Abstract
Purpose
To determine whether prophylactic laser peripheral iridotomy (LPI) for primary angle closure (PAC) is associated with cataract progression.
Methods
In 1999, Mongolian volunteers aged ⩾50 years were invited to participate in a longitudinal study. Glaucoma was excluded in all participants and 712 of them were selected to undergo a full ophthalmic examination as part of the study protocol. Lenses were graded and PAC diagnosed using international classification systems. In 2005, all traced participants underwent a similar dilated examination. Diagnosis of cataract progression was based on the inter-observer variation +2 standard deviations. The association between LPI at baseline and cataract progression was assessed using χ2-test and logistic regression.
Results
Of 712 participants, 158 were diagnosed with occludable angles and treated with LPI. In 2005, 137 participants (19.2%) had died, 315 (315/575=54.8%) were traced, and dilated examination was performed on 276 (48%) of them. Progression of nuclear opacity (NO), cortical, and posterior subcapsular (PSC) opacities were evident in 40 (14.5%, 95% confidence interval (CI)=10.6–19.2%), 89 (32.2%, 95% CI=26.8–38.1%), and 11 participants (4.0%, 95% CI=2.0–7.0%), respectively. Although NO was more likely to progress in those with LPI in a crude analysis (odds ratio (OR)=2.02, 95% CI=1.00–4.11, P=0.05), no evidence of an independent association was detected in multivariate analysis adjusting for age, sex, and baseline Schaffer grading (adjusted OR=1.24, 0.41–3.75, P=0.7). There was no evidence of an association between LPI and progression of PSC or cortical opacities.
Conclusions
There is no evidence that prophylactic LPI is independently associated with cataract progression in this study.
Similar content being viewed by others
Background
Glaucoma is the leading cause of irreversible blindness.1 Primary angle closure (PAC) glaucoma (PACG) is an important source of visual morbidity in Asian countries.2, 3 Although more people are affected by primary open angle glaucoma (POAG), PACG blinds nearly half of those affected compared with POAG, which blinds 25% of sufferers.3, 4
Laser peripheral iridotomy (LPI) is the most effective intervention for the majority of cases of PAC.5, 6 Iridotomies relieve pupil block in patients presenting with acute PAC (APAC) and almost completely protects the fellow eye from symptomatic episodes.7 Ultrasound biomicroscopy (UBM) studies of treated fellow eyes have shown that LPI can result in a significant widening of the angle, 2 weeks after treatment.5 LPI is also more effective if performed in the earlier stages of disease.6 A major concern is the potential for complications that may arise from prophylactic treatment, especially if applied to people with an early precursor of disease that may not lead to morbidity in their lifetime.8, 9 In particular, there is a theoretical long-term risk of cataract formation due to the disturbance of normal aqueous flow.8, 9 There has been much interest in this potential risk with different studies showing differing results.10, 11 For example, a study from Singapore suggested that there was a potential association between LPI and cataract progression, whereas another study from the United States showed no association. One possible explanation for these differences is that different populations may experience different underlying cataract progression rates, which may affect the observed cataract progression rates after LPI.10
The aim of this study was to investigate the association between prophylactic LPI for PAC suspects (PACS) and PAC and cataract progression in a longitudinal study with a 6-year follow-up.
