Abstract
The primary purpose of this study was to explore the short-term efficacy of different cisplatin and fluorouracil-based chemotherapy regimens in the treatment of patients with esophagogastric junctional adenocarcinoma (EGJA) using a network meta-analysis (NMA). Randomized controlled trials (RCTs) related to chemotherapy regimens based on cisplatin and fluorouracil for EGJA were included from the PubMed, EMBASE and Cochrane Library electronic databases (from inception to June 2016). Direct and indirect evidence were combined to calculate the pooled odds ratio (OR) and its 95% confidence interval (95% CI) as well as to draw the surface under the cumulative ranking (SUCRA) curves. This NMA finally enrolled ten eligible RCTs with the following five regimens: cisplatin plus fluorouracil (cisplatin+fluorouracil), cisplatin+fluorouracil-based chemotherapy (cisplatin+fluorouracil+docetaxel/epirubicin/irinotecan), fluorouracil-based chemotherapy (fluorouracil+docetaxel/doxorubicin/methotrexate/irinotecan), cisplatin-based chemotherapy (cisplatin+docetaxel/epirubicin/irinotecan/capecitabine/s-1) and other drug-based chemotherapy (docetaxel/irinotecan/capecitabine). These results revealed that compared with a cisplatin+ fluorouracil-based chemotherapy regimen, the fluorouracil-based chemotherapy regimen had a lower overall response rate (ORR) and partial response (PR) for EGJA patients (ORR: OR=0.43, 95% CI=0.22–0.86; PR: OR=0.46, 95% CI=0.23–0.91). Cluster analyses suggested that the cisplatin+fluorouracil-based chemotherapy regimen had the best short-term efficacy for EGJA in terms of the complete response (CR), PR, ORR, stable disease (SD) and progression disease (PD). Our results indicated that cisplatin+fluorouracil-based chemotherapy regimens may have the best short-term efficacy in the treatment of EGJA.
Similar content being viewed by others
Introduction
Gastric carcinoma and esophageal carcinoma are two of the most common malignancies around the world.1 The esophagogastric junction refers to the border between the distal esophagus and proximal stomach.2 Esophagogastric junctional adenocarcinoma (EGJA) describes tumors with a center within 5.0 cm proximal or distal from the cardia, which is a rare but often lethal situation and had become a very serious public health problem in recent decades.3, 4 Several studies have reported that the incidence of EGJA has rapidly increased since the early 1970s in many regions worldwide.5, 6 Most EGJA patients are diagnosed at the regional or distant stage, presenting with 12% and 2% overall 5-year survival rates, respectively.4 Current treatment modalities for EGJA based on the results of major clinical trials were evaluated in a report on surgery, perioperative chemotherapy, perioperative chemoradiotherapy and systemic chemotherapy.7 However, surgery has limitations of low resectability and a high risk of distant metastasis for the treatment of advanced EGJA patients, who are often advised to undergo systemic chemotherapy.8
Currently, the available chemotherapeutic drugs for patients with EGJA include cisplatin, fluorouracil, oxaliplatin, irinotecan and taxane.9 Cisplatin, the first discovered platinum-based compound, which has been one of the most commonly used chemotherapy drugs for treating several human cancers, such as lung, ovarian, head and neck, and breast cancers.10, 11, 12, 13 Regarding the therapeutic resistance and side effects, combination chemotherapy regimens based on cisplatin have become novel therapeutic strategies for treating many human cancers.14 Fluorouracil (also referred to as 5-fluorouracil), which is a mainstay medication of chemotherapy,15 is a structural analog of thymine that blocks the enzyme thymidylate synthetase to depress the formation of DNA.16 Fluorouracil has been one of the most widely used chemotherapy drugs in treating solid organ tumors, including tumors of the colon, rectum, breast, pancreas, and stomach; however, its common side effects are gastrointestinal symptoms, alopecia, cardiotoxicity, and neutropenia.17
As two of the most widely applied chemotherapeutic drugs, cisplatin and fluorouracil may play a very important role in treating EGJA patients. Several studies have focused on the chemotherapy regimens based on cisplatin and fluorouracil for EGJA. However, the chemotherapy regimen based on cisplatin and fluorouracil that may have the best short-term efficacy in treating EGJA remains unclear. Therefore, in the present study, different chemotherapy regimens based on cisplatin and fluorouracil for EGJA patients were evaluated from relevant databases to compare their short-term efficacy by performing this network meta-analysis and to calculate the current clinical data for screening more short-term effective chemotherapy regimens.
