where the BP−CP difference was identical to the diastolic BP (that is, end-diastolic cross-sectional area). The lowest CP indicating complete collapse of the brachial artery is usually a little higher than BP; therefore, the corresponding point (P0) on the pressure axis of the curve was set at less than zero. VE was defined as the change in the BP−CP difference (ΔP1) per 1% increase in cross-sectional area at P1, where P1=P0+40 mm Hg. We previously reported that eA closely correlated with the brachial artery diameter measured with ultrasonography (r=0.93) in healthy subjects.14 In the previous report, we also showed that the coefficients of variation of eA and VE for two consecutive measurements were 3.6% and 8.3%, respectively.14
Before the above measurements, brachial–ankle pulse wave velocity (baPWV) was measured by nearly the same methods described elsewhere with another commercially available device.15
The values of eA, VE and baPWV for the right and left sides were, respectively, averaged and used in the subsequent statistical analysis.
Statistical analysis
All statistical tests were performed using SPSS software version 19.0.0 (IBM Corporation, Somers, NY, USA). Continuous variables with and without a skewed distribution were expressed as the median (interquartile range) and the mean±s.d., respectively. Categorical data were expressed as the percent of total. The unpaired Student’s t-test and an analysis of variance with the post hoc Bonferroni multiple comparisons were used to examine the difference between the two groups and among the three groups, respectively. Pearson’s correlation coefficient was analyzed to determine the simple correlation between variables. A multiple linear regression analysis was conducted to examine the independent determinants of eA among cardiovascular risk factors and the indices of arterial stiffness. In the analysis, variables that showed a P-value <0.2 by the Pearson’s correlation coefficient were used as explanatory variables. All statistical tests were two-sided, and a P-value <0.05 was considered significant.
Results
The characteristics of the study participants are described in Table 1. The means or the medians of cardiovascular risk parameters were found to be within acceptable ranges. The prevalence of participants who were taking medications for hypertension, dyslipidemia, DM and hyperuricemia was 3.9%, 2.1%, 0.8% and 2.1%, respectively.
Overall, the mean eA, VE and baPWV were 12.9±2.9 mm2, 0.98±0.19 mm Hg per % and 1277±181 cm s−1, respectively. The scatter plots between eA and VE or baPWV are shown in Figure 2. A significant but weak correlation was found between eA and VE (r=0.16, P=0.002) as well as eA and baPWV (r=0.20, P<0.001).
As shown in Figure 3, eA was significantly higher in subjects with obesity, hypertension, dyslipidemia or IFG/DM than in those without each of these risk factors. In contrast, eA was found to be similar between subjects with and without hyperuricemia or current smoking.
A significant correlation was observed between eA and the Framingham CVD risk (r=0.32, P<0.001). When the subjects were divided according to the Framingham CVD risk category, eA gradually increased across the categories and significant differences in eA were found among all combinations of the categories (all P<0.001; Figure 4).
As noted in Table 2, eA significantly and positively correlated with age, BMI, systolic and diastolic BP, log-transformed triglycerides, fasting plasma glucose, HbA1c and uric acid, while it tended to correlate negatively with pulse rate in a univariate analysis. In a multiple linear regression analysis, Model 1 (VE and baPWV-excluded model) showed that age, BMI, systolic BP and pulse rate were independent determinants of eA. In Model 2 (VE and baPWV-included model), the same independent determinants as those seen in Model 1 were observed, while neither VE nor baPWV were selected as independent determinants of eA.
Sensitivity analyses were next conducted. When diastolic BP was substituted for systolic BP as an explanatory variable in the multiple linear regression analysis (Model 2), age, BMI and pulse rate remained as independent determinants of eA (data not shown). However, diastolic BP did not reach a statistically significant level as an independent determinant (β=0.10, P=0.064). Next, when the multiple linear regression analysis (Model 2) was conducted in the 372 subjects who were not taking antihypertensive medications (that is, vasoactive drugs), all of the same independent determinants as those seen in the main analysis (age, BMI, systolic BP and pulse rate) were observed (data not shown). Finally, when the multiple linear regression analysis (Model 2) was repeated in only the 357 subjects who were not taking any medications for hypertension, dyslipidemia, DM or hyperuricemia, the results were substantially maintained, except that fasting plasma glucose was further selected as an independent determinant of eA (data not shown).