Materials and methods
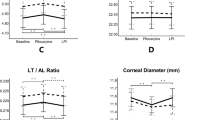
This longitudinal study was nested within a randomised controlled screening trial in Mongolia, designed to investigate prophylactic LPI in the prevention of PACG. The study was carried out in accordance with the World Medical Association's Declaration of Helsinki. The methods and preliminary results of the baseline study have already been described.12 In brief, all residents from the capital Ulaanbaatar and the rural province of Bayanhongor aged ⩾50 years were invited to participate in the trial. Glaucoma was excluded in all participants. A full ophthalmic examination was performed on 712 of 4597 participants who had failed a screening test or were examined because of suspicious discs detected on direct ophthalmoscopy. This included LogMAR visual acuity, central anterior chamber depth (cACD) using slit lamp mounted ultrasound A-scan, slit lamp examination of the anterior segment, Goldmann applanation tonometry, modified van Herrick grading, gonioscopy, dilated lens, and fundus examination. Lenses were graded using the Lens Opacity Classification (LOCS) III system with reference to photographic standards at the slit lamp.13 Lenses were graded to the nearest 0.5 U. At baseline, the slit lamp examination, including gonioscopy and subsequent LOCS III grading under maximal dilation with tropicamide, was performed by one observer (WPN) with 690 participants consenting to dilatation. Of the 712 examined participants, 550 had open angles and 162 were diagnosed with occludable angles (62 PAC and 100 PACS) using the International Society for Geographical and Epidemiological Organisation grading system,14 of which 158 had LPI in both eyes. PACS was diagnosed in participants with an occludable angle on gonioscopy (where ⩾270° of the posterior trabecular meshwork could not be seen), but no evidence of peripheral anterior synechiae (PAS), raised IOP, previous acute angle closure, or glaucomatous damage. PAC was diagnosed in those with an occludable angle and features indicating that trabecular obstruction had occurred, such as PAS, raised IOP, signs of previous acute angle closure, or excessive pigment on the trabecular surface, but no evidence of glaucomatous damage.
Participants were located through contact tracing, asking key informants, and by reviewing national registration records, 6 years later. Deaths were ascertained through the same methods. At follow-up, all traced participants underwent a full ophthalmic examination similar to that described at baseline, including a dilated LOCS III grading on the same slit lamp. This was performed by a single observer at follow-up (JLY). Inter-observer variability between WN and JLY was evaluated by consecutive lens grading at the same slit lamp of the right eye of 25 patients with severity ranging from 2 to 6 for nuclear opacity (NO) and colour; from 0 to 2.5 for cortical opacity; and from 0 to 1.5 for posterior subcapsular (PSC) opacity. There was good agreement between baseline and follow-up observers for LOCS III grading (weighted kappa⩾0.5 for all types of lens opacity). All data were collected using standardised forms and double entered independently into a computerised database.
Cataract progression was defined as inter-observer variation +2 standard deviations and rounded up to the nearest 0.5 U. This resulted in a cutoff point of an increase of 1 LOCS III grade for NO, nuclear colour, and PSC opacity and an increase of 1.5 U for cortical lens opacity. Data obtained from the right eye only were analysed.
The association between cataract progression and demographic and ocular variables were assessed using χ2-test for categorical variables and t-test or the Wilcoxon rank sum test for quantitative variables. The association between LPI at baseline and cataract progression was assessed using χ2-test and logistic regression in multivariate models using a stepwise approach to account for detected and a priori confounders. Detected confounders were identified by a statistically significant association (based on cutoff <0.1 for inclusion in model) with both the putative risk factor (LPI) and the outcome (cataract progression). Important a priori confounders such as age and sex were included in the final model. Tests for interaction between variables within the final models were also performed. Differences in baseline characteristics between subjects who did and did not attend for re-examination were analysed to assess the effect of bias on the results. Participants who were known to have died were excluded from this analysis.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Results
Of the 712 participants examined at baseline, 6 years later, 137 (19. 2%) had died and 315 (315/575=54.8%) were traced and re-examined between March and September 2005. Of 158 participants who had LPI at baseline, 30 (21.9%) had died and 80 (80/128=62.5%) were re-examined. Of 315 traced participants, 39 refused dilation or had corneal opacities that precluded a full lens examination. The results are presented for 276 participants with full dilated examination at follow-up.
The mean age of the traced cohort was 69.6 years (range 55–91 years), 70 of whom (23.0%) were men. The life expectancy of Mongolians in 2005 was 64 years; therefore, we expected a high death rate in our study population. There was no difference in baseline cup disc ratio (CDR) between participants who were re-examined and those who were lost to follow-up (both CDR median 0.3, inter-quartile range 0.2–0.4, Wilcoxon rank sum test for difference P=0.23).
Lens characteristics
The baseline and follow-up characteristics of lens opacities are summarised in Table 1. As grading of nuclear colour and NO were closely correlated, only NO will be described. Overall, 40 participants (15.4%, 95% CI=10.4–18.8%) were diagnosed with progression of NO and 89 (32.2%, 95% CI=26.8–38.1%) had evidence of progression of cortical opacity. Only 4 participants (1.5%, 95% CI=0.4–3.7%) had evidence of PSC opacity at baseline with progression evident in 11 participants (4.0%, 95% CI=2.0–7.0%).