Materials and methods
Literature search
The PubMed, EMBASE and Cochrane Library electronic databases were comprehensively searched from inception to June 2016. The following search terms were searched in the combination of medical subject headings (MeSH) terms and the following free words: esophagogastric junctional adenocarcinoma (EGJA), chemotherapy, pharmacotherapy, cisplatin, fluorouracil and so on. In addition, we also manually searched other potential and relevant references.
Study selection
Studies were enrolled into our analysis if they met the following inclusion criteria: (1) the study design was a randomized controlled trial (RCT); (2) different chemotherapeutic interventions were included; (3) EGJA patients were histologically confirmed with at least one measurable lesion according to the version 1.0 Response Evaluation Criteria in Solid Tumors (RECIST);18 and (4) studies containing the overall remission rate (ORR), complete response (CR), partial response (PR), stable disease (SD) or progressive disease (PD). The exclusion criteria were as follows: (1) patients who received surgery or radiotherapy and (2) studies with insufficient data, non-RCTs or duplicated publications.
Data extraction and quality assessment
All data from eligible RCTs were independently extracted by two investigators using a standardized form, and any disagreements were resolved by discussions with other investigators. The quality of enrolled RCTs was evaluated by two or more investigators according to the Physiotherapy Evidence Database (PEDro) scale.19 The total score is 11 points, and the study was judged as high quality if its scores were ⩾6 points; 4–5 points were generally considered to be fair quality and scores <4 points were considered low quality.20
Statistical analysis
Traditional pairwise meta-analyses were performed to analyze the comparisons in enrolled studies that directly compared five chemotherapy regimens. The odds ratios (ORs) and 95% confidence intervals (CIs) were calculated by a random effects model, and the Z-test was performed to detect the significance of the pooled effect size.21 The Cochran’s Q and I2 (ranging from 0 to 100%) statistics were performed to determine and quantify statistical heterogeneity among the enrolled studies.22, 23 Since a model should take the relevant source of error into consideration, thus, when studies are gathered from the published literature, the random-effects model is generally more reasonable;24 therefore, the random-effects model was adopted in this study. We used STATA 13.1 (Stata Corp, College Station, TX, USA) software to perform a network analysis and create network relation plots, with the nodes indicating interventions, node sizes representing sample sizes and thickness of lines referring to the accuracy of the effect size of comparison between two studies (the inverse of variance). The node-splitting method was performed in our study to evaluate the consistency between direct and indirect evidence, and the consistency or inconsistency model was result based.25 According to the above models, we calculated the OR and 95% CI of efficacy outcomes among chemotherapies. A surface under the cumulative ranking (SUCRA) curve analysis was used to compare the SUCRA value of outcomes and determined the efficacy ranks of the chemotherapies. Higher SUCRA values indicated better treatments and vice versa.25 Cluster analyses were performed to compare the efficacy of the chemotherapy regimens for advanced EGJA, and different chemotherapy regimens were clustered according to the similarity of two variables. Then, their effectiveness was determined based on the performance.26 A comparison-adjusted funnel plot was used to evaluate the small-study effect, which considered the difference of the summary effect for each set of studies (measure of precision vs estimated treatment effect).27 STATA 13.1 (Stata Corp) was used to perform for all calculations in this study.