In regard to the indices of arterial stiffness, VE significantly correlated with age (r=0.29, P<0.001) and pulse rate (r=−0.22, P<0.001), but did not correlate with any other cardiovascular risk parameters used in this study (data not shown). Similarly, baPWV significantly correlated with age (r=0.53, P<0.001) and pulse rate (r=0.25, P<0.001), and further correlated with a number of cardiovascular risk parameters, such as BMI, systolic and diastolic BP, white blood cell count, fasting plasma glucose and HbA1c, triglycerides and LDL cholesterol and uric acid (data not shown).
The characteristics and tentative results of the correlation analysis between eA and cardiovascular risk parameters in 33 female workers are listed in Supplementary Tables S1 and S2, respectively.
Discussion
This study showed that eA was independently associated with age, BMI, systolic BP and pulse rate in a population of middle-aged men without known CVD. In contrast, no independent association was observed between eA and either VE or baPWV. To our knowledge, this is the first study to focus on the extent of brachial artery enlargement evaluated by the oscillometric method and to examine its relationship with cardiovascular risk factors and arterial stiffness.
In a multivariate analysis, age was an independent determinant of eA in this study. Arterial diameter has been reported to increase with advancing age.4 The present findings are therefore in line with earlier observations. Among other cardiovascular risk factors considered in this analysis, BMI and systolic BP were independent determinants of eA, which also supports the findings in this study that eA is larger in subjects with obesity or hypertension than in those without each of these risk factors. These results are also consistent with previous observations of the significant associations of BP or obesity indices with brachial or carotid artery diameters.3, 16 From a clinical perspective, these observations suggest that eA may be a useful marker for evaluating the effects of these risk factors on brachial artery enlargement. Earlier studies have reported that matrix metalloproteinases, a family of zinc-dependent endopeptidases capable of degrading all of the components of the extracellular matrix, have a crucial role in vascular remodeling.17 It has also been reported that matrix metalloproteinases, in particular matrix metalloproteinase-9, are increased in patients with hypertension and/or obesity.18, 19, 20 Matrix metalloproteinases, while not measured in this study, may be involved in the association of eA with BMI and systolic BP.
This study showed that eA gradually increased as the CVD risk category, as determined by the Framingham CVD risk prediction algorithm, increased.13 These are convincing results, because the Framingham CVD risk prediction algorithm incorporates variables that also showed a significant correlation with eA in this study, including age, BMI and systolic BP. These findings are further supported by the previous reports of the positive association between the enlargement of brachial artery diameter and increased risk of CVD.10 The usefulness of eA as a risk marker for future cardiovascular event is anticipated.
Unexpectedly, eA was not significantly associated with lipid profiles, uric acid levels, white blood cell counts or current smoking status, all of which have been reported elsewhere to be associated with impaired arterial properties.11, 21, 22, 23, 24 One possible reason for this finding is that the duration of exposure to these risk factors could not be evaluated because of the cross-sectional nature of this study. Alternatively, it is possible that brachial artery enlargement is not intrinsically influenced by these risk factors in this study population. Further longitudinal investigations would be needed to address this issue.
Although eA significantly correlated with both VE and baPWV in a univariate analysis, independent associations were not observed in a multivariate model that included cardiovascular risk factors as explanatory variables. These findings suggest the existence of some confounding factors for the relationship of eA with VE or baPWV. Similar to the positive correlation between eA and age, VE significantly and positively correlated with age in this study. It is also well known that baPWV is increased with advancing age25 and, in fact, baPWV also significantly and positively correlated with age in this study. These results suggest that age is at least one of the potential confounding factors. Taken together, the lack of independent association of eA with VE or baPWV seen in this study raises the possibility of a different clinical significance of eA from that of VE or baPWV. This point may merit further investigation.
Another important finding of this study was the negative association of eA with pulse rate. This indicates that caution is needed when evaluating eA in subjects with bradycardia or tachycardia. However, the association with pulse rate is not specific to eA, but is shown in other noninvasive measures of arterial properties as well, including PWV and augmentation index.11
There are limitations to this study. First, as noted above, this was a cross-sectional investigation. Therefore, the causal relationship between eA and cardiovascular risk factors could not be clarified. Second, the study participants included only middle-aged Japanese men at a single site. Therefore, it is unclear whether these results can be extrapolated to other populations, including female subjects, the elderly and other ethnic groups. In particular, female workers were not included in the main analysis because their number was relatively small. In fact, the results of the correlation analysis in female workers (Supplementary Table S2) appeared to be inconsistent with those in male workers, thus suggesting that a larger sample size may be needed to further discuss the relationship of eA with cardiovascular risk parameters in female workers.