The baseline lens characteristics of the group with follow-up were similar to the whole baseline group examined, and there was no statistical evidence of a difference in baseline lens characteristics in those with and without follow-up (all P<0.01).
Risk factors
The association between ocular and demographic risk factors with LPI is shown in Table 2, and with cataract progression in Table 3. LPI was performed on participants who had shallower cACD and narrower Shaffer grading at baseline (P<0.01). Progression of cortical opacity and PSC opacity, but not NO, was associated with older age (P<0.01 and 0.03, respectively). There was no association between gender and progression of any type of lens opacity. There was no association between cataract progression and screening IOP or cACD measurements.
There was weak evidence that NO was more likely to progress in those with LPI in a crude analysis (21.7 vs 12.1%, odds ratio (OR)=2.02, 95% CI=1.00–4.11, P=0.05). However, in a multivariate analysis adjusting for age and sex as a priori confounders and baseline Shaffer grading as a detected confounder, no association was found (adjusted OR=1.24, 95% CI=0.41–3.75, P=0.7). There was no evidence that LPI was associated with progression of cortical or PSC lens opacities. No interactions were detected in any of the multivariate models examined (Table 4).
Progression of NO only was associated with a reduction in visual acuity. There was also evidence to suggest that participants with LPI at baseline had greater reduction of vision over the 6-year follow-up. However, LPI was no longer associated with reduction of vision in multiple regression analysis adjusting for age, sex, and NO progression.
A total of 10 people with lens examination at baseline had undergone cataract surgery in the interim period, all of whom had NO or NO in combination with other types of opacities. There was no association between cataract surgery and LPI performed at baseline.
Discussion
This study has provided information on the association between LPI and cataract progression from a community-based sample in East Asia. The baseline study showed that all participants had evidence of NO, nearly a quarter had cortical opacity (23.2%), but PSC opacity was less common (1.5%). At follow-up, progression was noted in 14.5% of NO scores, 32.2% of cortical opacity, and 4.0% of PSC opacity. Progression of NO was comparable with the findings of a study undertaken in Australia (19.3% over 5 years),15 but was lower than that detected in the Longitudinal Cataract Study (45.8% over 5 years)16 and the Beaver Dam Eye Study (70% over 5 years).17 Progression in our study was higher than that reported among Blacks in Barbados (3.6% over 4 years).18 However, different classifications and definitions were used in these studies making comparisons misleading and therefore should be viewed with caution.15
A higher proportion of participants treated with LPI at baseline had progression of NO (22.9% with LPI vs 13.0% without LPI, P=0.05), but the association was not statistically significant after adjusting for age, sex, and baseline Shaffer grading. There were also higher proportions of progression for PSC opacity, but this was not statistically significant. PSC opacity is the most commonly reported type of cataract to occur after trabeculectomy,19 and is the type of cataract most likely to occur as a potential complication of prophylactic LPI due to disturbances in aqueous flow. A clinic-based study involving an urban East Asian population reported that 16.7% of patients with LPI showed evidence of progression of PSC opacity after 12 months,11 but the study suffered from lack of controls and high loss to follow-up.20 Similarly, a letter in response to this study showed a high rate of cataract extraction after prophylactic LPI in a Caucasian population. However, in this report, there were also no controls, nor was there evidence that cataract extraction was performed for symptomatic cataract progression.21 In our study, we did not find an independent effect of prophylactic LPI on the 6-year PSC opacity progression, but the small number of cases may have reduced the ability of the data to detect an effect. Assuming 4.0% progression in the untreated group (taken from the overall PSC progression rate from this study) and 16.7% in the LPI group (taken from the PSC progression rate from the study by Lim et al11), this study would have had 85% power to detect an effect. There was good agreement between observers for LOCS III grading, which suggests that the results were less likely to be due to measurement error; in addition, we used two standard deviations of the inter-observer variation as a cutoff for diagnosis of progression. Although different diagnostic criteria for cataract progression yield different estimates for incidence and progression,15 there was no association between LPI and progression of any type of cataract using different cutoff points in this data set.