Results
Baseline characteristics of included studies
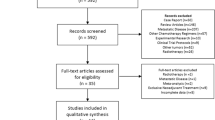
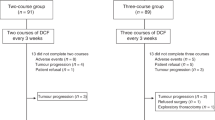
A total of 1966 articles on the treatment of five chemotherapy regimens for EGJA were initially reviewed. After excluding duplicate studies (n=470), letters or reviews (n=62), non-human studies (n=70) and studies unrelated to research topics (n=586), 778 remaining studies were evaluated with full-text assessment. Further exclusion was performed in the remaining studies with 156 neoadjuvant chemoradiotherapy studies, 275 surgery-related articles, 112 studies related to radiotherapy, 221 studies that were unrelated to the outcomes in this study, and four that had unavailable or missing data. Finally, 10 RCTs (3506 individuals), published between 1997 and 2012, remained in this meta-analysis.28, 29, 30, 31, 32, 33, 34, 35, 36, 37 Among all enrolled individuals, 732 were treated with the cisplatin plus fluorouracil (cisplatin+fluorouracil) chemotherapy regimen; 763 received cisplatin+fluorouracil-based (cisplatin+fluorouracil+docetaxel/epirubicin/irinotecan); 336 were treated with fluorouracil-based (fluorouracil+docetaxel/epirubicin/irinotecan); 1577 were given cisplatin-based (cisplatin+docetaxel/epirubicin/irinotecan/capecitabine/s-1); and the remaining 98 were treated with other drugs (docetaxel/irinotecan/capecitabine). Subjects in the study were all Caucasians. All included studies were two-arm trials with 10 comparisons. The baseline characteristics of included studies are shown in Supplementary Appendix Table 1, and the literature assessment using PEDro scale is displayed in Figure 1.
Pairwise meta-analysis for short-term efficacy of five chemotherapy regimens in the treatment of EGJA
A random-effects model was used to perform direct pairwise matching, and the results of the short-term efficacy differences of five chemotherapy regimens for EGJA are shown in Table 1. The results suggested that the cisplatin+fluorouracil chemotherapy regimens had a worse short-term efficacy in the ORR and PR compared with cisplatin+fluorouracil-based chemotherapy regimens (OR=0.59, 95% CI=0.39~0.89; OR=0.59, 95% CI=0.39~0.90, respectively). The cisplatin+fluorouracil-based chemotherapy regimens had better short-term efficacy in the ORR and PR than fluorouracil-based chemotherapy regimens (OR=3.03, 95% CI=1.67~5.48; OR=2.62, 95% CI=1.42–4.82, respectively). EGJA patients who received cisplatin+fluorouracil-based chemotherapy regimens had a better ORR than those who received other drugs (OR=2.45, 95% CI=1.06–5.66). However, the short-term efficacy in PD of EGJA patients treated with the cisplatin and fluorouracil chemotherapy regimen was better than for the cisplatin and fluorouracil-based chemotherapy regimen (OR=1.74, 95% CI=1.09–2.76), while the cisplatin and fluorouracil-based chemotherapy regimens performed worse than the fluorouracil-based chemotherapy regimen (OR=0.47, 95% CI=0.26–0.88).
Network evidence of five chemotherapy regimens in the treatment of EGJA
In this NMA, five chemotherapy regimens were evaluated, including cisplatin+fluorouracil, cisplatin+fluorouracil-based chemotherapy, fluorouracil-based chemotherapy, cisplatin-based chemotherapy and other drugs. Regarding the ORR, most EGJA patients were treated with the cisplatin-based chemotherapy regimen, and direct comparison between cisplatin+fluorouracil chemotherapy and cisplatin-based chemotherapy and between cisplatin+fluorouracil-based chemotherapy and cisplatin-based chemotherapy was observed in most studies (Figure 2). There were relatively more EGJA patients treated with cisplatin+fluorouracil-based and cisplatin-based chemotherapies in terms of the CR and PR, and the most direct comparisons of the cisplatin+fluorouracil chemotherapy regimen and cisplatin-based chemotherapy regimen are shown in these included studies (Figure 2). For the SD, cisplatin and fluorouracil-based chemotherapies were used to treat more EGJA patients, and most of these included studies explored the comparison between cisplatin+fluorouracil and cisplatin+fluorouracil-based chemotherapy (Supplementary Figure 1). Regarding the PD, more EGJA patients were treated with cisplatin+fluorouracil-based and cisplatin-based chemotherapy regimens, and most studies compared cisplatin-based chemotherapies with cisplatin+fluorouracil-based chemotherapies and fluorouracil-based chemotherapies, respectively (Supplementary Figure 1).
