Abstract
Aim To determine the magnitude of visual impairment (VI) resulting from lens opacity/cataract among a rural population in southwestern Nigeria.
Method A population-based cross-sectional survey using a multistage sampling method to select subjects ⩾50 years. Participants with pinhole visual acuity of ⩽6/18 in their better eye, exclusively from lens opacity/cataract, were further examined by an ophthalmologist. Their level of VI was categorised using the International Classification of Disease tenth revision and lens opacity was graded using the World Health Organization's cataract grading system.
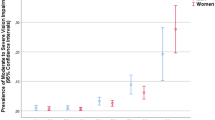
Results From the enumerated population of 1200 subjects, 1031 subjects were examined. The prevalence of VI from cataract/lens opacity in the population studied was 11.9% (95% CI: 10.1–14.0) with a cataract blindness prevalence of 2.0% (95% CI: 1.3–3.0). The odds for VI increased with increasing age and female patients had 1.6 times the odds for cataract blindness than did male patients. Mixed cataract was the most prevalent of the visually disabling cataract. (3.9% (95% CI: 2.8–5.2)), whereas posterior subcapsular cataract was the least prevalent (2.5% (95% CI: 1.7–3.7)).
Conclusion VI from cataract remains a public health problem in the Akinyele district of Nigeria. The need for a comprehensive cataract surgical service using the VISION 2020 model is necessary in the district if the burden from the backlog of visually disabling cataract is to be reduced.
Similar content being viewed by others
Introduction
There are 161 million people worldwide who are visually disabled, of whom 124 million have low vision and 37 million are blind, according to the 2002 World Health Organization's (WHO) global estimate.1 Approximately 80% of visually impaired people live in the low-resource countries of Africa and Asia, mostly in rural areas with few or underutilised eye-care facilities.2, 3, 4
The prevalence of blindness in Sub-Saharan Africa ranges from 0.3 to 1.3%, whereas for low vision it ranges from 1.4 to 3.6%.5
Age-related cataract remains the world's leading cause of curable blindness and is the main target of VISION 2020—the Right to sight.6 This joint initiative of WHO and the International Agency for the Prevention of Blindness is directed at eliminating avoidable blindness by the year 2020 and its successful implementation requires accurate community-based data.6
Determining the prevalence of visually disabling, unoperated cataract remains one of the indicators commonly used in planning any cataract surgical service. There had been many studies in southwestern Nigeria7, 8, 9, 10, 11, 12 and Sub-Saharan Africa13, 14, 15, 16 on blindness and visual impairment (VI) using the Rapid assessment of cataract surgical service methodology, a WHO validated research tool.17 These studies tend to underestimate the true burden of cataract visual disability as the focus was more on blinding cataract.
There are no robust population-based epidemiological data on the singular contribution of different morphological types of lens opacity on VI in Sub-Saharan Africa. It is known that different cataract types differ in their ability to cause visual disability and as such the need for surgery.18
Akinyele Local Government Area (LGA), the largest of the 32 LGA in Oyo state has a 2006 projected population figure of 343,118, projected from the 1991 population census figure.19 It is predominantly a rural population. There is no eye clinic in the area but there are two government referral hospitals in the state capital. A need assessment survey was necessitated in the LGA because of an on-going collaboration between the University College Hospital, Ibadan Eye Department, which was recently upgraded to a WHO Regional training centre and a centre for high-volume cataract surgery, and the authority of Akinyele LGA towards implementing the VISION 2020 program.
In this paper, findings from the Akinyele Eye study are reported with respect to the prevalence and magnitude of VI caused by different morphological types of lens opacity.
Patients and methods
The Akinyele District Eye study is a population-based cross-sectional survey on both blinding and non-blinding eye diseases in the Akinyele district of Oyo state, southwestern Nigeria. Approval for the survey was obtained from the Institutional Review Board of the University of Ibadan/University College Hospital, Ibadan and the Akinyele Local Government Authority. Informed verbal consent was also obtained from individuals who participated in the survey, as most of them had no formal education.
The survey that was conducted among residents aged ⩾50 years took place between September 2006 and January 2007.
Study design
The study population was selected by a multistage cluster sampling technique. The 1991 census data on the local government area was used to generate a list of villages in the district to create a sampling frame. Forty clusters were randomly selected from the sampling frame of 193 villages on the basis of probability proportional to size. In the final sampling, people aged ⩾50 years, who had been residents for a minimum of 6 months in the selected village (cluster), were enumerated for the survey. This was carried out by randomly choosing a direction in the village and enumerating all eligible people in the households along the direction until the desired number had been enumerated.
Data collection was conducted in three stages:
Enumeration—the socio-demographic data of eligible participants in the selected households were collected on a questionnaire. This was carried out by trained field assistants during a door-to-door enumeration.