We presented results from participants who were traced and re-examined with dilatation. Excluding available data can bias results; however, similar results were obtained with analysis using all available data, including participants examined without dilatation. There were no differences in either baseline LOCSIII scores for any cataract type or baseline CDRs between those who were re-examined and those not re-examined, suggesting that those who were re-examined are likely to be representative of the whole cohort. This would reduce the likelihood of an effect from selection bias due to the loss in follow-up on the results.
Narrower baseline angle width was identified as confounding the association between LPI and progression of NO. This has a biological basis with a theoretical risk that alteration in aqueous outflow dynamics could influence exposure of the lens to aqueous flow,8 which in turn may hasten the development of opacities. In the multivariate model with age, sex, and LPI, neither narrower angles nor LPI were independent risk factors for NO progression. This suggests that the effects of narrow angles at baseline and LPI on cataract progression are interdependent, wherein the initial relationship between LPI and NO progression may be mediated through narrower baseline Shaffer grading. It is also possible that progression of NO may be associated with both narrower angles and subsequent LPI.
Prophylactic LPI is commonly used in standard clinical practice to protect fellow eyes from acute angle closure and clinical guidelines also recommend that LPI be considered for potentially occludable angles.22, 23, 24 This study has shown that LPI is not independently associated with cataract progression and supports the findings in Bobrow's10 clinical study from the United States. However, further studies from East Asian populations are necessary to corroborate these findings. In addition, the question of whether narrow angles themselves are associated with cataract progression is an important question to address, as this will repeatedly confound the association between prophylactic LPI and cataract progression. An alternative treatment for occludable angles is cataract surgery, which also widens narrow angles.25 This could potentially address both PACG and cataract blindness with one procedure and trials are currently ongoing.26 However, the potential complications from intraocular surgery are greater than for LPI, and using this approach to prevent PACG in some settings may not be feasible. There remains an important role of prophylactic LPI in the treatment of occludable angles.

References
Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, Pokharel GP et al. Global data on visual impairment in the year 2002. Bull World Health Organ 2004; 82: 844–851.
Foster PJ, Johnson GJ . Glaucoma in China: how big is the problem? Br J Ophthalmol 2001; 85: 1277–1282.
Foster PJ, Oen FT, Machin D, Ng TP, Devereux JG, Johnson GJ et al. The prevalence of glaucoma in Chinese residents of Singapore: a cross-sectional population survey of the Tanjong Pagar district. Arch Ophthalmol 2000; 118: 1105–1111.
Quigley HA, Broman AT . The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006; 90: 262–267.
Gazzard G, Friedman DS, Devereux JG, Chew P, Seah SK . A prospective ultrasound biomicroscopy evaluation of changes in anterior segment morphology after laser iridotomy in Asian eyes. Ophthalmology 2003; 110: 630–638.
Nolan WP, Foster PJ, Devereux JG, Uranchimeg D, Johnson GJ, Baasanhu J . YAG laser iridotomy treatment for primary angle closure in East Asian eyes. Br J Ophthalmol 2000; 84: 1255–1259.
Lowe RF . The natural history and principles of treatment of primary angle-closure glaucoma. Am J Ophthalmol 1966; 61: 642–651.
Caronia RM, Liebmann JM, Stegman Z, Sokol J, Ritch R . Increase in iris-lens contact after laser iridotomy for pupillary block angle closure. Am J Ophthalmol 1996; 122: 53–57.
Friedman DS . Who needs an iridotomy? Br J Ophthalmol 2001; 85: 1019–1021.
Bobrow JC . Factors influencing cataract formation after Nd:YAG laser peripheral iridotomy. Trans Am Ophthalmol Soc 2008; 106: 93–97; discussion 97–9.
Lim LS, Husain R, Gazzard G, Seah SK, Aung T . Cataract progression after prophylactic laser peripheral iridotomy: potential implications for the prevention of glaucoma blindness. Ophthalmology 2005; 112: 1355–1359.
Nolan WP, Baasanhu J, Undraa A, Uranchimeg D, Ganzorig S, Johnson GJ . Screening for primary angle closure in Mongolia: a randomised controlled trial to determine whether screening and prophylactic treatment will reduce the incidence of primary angle closure glaucoma in an east Asian population. Br J Ophthalmol 2003; 87: 271–274.
