Abstract
Background/Objectives:
Gestational diabetes mellitus (GDM) risk factors are well established for Caucasians, but not for Asians. We hypothesized that nutrient intakes, plasma adipokines and/or gestational hormones might be linked to GDM development among pregnant Korean women. This study sought to identify new risk factors for GDM and adverse pregnancy outcomes according to body weight at prepregnancy.
Subjects/Methods:
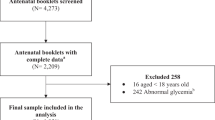
All subjects were pregnant women visiting the Cheil General Hospital and Women’s Healthcare Center between June 2006 and March 2009. Non-GDM (n=531) and GDM (n=215) participants were divided into normal-weight and overweight groups according to prepregnancy body mass index (BMI) above or below 23 kg/m2 at 24–28th week of gestation. At that time, glucose tolerance, insulin resistance as homeostatic model assessment for insulin resistance, insulin secretory capacity as homeostatic model assessment for β-cell function, anthropometric measurement, nutrient intakes, and plasma levels of adipokines and gestational hormones were determined.
Results:
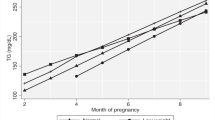
GDM women gained more weight in early pregnancy than non-GDM among normal-weight women. GDM was mainly associated with increased insulin resistance in overweight women and decreased insulin secretory capacity in normal-weight women. Plasma visfatin and adiponectin were lower and progesterone levels higher in GDM than non-GDM independent of BMI while plasma resistin levels were higher in non-GDM, but not GDM, overweight women. Energy and saturated fat intakes were higher in GDM independent of body weight, whereas taurine intakes were lower in GDM than non-GDM only in normal-weight women.
Conclusions:
Low visfatin and adiponectin and high progesterone levels in the circulation and high energy and saturated fat intakes were common risk factors for GDM and pregnancy outcome such as large for gestational age. Daily reference intakes for energy and fat during pregnancy need to be re-evaluated according to prepregnancy BMI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Hedderson MM, Williams MA, Holt VL, Weiss NS, Ferrara A . Body mass index and weight gain prior to pregnancy and risk of gestational diabetes mellitus. Am J Obstet Gynecol 2008; 198: 409 e1-e7.
Coustan DR, Nelson C, Carpenter MW, Carr SR, Rotondo L, Widness JA . Maternal age and screening for gestational diabetes: a population based study. Obstet Gynecol 1989; 73: 557–561.
Park S, Park JE, Daily JW, Kim SH . Low gestational weight gain improves infant and maternal pregnancy outcomes in overweight and obese Korean women with gestational diabetes. Gynecol Endocrinol 2011; 27: 775–781.
Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 2009; 301: 2129–2140.
Volpe L, Di Cianni G, Lencioni C, Cuccuru I, Benzi L, Del Prato S . Gestational diabetes, inflammation, and late vascular disease. J Endocriol Invest 2007; 30: 873–879.
Donath MY, Böni-Schnetzler M, Ellingsgaard H, Ehses JA . Islet inflammation impairs the pancreatic beta-cell in type 2 diabetes. Physiology 2009; 24: 325–331.
Saddi-Rosa P, Oliveira DSV, Giuffrida FMA, Reis AF . Visfatin, glucose metabolism and vascular disease: a review of the evidence. Diabetol Metab Syndr 2010; 2: 21.
Hirose H, Yamamoto Y, Seino-Yoshihara Y, Kawabe H, Saito I . Serum high-molecular-weight Adiponectin as a marker for the evaluation and care of subjects with metabolic syndrome and related disorders. J Atheroscler Thromb 2010; 17: 1201–1211.
Carpenter MW, Coustan DR . Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol 1982; 144: 769–773.
Brănişteanu DD, Mathieu C . Progesterone in gestational diabetes mellitus: guilty or not guilty? Trends Endocrinol Metab 2003; 14: 54–56.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Committee of Dietary reference intake in Korean Nutrition Society. Dietary reference intake for Koreans. Korean Nutrition Society: Seoul, 2008.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363: 157–163.
Lee S, Choi S, Kim HJ, Chung YS, Lee KW, Lee HC et al. Cutoff values of surrogate measures of insulin resistance for metabolic syndrome in Korean non-diabetic adults. J Korean Med Sci 2006; 21: 695–700.
Salmenhaara M, Uusitalo L, Uusitalo U, Kronberg-kippilä C, Sinkko H, Ahonen S et al. Diet and weight gain characteristics of pregnant women with gestational diabetes. Eur J Clin Nutr 2010; 64: 1433–1440.