In conclusion, this study showed that eA was significantly associated with age, BMI and systolic BP in a population of middle-aged men. These results suggest that eA may be a useful marker for evaluating the effects of these risk factors on brachial artery enlargement. In addition, eA was not independently associated with the indices of arterial stiffness, VE or baPWV, thus suggesting a different clinical significance of eA from that of VE or baPWV. To date, ultrasonography, which requires a skilled examiner, has been almost the sole noninvasive method to measure brachial artery diameter. In this regard, the oscillometric measurement technique presented here offers a simple and more operator-independent method to evaluate noninvasively brachial artery cross-sectional area. Further studies to examine the usefulness of this measurement in various clinical and epidemiological settings are anticipated.
References
Montalcini T, Gorgone G, Gazzaruso C, Romeo S, Bosco D, Pujia A . Brachial artery diameter measurement: a tool to simplify non-invasive vascular assessment. Nutr Metab Cardiovasc Dis 2012; 22: 8–13.
Glagov S, Weisenberg E, Zarins CK, Stankunavicius R, Kolettis GJ . Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med 1987; 316: 1371–1375.
Holewijn S, den Heijer M, Swinkels DW, Stalenhoef AF, de Graaf J . Brachial artery diameter is related to cardiovascular risk factors and intima–media thickness. Eur J Clin Invest 2009; 39: 554–560.
Montalcini T, Gorgone G, Gazzaruso C, Garzaniti A, Pujia A . Large brachial artery diameter and metabolic syndrome in postmenopausal women. Atherosclerosis 2010; 210: 458–460.
Iwamoto Y, Maruhashi T, Fujii Y, Idei N, Fujimura N, Mikami S, Kajikawa M, Matsumoto T, Kihara Y, Chayama K, Noma K, Nakashima A, Higashi Y . Intima–media thickness of brachial artery, vascular function, and cardiovascular risk factors. Arterioscler Thromb Vasc Biol 2012; 32: 2295–2303.
Celermajer DS, Sorensen KE, Gooch VM, Spiegelhalter DJ, Miller OI, Sullivan ID, Lloyd JK, Deanfield JE . Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 1992; 340: 1111–1115.
Herrington DM, Fan L, Drum M, Riley WA, Pusser BE, Crouse JR, Burke GL, McBurnie MA, Morgan TM, Espeland MA . Brachial flow-mediated vasodilator responses in population-based research: methods, reproducibility and effects of age, gender and baseline diameter. J Cardiovasc Risk 2001; 8: 319–328.
Kullo IJ, Malik AR, Bielak LF, Sheedy PF 2nd, Turner ST, Peyser PA . Brachial artery diameter and vasodilator response to nitroglycerine, but not flow-mediated dilatation, are associated with the presence and quantity of coronary artery calcium in asymptomatic adults. Clin Sci (Lond) 2007; 112: 175–182.
Gullu H, Erdogan D, Caliskan M, Tok D, Yildirim E, Ulus T, Turan Sezgin A, Muderrisoglu H . Interrelationship between noninvasive predictors of atherosclerosis: transthoracic coronary flow reserve, flow-mediated dilation, carotid intima-media thickness, aortic stiffness, aortic distensibility, elastic modulus, and brachial artery diameter. Echocardiography 2006; 23: 835–842.
Yeboah J, Crouse JR, Hsu FC, Burke GL, Herrington DM . Brachial flow-mediated dilation predicts incident cardiovascular events in older adults: the Cardiovascular Health Study. Circulation 2007; 115: 2390–2397.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H . Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27: 2588–2605.
Sakuragi S, Abhayaratna WP . Arterial stiffness: methods of measurement, physiologic determinants and prediction of cardiovascular outcomes. Int J Cardiol 2010; 138: 112–118.
Pencina MJ, D’Agostino RB Sr, Larson MG, Massaro JM, Vasan RS . Predicting the 30-year risk of cardiovascular disease: the framingham heart study. Circulation 2009; 119: 3078–3084.
Munakata R, Otsuka T, Umeda M, Kato K, Ibuki C, Seino Y . Reproducibility and accuracy of oscillometric measurement of the brachial artery cross-sectional area. Ther Res 2012; 30: 1701–1709 (in Japanese with English abstract).