Inconsistency tests of the ORR, CR, PR, SD and PD among all included studies
The inconsistency tests of the ORR, CR, PR, SD and PD were performed by the node-splitting method. Consistency was shown in the direct and indirect evidence of all these outcomes and thus the consistency model was selected (both P>0.05; Table 2).
Comparison of the ORR in EGJA patients treated with five chemotherapy regimens
All enrolled studies reported the differences in the ORR for EGJA patients treated with five chemotherapies. Patients who received the fluorouracil-based chemotherapy regimen had a worse ORR than those treated with the cisplatin+fluorouracil-based chemotherapy regimen (OR=0.43, 95% CI=0.22–0.86; Table 3, Figure 3). Consequently, the cisplatin+fluorouracil-based chemotherapy regimen may be the best regimen of the five chemotherapy regimens for EGJA.
Forest plots of the comparisons for the ORR, CR and PR of EGJA patients treated with five chemotherapy regimens. A, cisplatin plus fluorouracil; B, cisplatin plus fluorouracil-based chemotherapy; C, fluorouracil-based chemotherapy; CR, complete response; D, cisplatin-based chemotherapy; E, other drugs [docetaxel/irinotecan/capecitabine]; ORR, overall remission rate; PR, partial response.
Comparison of the CR and PR in EGJA patients treated with five chemotherapy regimens
Nine of 10 studies focused on the CR differences for patients treated with 5 chemotherapy regimens for EGJA. The results demonstrated that the cisplatin-based chemotherapy regimen was better than the fluorouracil-based chemotherapy regimen in achieving a CR for EGJA patients (OR=2.70, 95% CI=1.11~6.56) (Table 3, Figure 3). The PR differences for the five chemotherapy regimens for EGJA were investigated in nine of the included studies. A worse PR was observed in patients who received fluorouracil-based chemotherapy compared to cisplatin+fluorouracil-based chemotherapy (OR=0.46, 95% CI=0.23–0.91; Table 3, Figure 3).
Comparison of PD and SD in EGJA patients treated with five chemotherapy regimens
Nine out of 10 studies explored the PD differences of patients treated with 5 chemotherapy regimens for EGJA, while 7 of the included studies compared the SD differences. The results revealed that there was no evidence of PD or SD differences in the pairwise comparison of all the chemotherapy regimens (Table 3, Supplementary Figure 2).
Cumulative probability ranking of five chemotherapy regimens in treating EGJA
As shown in Table 4 and Supplementary Figure 3, regarding the PR, ORR, SD and PD, the SUCRA values of five chemotherapy regimens revealed that the cisplatin+fluorouracil-based chemotherapy regimen ranked the highest (PR: 88.2%; ORR: 89.2%; SD: 76.0%; PD: 93.3%). As for the CR, the SUCRA values of cisplatin-based chemotherapy (83.9%) and cisplatin+fluorouracil-based chemotherapy (71.4%) were higher than for other chemotherapy regimens. Other drugs had the lowest SUCRA values in terms of the CR and PD (CR: 11.7%; PD: 25.2%), and fluorouracil-based chemotherapy regimens had the lowest SUCRA values for the PR and ORR (PR: 18.5%; ORR: 15.7%). In addition, the SUCRA value of cisplatin-based chemotherapy had the lowest SD (30.6%).
Cluster analyses and publication bias assessment of five chemotherapy regimens in the treatment of EGJA
In this study, cluster analyses of the CR, PR, ORR, SD and PD demonstrated that the cisplatin+fluorouracil-based chemotherapy regimen had the best efficacy in the treatment of EGJA, which was followed by the cisplatin-based chemotherapy regimen (Figure 4). Therefore, cisplatin+fluorouracil-based chemotherapy may be the best regimen for EGJA patients. No evidence of publication bias for these outcomes was discovered in this NMA (Supplementary Figure 4).
Cluster analyses for the CR, PR, ORR, PD and SD of EGJA patients treated with five chemotherapy regimens. A, cisplatin plus fluorouracil; B, cisplatin plus fluorouracil-based chemotherapy; C, fluorouracil-based chemotherapy; CR, complete response; D, cisplatin-based chemotherapy; E, other drugs [docetaxel/irinotecan/capecitabine]; ORR, overall remission rate; PD, progressive disease; PR, partial response; SD, stable disease.