Chylack Jr LT, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL et al. The Lens Opacities Classification System III. The longitudinal study of cataract study group. Arch Ophthalmol 1993; 111: 831–836.
Foster PJ, Buhrmann R, Quigley HA, Johnson GJ . The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol 2002; 86: 238–242.
McCarty CA, Mukesh BN, Dimitrov PN, Taylor HR . Incidence and progression of cataract in the Melbourne Visual Impairment Project. Am J Ophthalmol 2003; 136: 10–17.
Leske MC, Chylack Jr LT, Wu SY, Schoenfeld E, He Q, Friend J et al. Incidence and progression of nuclear opacities in the Longitudinal Study of Cataract. Ophthalmology 1996; 103: 705–712.
Klein BE, Klein R, Lee KE . Diabetes, cardiovascular disease, selected cardiovascular disease risk factors, and the 5-year incidence of age-related cataract and progression of lens opacities: the Beaver Dam Eye Study. Am J Ophthalmol 1998; 126: 782–790.
Leske MC, Wu SY, Nemesure B, Li X, Hennis A, Connell AM . Incidence and progression of lens opacities in the Barbados Eye Studies. Ophthalmology 2000; 107: 1267–1273.
Husain R, Aung T, Gazzard G, Foster PJ, Devereux JG, Chew PT et al. Effect of trabeculectomy on lens opacities in an East Asian population. Arch Ophthalmol 2006; 124: 787–792.
Yip JL, Jones E, Foster PJ, Nolan WP, Friedman DS . Cataract after laser iridotomy. Ophthalmology 2006; 113: 1467; author reply 1467–8.
Tsatsos M, Eke T . Cataract after laser iridotomy. Ophthalmology 2006; 113: 1252; author reply 1252.
American Academy of Ophthalmology Glaucoma Panel. Primary Angle Closure. American Academy of Ophthalmology: San Francisco, 2005.
Ang MH, Baskaran M, Kumar RS, Chew PT, Oen FT, Wong HT et al. National survey of ophthalmologists in Singapore for the assessment and management of asymptomatic angle closure. J Glaucoma 2008; 17: 1–4.
Sheth HG, Goel R, Jain S . UK national survey of prophylactic YAG iridotomy. Eye 2005; 19: 981–984.
Nonaka A, Kondo T, Kikuchi M, Yamashiro K, Fujihara M, Iwawaki T et al. Angle widening and alteration of ciliary process configuration after cataract surgery for primary angle closure. Ophthalmology 2006; 113: 437–441.
Lam DS, Leung DY, Tham CC, Li FC, Kwong YY, Chiu TY et al. Randomized trial of early phacoemulsification versus peripheral iridotomy to prevent intraocular pressure rise after acute primary angle closure. Ophthalmology 2008; 115: 1134–1140.
Acknowledgements
We would like to thank Drs Davaasambuu Tsendenkhuu and Tsedendavaa, Chimed Oyunsuren, Tsedengonbo Lhagvasuren, Dr Tsagaan Altantsetseg from Sukbaator District hospital, and Dr Legtsegdulam Altantsetseg from Bayanzurkh District hospital, the staff of Sukbaator District hospital, Bayanhongor hospital, and Bolor Melmii who worked on this project. This work was funded by the Wellcome Trust, British Council for Prevention of Blindness (London), Christian Blind Mission (CBM) (Bensheim), The National Lotteries Fund through Fight for Sight (London). The Yag laser used in this study was donated by the Velux Foundation, Copenhagen. We acknowledge a proportion of our financial support from the Department of Health through the award made by the National Institute for Health Research to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology for a Specialist Biomedical Research Centre for Ophthalmology. The views expressed in this publication are those of the authors and not necessarily those of the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Yip, J., Nolan, W., Gilbert, C. et al. Prophylactic laser peripheral iridotomy and cataract progression. Eye 24, 1127–1135 (2010). https://doi.org/10.1038/eye.2010.59
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.59
Keywords
This article is cited by
-
Reply to Yip et al
Eye (2011)
-
Reply to Athanasiadis et al
Eye (2011)