Yamashina A, Tomiyama H, Takeda K, Tsuda H, Arai T, Hirose K, Koji Y, Hori S, Yamamoto Y . Validity, reproducibility, and clinical significance of noninvasive brachial–ankle pulse wave velocity measurement. Hypertens Res 2002; 25: 359–364.
Kozakova M, Palombo C, Paterni M, Anderwald CH, Konrad T, Colgan MP, Flyvbjerg A, Dekker J . Body composition and common carotid artery remodeling in a healthy population. J Clin Endocrinol Metab 2008; 93: 3325–3332.
Galis ZS, Khatri JJ . Matrix metalloproteinases in vascular remodeling and atherogenesis: the good, the bad, and the ugly. Circ Res 2002; 90: 251–262.
Hopps E, Caimi G . Matrix metalloproteinases in metabolic syndrome. Eur J Intern Med 2012; 23: 99–104.
Marchesi C, Dentali F, Nicolini E, Maresca AM, Tayebjee MH, Franz M, Guasti L, Venco A, Schiffrin EL, Lip GY, Grandi AM . Plasma levels of matrix metalloproteinases and their inhibitors in hypertension: a systematic review and meta-analysis. J Hypertens 2012; 30: 3–16.
Fontana V, Silva PS, Gerlach RF, Tanus-Santos JE . Circulating matrix metalloproteinases and their inhibitors in hypertension. Clin Chim Acta 2012; 413: 656–662.
Ishizaka N, Ishizaka Y, Toda E, Hashimoto H, Nagai R, Yamakado M . Higher serum uric acid is associated with increased arterial stiffness in Japanese individuals. Atherosclerosis 2007; 192: 131–137.
Vlachopoulos C, Xaplanteris P, Vyssoulis G, Bratsas A, Baou K, Tzamou V, Aznaouridis K, Dima I, Lazaros G, Stefanadis C . Association of serum uric acid level with aortic stiffness and arterial wave reflections in newly diagnosed, never-treated hypertension. Am J Hypertens 2011; 24: 33–39.
Lee YJ, Lee JW, Kim JK, Lee JH, Kim JH, Kwon KY, Lee HR, Lee DC, Shim JY . Elevated white blood cell count is associated with arterial stiffness. Nutr Metab Cardiovasc Dis 2009; 19: 3–7.
Tomiyama H, Hashimoto H, Tanaka H, Matsumoto C, Odaira M, Yamada J, Yoshida M, Shiina K, Nagata M, Yamashina A . Continuous smoking and progression of arterial stiffening: a prospective study. J Am Coll Cardiol 2010; 55: 1979–1987.
Tomiyama H, Yamashina A, Arai T, Hirose K, Koji Y, Chikamori T, Hori S, Yamamoto Y, Doba N, Hinohara S . Influences of age and gender on results of noninvasive brachial-ankle pulse wave velocity measurement-a survey of 12517 subjects. Atherosclerosis 2003; 166: 303–309.
Acknowledgements
This study was supported, in part, by the Grant-in-Aid for Young Scientists (B), from the Ministry of Education, Culture, Sports, Science and Technology (MEXT KAKENHI Grant Number 21790561). We thank Chiharu Komiya and Yuka Sugimori for their technical assistance in collecting the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Otsuka, T., Munakata, R., Kato, K. et al. Oscillometric measurement of brachial artery cross-sectional area and its relationship with cardiovascular risk factors and arterial stiffness in a middle-aged male population. Hypertens Res 36, 910–915 (2013). https://doi.org/10.1038/hr.2013.56
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2013.56
Keywords
This article is cited by
-
Incidence and predictors of left ventricular remodeling among elderly Asian women: a community-based cohort study
BMC Geriatrics (2017)
-
Risks and predictors of mild diastolic dysfunction among middle-aged and aged women: a population-based cohort study
Journal of Human Hypertension (2016)
-
Volume elastic modulus of the brachial artery and coronary artery stenosis in patients with suspected stable coronary artery disease
Heart and Vessels (2016)
-
Considerations for SphygmoCor radial artery pulse wave analysis: side selection and peripheral arterial blood pressure calibration
Hypertension Research (2015)
-
The impact of angiotensin receptor blockers on arterial stiffness: a meta-analysis
Hypertension Research (2015)