Discussion
This network meta-analysis compared the short-term efficacy of 5 chemotherapy regimens with evaluation based on 10 studies with a total of 3506 EGJA patients. The treatment regimens included cisplatin+fluorouracil, cisplatin+fluorouracil-based chemotherapy, fluorouracil-based chemotherapy, cisplatin-based chemotherapy and other drugs (docetaxel/irinotecan/capecitabine). Our results from cluster analyses for the SUCRA values showed that cisplatin+fluorouracil-based chemotherapy regimens had the highest PR, ORR, SD and PD and the second highest CR, which demonstrated that cisplatin+fluorouracil-based chemotherapy may have the best short-term efficacy for treating EGJA patients.
Recently, a meta-analysis compared triple therapy regimens with fluorouracil+cisplatin and fluorouracil+anthracycline doublets, which supported the benefits of triple therapy regimens in patients with advanced EGJA due to the significant OS in triple therapy regimens.38 Despite this, the toxicity also increased for patients who received fluorouracil, cisplatin and docetaxel, and there was no difference in the treatment-related mortality rate between the double and triple therapy regimens.39 In addressing this result, our finding demonstrated that the cisplatin+fluorouracil-based chemotherapy regimen had an encouraging efficacy profile with an elevated ORR compared with cisplatin- and fluorouracil-based chemotherapy regimens as well as other drugs. Moreover, the SUCRA curves showed that the cisplatin+fluorouracil-based chemotherapy regimen ranked at the top among the five chemotherapy regimens, while other drugs had the lowest efficacy benefit in terms of the PR, ORR, SD, CR and PD.
Two previously published clinical trials suggested that preoperative treatment with the combination of cisplatin+fluorouracil+docetaxel was associated with an ORR of 64.3% and was associated with favorable outcomes in esophageal squamous cell carcinoma or advanced OG adenocarcinoma.40, 41 Docetaxel, a semi-synthetic taxoid, in combination with cisplatin, has shown encouraging activity with an objective response rate ranging from 31 to 56%.27, 28 After the additional use of docetaxel in combination with cisplatin and fluorouracil, the OS for patients with advanced EGJA achieved a significant improvement with an elevated ORR of 37% compared with the ORR of 25% using cisplatin and fluorouracil.42 A possible explanation could be that the rationale for these individualized regimens is based on the theory of oncogene dependence, which implies that single or slight abnormalities may be key triggers for cancer cell growth and maintenance. It is possible that the most effective therapy would be a multi-tyrosine kinase inhibitor or dual-targeted approach.43 The combined use of cisplatin, fluorouracil and docetaxel significantly prolonged the maintenance of the Karnofsky performance status and presented with better results in terms of the appetite and weight-loss analyses in advanced gastric or gastroesophageal cancer treatment, notably in the study by Ajani et al.44 In Europe and in USA, cisplatin and fluorouracil-based chemotherapy regimens with three drugs, including docetaxel or epirubicin, are widely applied, first-line chemotherapy combination regimens for treating advanced EGJA.45
Our study has some strengths. This network meta-analysis compared all major chemotherapy regimens and assessed the end points. As one of the striking aspects of our study, the assessment of the ORR, PR, CR, PD and SD provided a comprehensive and reliable result for chemotherapy. Furthermore, this network meta-analysis also indirectly compared therapies when head-to-head trials were not available, and it demonstrated more precise estimates via direct and indirect comparisons. In addition, both the direct and indirect evidence were consistent, which contributed to the credibility of our results. Moreover, the application of SUCRA double confirmed the major results of our analysis, which enhanced its reliability and research value. In addition, there were limitations with the analysis that should be mentioned. First, in the clinical trials enrolled in the current network meta-analysis, observations were grouped by the initial randomized drug (because it is least likely of all variables to be biased). However, there might be differences when considering drugs in different subjects, which affect our results. In addition, only 10 studies were included in the current network meta-analysis, and our results might have limited generalizability because the included studies were mostly conducted in Western countries. The failure to detect any significant differences between the cisplatin and fluorouracil chemotherapy strategy and the other four chemotherapy strategies in terms of the endpoints, ORR, PR, CR, PD and SD may be due to the limited number of included studies, and this may also help explain the current disputed results with previous studies. However, all included studies had high PEDro scales; therefore, the results of our network meta-analysis were credible and reliable. Furthermore, our study has established a new direction for future studies because rigorous and precious studies or network meta-regression analyses are required to fully evaluate the different chemotherapy regimens.
