Abstract
Thrombotic microangiopathy (TMA) is a systemic disease characterized by microangiopathic hemolytic anemia, thrombocytopenia and organ failure. Post-bone marrow transplant TMA (post-BMT TMA) is a life-threatening condition that has been reported to afflict between 0.5 and 63.6% of BMT patients. The incidence of post-BMT TMA is affected by evolving therapies such as conditioning regimens. The etiology of post-BMT TMA is thought to be multifactorial, including the effects of immunosuppressive agents, viral infections, TBI and GvHD. A growing body of evidence highlights the importance of complement system activation and endothelial damage in post-BMT TMA. Although plasmapheresis has commonly been used, its therapeutic rationale for the majority of post-BMT TMA cases is unclear in the absence of circulatory inhibitors. It has become possible to target complement activation with eculizumab, a drug that blocks the terminal complement pathway. Early studies have highlighted the importance of anti-complement therapies in treating post-BMT TMA. Moreover, finding complement gene mutations may identify patients at risk, but whether such patients benefit from prophylactic anti-complement therapies before BMT remains to be studied. This review focuses on diagnostic criteria, pathophysiology, treatment and renal outcomes of post-BMT TMA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Stavrou E, Lazarus HM . Thrombotic microangiopathy in haematopoietic cell transplantation: an update. Mediterr J Hematol Infect Dis 2010; 2: e2010033.
Rabinowe SN, Soiffer RJ, Tarbell NJ, Neuberg D, Freedman AS, Seifter J et al. Hemolytic-uremic syndrome following bone marrow transplantation in adults for hematologic malignancies. Blood 1991; 77: 1837–1844.
Noris M, Remuzzi G . Atypical hemolytic-uremic syndrome. N Engl J Med 2009; 361: 1676–1687.
Pham PT, Peng A, Wilkinson AH, Gritsch HA, Lassman C, Pham PC et al. Cyclosporine and tacrolimus-associated thrombotic microangiopathy. Am J Kidney Dis 2000; 36: 844–850.
Zarifian A, Meleg-Smith S, O’donovan R, Tesi RJ, Batuman V . Cyclosporine-associated thrombotic microangiopathy in renal allografts. Kidney Int 1999; 55: 2457–2466.
Trimarchi HM, Truong LD, Brennan S, Gonzalez JM, Suki WN . FK506-associated thrombotic microangiopathy: report of two cases and review of the literature. Transplantation 1999; 67: 539–544.
Fujino M, Kim Y, Ito M . Intestinal thrombotic microangiopathy induced by FK506 in rats. Bone Marrow Transplant 2007; 39: 367–372.
Abramowicz D, Pradier O, Marchant A, Florquin S, De Pauw L, Vereerstraeten P et al. Induction of thromboses within renal grafts by high-dose prophylactic OKT3. Lancet 1992; 339: 777–778.
Waiser J, Budde K, Rudolph B, Ortner MA, Neumayer HH . De novo hemolytic uremic syndrome postrenal transplant after cytomegalovirus infection. Am J Kidney Dis 1999; 34: 556–559.
Murer L, Zacchello G, Bianchi D, Dall’Amico R, Montini G, Andreetta B et al. Thrombotic microangiopathy associated with parvovirus B 19 infection after renal transplantation. J Am Soc Nephrol 2000; 11: 1132–1137.
Asaka M, Ishikawa I, Nakazawa T, Tomosugi N, Yuri T, Suzuki K . Hemolytic uremic syndrome associated with influenza A virus infection in an adult renal allograft recipient: case report and review of the literature. Nephron 2000; 84: 258–266.
Lawton CA, Barber-Derus SW, Murray KJ, Cohen EP, Ash RC, Moulder JE . Influence of renal shielding on the incidence of late renal dysfunction associated with T-lymphocyte deplete bone marrow transplantation in adult patients. Int J Radiat Oncol Biol Phys 1992; 23: 681–686.
Changsirikulchai S, Myerson D, Guthrie KA, McDonald GB, Alpers CE, Hingorani SR . Renal thrombotic microangiopathy after hematopoietic cell transplant: role of GVHD in pathogenesis. Clin J Am Soc Nephrol 2009; 4: 345–353.
Hale GA, Bowman LC, Rochester RJ, Benaim E, Heslop HE, Krance RA et al. Hemolytic uremic syndrome after bone marrow transplantation: clinical characteristics and outcome in children. Biol Blood Marrow Transplant 2005; 11: 912–920.
Uderzo C, Bonanomi S, Busca A, Renoldi M, Ferrari P, Iacobelli M et al. Risk factors and severe outcome in thrombotic microangiopathy after allogeneic hematopoietic stem cell transplantation. Transplantation 2006; 82: 638–644.
Siami K, Kojouri K, Swisher KK, Selby GB, George JN, Laszik ZG . Thrombotic microangiopathy after allogeneic hematopoietic stem cell transplantation: an autopsy study. Transplantation 2008; 85: 22–28.