Visual acuity testing—the presenting distant visual acuity (VA) was measured using a standard Snellen E chart at a distance of 6 m in open daylight. Participants with presenting VA of <6/18 had their VA checked with a multi-fenestrated pin hole. The VA measured separately for each eye was recorded. Participants with pinhole VA of <6/18 in the better eye were further examined by an ophthalmologist at a central examination site. VA testing (presenting and pinhole) was performed by the trained community health workers. The training of the community health workers was carried out by the second author (AOA).
Comprehensive eye examination—Detailed examination of the external eye and anterior segment was performed by an Ophthalmologist using a pen torch and a slit-lamp biomicroscope (Haag Streit, Koeniz, Switzerland). Pupillary reaction was evaluated and an oblique light test was used to exclude individuals with a shallow anterior chamber, who may be at risk of suffering from post-dilatation acute angle closure.
Pupillary dilatation was performed for 15 min. Fundoscopy was carried out using a direct ophthalmoscope. This was followed by grading of lens opacity on the slit lamp using the WHO cataract grading system.20
Visually disabling cataract/lens opacity was defined for the purpose of the survey as the presence of lens opacity/cataract in either eye of such magnitude as to cause a corrected acuity of <6/18 in the better eye.
-
Grading of lens opacity was performed by the first author (OOK). The levels of visual impairment are categorised using the ICD 10 classification of visual impairment.21
Treatment for minor eye problems was provided free of charge at the examination site, and participants with other pathologies, including refractive error, were sent to the University College Hospital, Ibadan Eye Centre.
We certify that all applicable institutional and governmental regulations regarding the ethical use of human volunteers were followed during this research.
Excluded from analysis were
-
participants with cornea pathology of such severity as to cause visual impairment,
-
participants with presumed advanced glaucoma with cup disc ratio of more than 0.8,
-
presence of maculopathies, retinal detachment and other non-glaucomatous optic atrophy,
-
participants in whom the lens opacity/cataract were assumed to have been secondary to trauma or intraocular inflammation, and
-
individuals in whom the lens opacity had been present before their estimated fiftieth birthday.
Statistical analysis
Data were analysed on SPSS 12. The prevalence rate and the 95% confidence interval of the visually disabling cataract were estimated for different age groups and gender. Frequency table and percentages were used where necessary. Univariate analysis was performed to determine whether age and gender were significantly related to lens-related visual impairment.
The χ2-test was applied to assess differences in categorical variables between groups.
The P-value quoted was two sided and was considered statistically significant at a value of <0.05.
Results
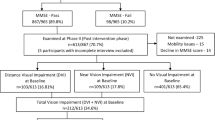
A total of 1200 subjects were enumerated for the survey and 1031 subjects participated, giving a participation rate of 85.9%. There were 527 males and 504 females, giving a male to female ratio of 1.05:1. The mean age of the participants was 64.9 years (SD 11.5).
Thirty-three percent of the subjects were aged between 50 and 59 years, whereas 35.5% were ⩾70 years. 83.2% of the subjects had no form of formal education. Majority of the subjects (62.7%) were peasant farmers. Table 1 shows the demographic characteristics of the participants.
One hundred and two subjects (9.9%) had low vision, whereas 21 (2.0%) had blindness from their cataract according to the WHO categorisation of VI. The mean age of the subjects who were cataract blind was 72.0 years (SD 11.8; range: 60.0), for those with low vision, the mean age was 67.5 years (SD 12.2; range: 55.0), whereas for those with pin hole VA>6/18 the mean age was 60.7 years (SD 9.0; range: 40 years). The prevalence of blindness and low vision on the basis of both presenting and pin hole VA among the participants according to the WHO categorisation of VI is shown in Table 2 .
The prevalence of blindness and low vision increased with increasing age. The rates of blindness and low vision were 0.2 and 1.5%, respectively, for those aged 50–59 years. Table 3a shows the prevalence of blindness and low vision from lens opacity by age group and gender. Age ⩾70 years was significantly associated with cataract blindness, whereas the factors significantly associated with cataract low vision included the age group ⩾60 years as well as female gender. Table 3b shows the association of cataract VI with age and gender.
Mixed cataract was the most prevalent of the visually disabling cataract (3.9% (95% CI; 2.8, 5.2)).Table 4 shows the distribution of visually disabling cataract on the basis of morphological type.
Discussion
This study provides vital epidemiological data on cataract blindness and VI among people aged ⩾50 years living in a rural area of southwestern Nigeria. The prevalence of 11.9% for cataract VI and 2.0% for cataract blindness among the population is high, even more so when compared with some earlier studies on blindness and VI in this geopolitical zone as well as in other parts of Sub-Saharan Africa.