This network meta-analysis suggested that the cisplatin+fluorouracil-based chemotherapy strategy may be the optimal treatment for advanced EGJA. Although our updated synthesis of existing data has provided new insight for the chemotherapy treatment for advanced EGJA, future trials are needed to confirm or validate the current findings.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Liu K, Yang K, Zhang W, Chen X, Chen X, Zhang B et al. Changes of esophagogastric junctional adenocarcinoma and gastroesophageal reflux disease among surgical patients during 1988-2012: a single-institution, high-volume experience in China. Ann Surg 2016; 263: 88–95.
Rusch VW . Are cancers of the esophagus, gastroesophageal junction, and cardia one disease, two, or several? Semin Oncol 2004; 31: 444–449.
Tercioti-Junior V, Lopes LR, Coelho-Neto Jde S, Carvalheira JB, Andreollo NA . Esophagogastric junction adenocarcinoma: multivariate analyses of surgical morbi-mortality and adjuvant therapy. Arq Bras Cir Dig 2012; 25: 229–234.
Buas MF, Vaughan TL . Epidemiology and risk factors for gastroesophageal junction tumors: understanding the rising incidence of this disease. Semin Radiat Oncol 2013; 23: 3–9.
Blot WJ, Devesa SS, Kneller RW, Fraumeni JF Jr . Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA 1991; 265: 1287–1289.
Botterweck AA, Schouten LJ, Volovics A, Dorant E, van Den Brandt PA . Trends in incidence of adenocarcinoma of the oesophagus and gastric cardia in ten European countries. Int J Epidemiol 2000; 29: 645–654.
Hasegawa S, Yoshikawa T . Adenocarcinoma of the esophagogastric junction: incidence, characteristics, and treatment strategies. Gastric Cancer 2010; 13: 63–73.
Hayashi K, Ando N, Watanabe H, Ide H, Nagai K, Aoyama N et al. Phase II evaluation of protracted infusion of cisplatin and 5-fluorouracil in advanced squamous cell carcinoma of the esophagus: a Japan Esophageal Oncology Group (JEOG) Trial (JCOG9407). Jpn J Clin Oncol 2001; 31: 419–423.
Li YH, Qiu MZ, Xu JM, Sun GP, Lu HS, Liu YP et al. S-1 plus cisplatin versus fluorouracil plus cisplatin in advanced gastric or gastro-esophageal junction adenocarcinoma patients: a pilot study. Oncotarget 2015; 6: 35107–35115.
O'Grady S, Finn SP, Cuffe S, Richard DJ, O'Byrne KJ, Barr MP . The role of DNA repair pathways in cisplatin resistant lung cancer. Cancer Treat Rev 2014; 40: 1161–1170.
Casagrande N, Celegato M, Borghese C, Mongiat M, Colombatti A, Aldinucci D . Preclinical activity of the liposomal cisplatin lipoplatin in ovarian cancer. Clin Cancer Res 2014; 20: 5496–5506.
Roh JL, Kim EH, Park JY, Kim JW, Kwon M, Lee BH . Piperlongumine selectively kills cancer cells and increases cisplatin antitumor activity in head and neck cancer. Oncotarget 2014; 5: 9227–9238.
Zhang J, Wang Z, Hu X, Wang B, Wang L, Yang W et al. Cisplatin and gemcitabine as the first line therapy in metastatic triple negative breast cancer. Int J Cancer 2015; 136: 204–211.
Dasari S, Tchounwou PB . Cisplatin in cancer therapy: molecular mechanisms of action. Eur J Pharmacol 2014; 740: 364–378.