Arumugam R, Horowitz E, Lu J, Collier J, Ronnebaum S, Fleenor D et al. The interplay of prolactin and the glucocorticoids in the regulation of β-cell gene expression, fatty acid oxidation, and glucose-stimulated insulin secretion: implications for carbohydrate metabolism in pregnancy. Endocrinology 2008; 149: 5401–5414.
Park S, Kim DS, Daily JW, Kim SH . Serum prolactin concentrations determine whether they improve or impair β-cell function and insulin sensitivity in diabetic rats. Diabetes Metab Res Rev 2011; 27: 564–574.
de Kreutzenberg SV, Ceolotto G, Papparella I, Bortoluzzi A, Semplicini A, Dalla MC et al. Downregulation of the longevity-associated protein sirtuin 1 in insulin resistance and metabolic syndrome: potential biochemical mechanisms. Diabetes 2010; 59: 1006–1015.
Milne JC, Lambert PD, Schenk S, Carney DP, Smith JJ, Gagne DJ et al. Small molecule activators of SIRT1 as therapeutics for the treatment of type 2 diabetes. Nature 2007; 450: 712–716.
Qiao L, Shao J . SIRT1 regulates adiponectin gene expression through Foxo1-c/enhancer-binding protein α transcriptional complex. J Biol Chem 2006; 281: 39915–39924.
Ramachandran D, Roy U, Garg S, Ghosh S, Pathak S, Kolthur-Seetharam U . Sirt1 and mir-9 expression is regulated during glucose-stimulated insulin secretion in pancreatic β-islets. FEBS J 2011; 278: 1167–1174.
Revollo JR, Körner A, Mills KF, Satoh A, Wang T, Garten A et al. Nampt/PBEF/Visfatin regulates insulin secretion in beta cells as a systemic NAD biosynthetic enzyme. Cell Metab 2007; 6: 363–375.
Song Y, Manson JE, Tinker L, Howard BV, Kuller LH, Nathan L et al. Insulin sensitivity and insulin secretion determined by homeostasis model assessment and risk of diabetes in a multiethnic cohort of women: the Women's Health Initiative Observational Study. Diabetes Care 2007; 30: 1747–1752.
Thompson FE, Subar AF . Dietary assessment methodology. In: Coulston AM, Boushey CJ (eds). Nutrition in the Prevention and Treatment of Disease 2nd edn. Academic Press: San Diego, CA, USA, 2008.
Acknowledgements
This work was supported by grants from the Korean Research Foundation in Korea (R04-2008-000-10078-0) and the Korea Health 21 R&D Project, Ministry of Health and Welfare, Republic of Korea (Grant no. A102065-1011-1070100).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author contributions
The author’s responsibilities were as follows: SP contributed to designing the study, analyzing data and preparing the manuscript; M-YK, J-TW and J-HY analyzed data and reviewed the manuscript; YJK performed data analysis; JWD and Y-MP joined to prepare the manuscript; SHB and S-HK collected samples and data and prepared the manuscript.
Supplementary Information accompanies the paper on European Journal of Clinical Nutrition website
Supplementary information
Rights and permissions
About this article
Cite this article
Park, S., Kim, MY., Baik, S. et al. Gestational diabetes is associated with high energy and saturated fat intakes and with low plasma visfatin and adiponectin levels independent of prepregnancy BMI. Eur J Clin Nutr 67, 196–201 (2013). https://doi.org/10.1038/ejcn.2012.207
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2012.207
Keywords
This article is cited by
-
Refining the diagnosis of gestational diabetes mellitus: a systematic review and meta-analysis
Communications Medicine (2023)
-
Impact of gene polymorphism of glutathione S-transferase and ghrelin as a risk factor in Egyptian women with gestational diabetes mellitus
Egyptian Journal of Medical Human Genetics (2022)
-
How does antenatal lifestyle affect the risk for gestational diabetes mellitus? A secondary cohort analysis from the GeliS trial
European Journal of Clinical Nutrition (2022)
-
Association of aryl hydrocarbon receptor transactivating activity, a potential biomarker for persistent organic pollutants, with the risk of gestational diabetes mellitus
Scientific Reports (2021)
-
Maternal dietary patterns and risk of gestational diabetes mellitus in twin pregnancies: a longitudinal twin pregnancies birth cohort study
Nutrition Journal (2020)