An outright comparison of our data with these other studies may not be too appropriate because of the differences in methodology, the definitions adopted, and the age group involved in such studies. Oluleye,9 in a blindness survey in three villages in Akinyele district using the rapid assessment of cataract surgical service protocol, reported cataract blindness prevalence of 0.84%. Onakpoya et al10 reported 0.63% for cataract blindness and 3.6% for cataract VI. This study included all age groups. Moreover, Adeoti7 found a cataract blindness prevalence of 0.6% among her study population. Both studies were conducted among populations in southwestern Nigeria.
In the Delta region of Nigeria, cataract VI and blindness prevalence, of 13.0% and 3.78%, respectively, were reported,12 whereas Rabiu13 in northern Nigeria found a cataract blindness prevalence of 3.6%.
Confining our survey to a rural population that is underserved in terms of eye care services and in instances where such available services are not affordable could also account for the high prevalence of cataract VI. Oye et al,16 in a survey in a semi-urban population in Cameroun, reported cataract blindness prevalence of 0.23%, severe VI prevalence of 0.13%, and VI prevalence of 1.44% from cataract and lens opacity. However, among a rural Chinese population, Li et al22 found cataract VI prevalence of 4.6% and cataract blindness of 1.3%. Also in Papua New Guinea,23 a cataract VI prevalence of 7.4% (95% CI 6.4–10.2) was reported.
The age distribution pattern of the study population may also have accounted for these high rates. 35.5% of the participants were aged ⩾70 years. Advancing age remains a leading risk factor for the development of cataract. This age distribution pattern can be attributed to urban–rural migration of these elderly people on retirement.
The cataract surgical coverage per person at VA <3/60 is worth considering. Eight of the enumerated subjects have had cataract extraction (three pseudophakic, three aphakic, and two couching). The cataract surgical coverage (both orthodox and couching) is 27.6%. Although this is an improvement over the 13.6% reported by Oluleye7 in an earlier survey 8 years ago in the same area and compares with the 22.1% reported by Rabiu,13 it is still a far cry from the 77.1% reported among a Pakistani population24 and the 56.5% reported in India.25
The risk factors associated with cataract blindness and VI in our study was in accordance with those in other studies. They included increasing age25, 26 and the female gender.1 The higher odds for cataract VI among the female gender may be because of the differences in the use of cataract surgical services. Only two of the subjects, who have assessed cataract surgical service were female. This might be connected to the fact that the men are seen as the ‘bread winner’ in this area and hence have more access to the family resources.
It is interesting, but not surprising, that all the subjects who were cataract blind had no formal education. Their eye-care-seeking behaviour may be poor because of the low demand for fine vision, as they were engaged in subsistent farming or trading.
Mixed cataract being the most prevalent form of visually disabling cataract may not be too surprising. The study conducted by Chua et al27 has shown that the estimated effect of mixed cataract on VA is at least the sum of the independent effect from each of the cataract morphological type and as such cause more image degradation.
Extrapolating the blindness and VI prevalences to the estimated 10.5% of the Akinyele population aged ⩾50 years on the basis of the projected 2006 population figure of about 343 118 yields a mean of 4200 people who are visually impaired from lens opacity, and of these about 700 are bilaterally blind. There is the obvious need to increase the cataract surgical rate in this study population if we desire to clear this backlog of visually disabling cataract.
This study had its strength in the use of a standard sampling method in choosing the study population with a fair response rate (85.9%). The grading of lens opacity was performed by a single ophthalmologist after 2 weeks of training by a more senior ophthalmologist (AAO). There was a good interobserver agreement after the period of training.
However, our survey was not without its limitations. Such a study that confined to only the rural area may not be totally representative of the entire district, but a more larger study with the population chosen along an urban rural strata may be more representative. The decision to limit our survey to the rural area was partly because of the limited resources available to the investigator; hence, the focus on the underserved areas. Also the age- and sex-adjusted rates could not be calculated as there were limited population data in this respect on the study area. This also made it difficult to compare data with other studies. Finally the use of pin hole VA in the place of objective refraction may have overestimated the prevalence of cataract VI among the study population.
In conclusion, cataract VI among the rural Akinyele population is high. There is the need to establish and maintain an appropriate cost effective eye care programme using the VISION 2020 strategy if the backlog of visually disabling cataract is to be taken care of.
References
Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, Pokharel GP et al. Global data on visual impairment in the year 2002. Bull World Health Organ 2004; 82: 844–851.
Foster A, Johnson G . Blindness in the developing world. Br J Ophthalmol 1993; 77: 398–399.
Thylefors B . A global initiative for the elimination of avoidable blindness. Indian J Ophthalmol 1998; 46: 129–130.