Rosmarin D, Palles C, Church D, Domingo E, Jones A, Johnstone E et al. Genetic markers of toxicity from capecitabine and other fluorouracil-based regimens: investigation in the QUASAR2 study, systematic review, and meta-analysis. J Clin Oncol 2014; 32: 1031–1039.
Joag MG, Sise A, Murillo JC, Sayed-Ahmed IO, Wong JR, Mercado C et al. Topical 5-Fluorouracil 1% as Primary Treatment for Ocular Surface Squamous Neoplasia. Ophthalmology 2016; 123: 1442–1448.
Ha JH, Hwang DY, Yu J, Park DH, Ryu SH . Onset of manic episode during chemotherapy with 5-fluorouracil. Psychiatry Investig 2011; 8: 71–73.
Bamal R, Chintamani, Tandon M, Mittal MK, Saxena S . Evaluation and validation of neo-adjuvant response index (NRI) and it's correlation with various predictive biomarkers and RECIST in locally advanced breast cancer. Indian J Surg Oncol 2014; 5: 171–177.
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M . Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther 2003; 83: 713–721.
Ferreira LL, Valenti VE, Vanderlei LC . Chest physiotherapy on intracranial pressure of critically ill patients admitted to the intensive care unit: a systematic review. Rev Bras Ter Intensiva 2013; 2: 327–333.
Chen H, Manning AK, Dupuis J . A method of moments estimator for random effect multivariate meta-analysis. Biometrics 2012; 68: 1278–1284.
Jackson D, White IR, Riley RD . Quantifying the impact of between-study heterogeneity in multivariate meta-analyses. Stat Med 2012; 31: 3805–3820.
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L . Comparison of two methods to detect publication bias in meta-analysis. JAMA 2006; 295: 676–680.
Higgins JP, Green S . Cochrane Handbook for Systematic Reviews of Interventions. Wiley-Blackwell: Hoboken, NJ, USA, 2010; 1: 97–111.
Zhu GQ, Shi KQ, Huang S, Wang LR, Lin YQ, Huang GQ et al. Systematic review with network meta-analysis: the comparative effectiveness and safety of interventions in patients with overt hepatic encephalopathy. Aliment Pharmacol Ther 2015; 41: 624–635.
Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G . Graphical tools for network meta-analysis in STATA. PLoS ONE 2013; 8: e76654.
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L, Moreno SG . Assessing publication bias in meta-analyses in the presence of between-study heterogeneity. J R Stat Soc 2010; 173: 575–591.
Roy A, Cunningham D, Hawkins R, Sorbye H, Adenis A, Barcelo JR et al. Docetaxel combined with irinotecan or 5-fluorouracil in patients with advanced oesophago-gastric cancer: a randomised phase II study. Br J Cancer 2012; 107: 435–441.
Tebbutt NC, Cummins MM, Sourjina T, Strickland A, Van Hazel G, Ganju V et al. Randomised, non-comparative phase II study of weekly docetaxel with cisplatin and 5-fluorouracil or with capecitabine in oesophagogastric cancer: the AGITG ATTAX trial. Br J Cancer 2010; 102: 475–481.
Ajani JA, Rodriguez W, Bodoky G, Moiseyenko V, Lichinitser M, Gorbunova V et al. Multicenter phase III comparison of cisplatin/S-1 with cisplatin/infusional fluorouracil in advanced gastric or gastroesophageal adenocarcinoma study: the FLAGS trial. J Clin Oncol 2010; 28: 1547–1553.
Cunningham D, Starling N, Rao S, Iveson T, Nicolson M, Coxon F et al. Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med 2008; 358: 36–46.
Ajani JA . Optimizing docetaxel chemotherapy in patients with cancer of the gastric and gastroesophageal junction: evolution of the docetaxel, cisplatin, and 5-fluorouracil regimen. Cancer 2008; 113: 945–955.
Trumper M, Ross PJ, Cunningham D, Norman AR, Hawkins R, Seymour M et al. Efficacy and tolerability of chemotherapy in elderly patients with advanced oesophago-gastric cancer: A pooled analysis of three clinical trials. Eur J Cancer 2006; 42: 827–834.