Ho VH, Schwab IR . Social economic development in the prevention of global blindness. Br J Ophthalmol 2001; 85: 653–657.
Lewallen S, Courtright P . Blindness in Africa: present situation and future needs. Br J Ophthalmol 2001; 85: 897–903.
World Health Organization. Global Initiative for the Elimination of Avoidable Blindness. An Internal Consultation. WHO/PBL/97.61. WHO: Geneva, 1997.
Adeoti CO . Prevalence and causes of blindness in a tropical African population. West Afr J Med 2004; 23: 249–252.
Adeoye A . Survey of blindness in rural communities of Southern western Nigeria. Trop Med Int Health 1996; 1: 672–676.
Oluleye TS . Cataract blindness and barriers to cataract surgical intervention in three rural communities of Oyo State, Nigeria. Niger J Med 2004; 13: 156–160.
Onakpoya OH, Adeoye AO, Akinsola FB, Adegbehingbe BO . Prevalence of blindness and visual impairment in Atakunmosa West Local Government area of southwestern Nigeria. Tanzan Health Res Bull 2007; 9: 126–131.
Adegbehingbe BO, Fajemilehin BR, Ojofeitimi EO, Bisiriyu LA . Blindness and visual impairment among the elderly in Ife Ijesha zone of Osun State, Nigeria. Indian J Ophthalmol 2006; 54: 59–62.
Patrick-Ferife G, Ashaye AO, Quereshi BM . Blindness and low vision in adults in Ozoro, a rural community in Delta State, Nigeria. Niger J Med 2005; 14: 390–395.
Rabiu MM . Cataract blindness and barrier to uptake of cataract surgery in a rural community of nothern Nigeria. Br J Opthalmol 2001; 85: 776–780.
Faal H, Minassian D, Sowa S, Foster A . National survey of blindness and low vision in The Gambia: results. Br J Ophthalmol 1989; 73: 82–87.
Melese M, Alemayehu W, Bayu S, Girma T, Hailesellasie T, Khandekar R et al. Low vision and blindness in adults in Gurage zone, central Ethiopia. Br J Ophthalmol 2003; 87: 677–680.
Oye JE, Kuper H . Prevalence and causes of blindness and visual impairment in Limber urban area, South West Province Cameroon. Br J Ophthalmol 2007; 91: 1435–1439.
World Health Organization. Rapid Assessment of Cataract Surgical Services. WHO/PBL/01.84. WHO: Geneva, 2001.
Klein BE, Klein R, Moss SE . Incident cataract surgery: the Beaver Dam Eye Study. Ophthalmology 1997; 104: 573–580.
Nigerian Population Commission 1991 Census report.
Thylefors B, Chylack Jr LT, Konyama K, Sasaki K, Sperduto R, Taylor HR et al. A Simplified Cataract Grading System—The WHO Cataract Grading Group WHO/PBD. WHO: Geneva, Switzerland, 1997.
World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 10th revision. Current version. Version for 2003. Chapter VII.H54. Blindness and low vision. WHO: Genova, 2003.
Li L, Guan H, Xun P, Zhou J, Gu H . Prevalence and causes of visual impairment among the elderly in Nantong, China. Eye 2008; 22 (8): 1069–1075.
Garap JN, Sheeladevi S, Brian G, Shamanna BR, Nirmalan PK, William C . Cataract and its surgery in Papua New Guinea. Clin Experiment Ophthalmol 2006; 34: 880–885.
Jadoon Z, Shah SP, Bourne R, Dineen B, Khan MA, Gilbert A et al. Cataract prevalence, cataract surgical coverage and the barriers to uptake of cataract surgical services in Pakistan: the Pakistan National Blindness and visual impairment survey. Br J Ophthalmol 2007; 91: 1269–1273.
Nirmalan PK, Thulasiraj RD, Maneksha V, Rahmathallah R, Ramakrishnan R, Padmavathi A . A population based eye survey of older adults in Tirunelveli district in South India: blindness, cataract surgery and visual outcomes. Br J Ophthalmol 2002; 86: 505–512.
Li S, Xu J, He M, Wu K, Munoz SR, Ellwein LB . A survey of blindness and cataract surgery in Douman County China. Ophthalmology 1999; 106: 1602–1608.
Chua BE, Mitchell P, Cumming RG . Effect of cataract type and location on visual function: the Blue Mountains Eye Study. Eye 2004; 18: 765–772.
Acknowledgements
We thank the Authority of Akinyele Local Government Area of Oyo state, Nigeria for providing the logistic support that facilitated this survey.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Komolafe, O., Ashaye, A., Ajayi, B. et al. Visual impairment from age-related cataract among an indigenous African population. Eye 24, 53–58 (2010). https://doi.org/10.1038/eye.2009.38
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.38