Sumpter K, Harper-Wynne C, Cunningham D, Rao S, Tebbutt N, Norman AR et al. Report of two protocol planned interim analyses in a randomised multicentre phase III study comparing capecitabine with fluorouracil and oxaliplatin with cisplatin in patients with advanced oesophagogastric cancer receiving ECF. Br J Cancer 2005; 92: 1976–1983.
Ajani JA, Fodor MB, Tjulandin SA, Moiseyenko VM, Chao Y, Cabral Filho S et al. Phase II multi-institutional randomized trial of docetaxel plus cisplatin with or without fluorouracil in patients with untreated, advanced gastric, or gastroesophageal adenocarcinoma. J Clin Oncol 2005; 23: 5660–5667.
Pozzo C, Barone C, Szanto J, Padi E, Peschel C, Bukki J et al. Irinotecan in combination with 5-fluorouracil and folinic acid or with cisplatin in patients with advanced gastric or esophageal-gastric junction adenocarcinoma: results of a randomized phase II study. Ann Oncol 2004; 15: 1773–1781.
Webb A, Cunningham D, Scarffe JH, Harper P, Norman A, Joffe JK et al. Randomized trial comparing epirubicin, cisplatin, and fluorouracil versus fluorouracil, doxorubicin, and methotrexate in advanced esophagogastric cancer. J Clin Oncol 1997; 15: 261–267.
Kang YK, Kang WK, Shin DB, Chen J, Xiong J, Wang J et al. Capecitabine/cisplatin versus 5-fluorouracil/cisplatin as first-line therapy in patients with advanced gastric cancer: a randomised phase III noninferiority trial. Ann Oncol 2009; 20: 666–673.
Rosati G, Ferrara D, Manzione L . New perspectives in the treatment of advanced or metastatic gastric cancer. World J Gastroenterol 2009; 15: 2689–2692.
Hara H, Tahara M, Daiko H, Kato K, Igaki H, Kadowaki S et al. Phase II feasibility study of preoperative chemotherapy with docetaxel, cisplatin, and fluorouracil for esophageal squamous cell carcinoma. Cancer Sci 2013; 104: 1455–1460.
Lorenzen S, Thuss-Patience P, Al-Batran SE, Lordick F, Haller B, Schuster T et al. Impact of pathologic complete response on disease-free survival in patients with esophagogastric adenocarcinoma receiving preoperative docetaxel-based chemotherapy. Ann Oncol 2013; 24: 2068–2073.
Van Cutsem E, Moiseyenko VM, Tjulandin S, Majlis A, Constenla M, Boni C et al. Phase III study of docetaxel and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as first-line therapy for advanced gastric cancer: a report of the V325 Study Group. J Clin Oncol 2006; 24: 4991–4997.
Paterson AL, Shannon NB, Lao-Sirieix P, Ong CA, Peters CJ, O'Donovan M et al. A systematic approach to therapeutic target selection in oesophago-gastric cancer. Gut 2013; 62: 1415–1424.
Ajani JA, Moiseyenko VM, Tjulandin S, Majlis A, Constenla M, Boni C et al. Clinical benefit with docetaxel plus fluorouracil and cisplatin compared with cisplatin and fluorouracil in a phase III trial of advanced gastric or gastroesophageal cancer adenocarcinoma: the V-325 Study Group. J Clin Oncol 2007; 25: 3205–3209.
Quintero-Aldana G, Jorge M, Grande C, Salgado M, Gallardo E, Varela S et al. Phase II study of first-line biweekly docetaxel and cisplatin combination chemotherapy in advanced gastric cancer. Cancer Chemother Pharmacol 2015; 76: 731–737.
Acknowledgements
This study was supported by a grant from the Project of Science and Technology in Beijing (No. Z151100002615031). We thank the reviewers for their helpful comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Experimental & Molecular Medicine website
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Wang, C., Song, DJ., Xu, ZL. et al. A network meta-analysis of the short-term efficacy of five chemotherapy regimens based on cisplatin and fluorouracil for esophagogastric junctional adenocarcinoma. Exp Mol Med 49, e383 (2017). https://doi.org/10.1038/emm.2017.170
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/emm.2017.170