George JN, Li X, McMinn JR, Terrell DR, Vesely SK, Selby GB . Thrombotic thrombocytopenic purpura-hemolytic uremic syndrome following allogeneic HPC transplantation: a diagnostic dilemma. Transfusion 2004; 44: 294–304.
Iacopino P, Pucci G, Arcese W, Bosi A, Falda M, Locatelli F et al. Severe thrombotic microangiopathy: an infrequent complication of bone marrow transplantation. Gruppo Italiano Trapianto Midollo Osseo (GITMO). Bone Marrow Transplant 1999; 24: 47–51.
Fuge R, Bird JM, Fraser A, Hart D, Hunt L, Cornish JM et al. The clinical features, risk factors and outcome of thrombotic thrombocytopenic purpura occurring after bone marrow transplantation. Br J Haematol 2001; 113: 58–64.
Shayani S, Palmer J, Stiller T, Liu X, Thomas SH, Khuu T et al. Thrombotic microangiopathy associated with sirolimus level after allogeneic hematopoietic cell transplantation with tacrolimus/sirolimus-based graft-versus-host disease prophylaxis. Biol Blood Marrow Transplant 2013; 19: 298–304.
Ruutu T, Barosi G, Benjamin RJ, Clark RE, George JN, Gratwohl A et al. Diagnostic criteria for hematopoietic stem cell transplant-associated microangiopathy: results of a consensus process by an International Working Group. Haematologica 2007; 92: 95–100.
Ho VT, Cutler C, Carter S, Martin P, Adams R, Horowitz M et al. Blood and marrow transplant clinical trials network toxicity committee consensus summary: thrombotic microangiopathy after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2005; 11: 571–575.
Cho B-S, Yahng S-A, Lee S-E, Eom K-S, Kim Y-J, Kim H-J et al. Validation of recently proposed consensus criteria for thrombotic microangiopathy after allogeneic hematopoietic stem-cell transplantation. Transplantation 2010; 90: 918–926.
Jodele S, Davies SM, Lane A, Khoury J, Dandoy C, Goebel J et al. Diagnostic and risk criteria for HSCT-associated thrombotic microangiopathy: a study in children and young adults. Blood 2014; 124: 645–653.
Schwimmer J, Nadasdy TA, Spitalnik PF, Kaplan KL, Zand MS . De novo thrombotic microangiopathy in renal transplant recipients: a comparison of hemolytic uremic syndrome with localized renal thrombotic microangiopathy. Am J Kidney Dis 2003; 41: 471–479.
Magro CM, Momtahen S, Mulvey JJ, Yassin AH, Kaplan RB, Laurence JC . Role of the skin biopsy in the diagnosis of atypical hemolytic uremic syndrome. Am J Dermatopathol 2015; 37: 349–359.
Sarma JV, Ward PA . The complement system. Cell Tissue Res 2011; 343: 227–235.
Walport MJ . Complement. First of two parts. N Engl J Med 2001; 344: 1058–1066.
MORGAN BP, GASQUE P . Extrahepatic complement biosynthesis: where, when and why? Clin Exp Immunol 1997; 107: 1–7.
Geiger H, Good RA, Day NK . Clearances of complement components, C3 proactivator and other serum proteins in chronic membranoproliferative glomerulonephritis (CMPGN). Clin Nephrol 1975; 3: 139–147.
Kusunoki Y, Akutsu Y, Itami N, Tochimaru H, Nagata Y, Takekoshi Y et al. Urinary excretion of terminal complement complexes in glomerular disease. Nephron 1991; 59: 27–32.
Manthei U, Strunk RC, Giclas PC . Acute local inflammation alters synthesis, distribution, and catabolism of third component of complement (C3) in rabbits. J Clin Invest 1984; 74: 424–433.
Giclas PC, Manthei U, Strunk RC . The acute phase response of C3, C5, ceruloplasmin, and C-reactive protein induced by turpentine pleurisy in the rabbit. Am J Pathol 1985; 120: 146–156.
Laufer J, Katz Y, Passwell JH . Extrahepatic synthesis of complement proteins in inflammation. Mol Immunol 2001; 38: 221–229.
Naughton MA, Botto M, Carter MJ, Alexander GJ, Goldman JM, Walport MJ . Extrahepatic secreted complement C3 contributes to circulating C3 levels in humans. J Immunol 1996; 156: 3051–3056.
Fey G, Colten HR . Biosynthesis of complement components. Fed Proc 1981; 40: 2099–2104.
Brauer RB, Baldwin WM, Wang D, Horwitz LR, Hess AD, Klein AS et al. Hepatic and extrahepatic biosynthesis of complement factor C6 in the rat. J Immunol 1994; 153: 3168–3176.
Langeggen H, Pausa M, Johnson E, Casarsa C, Tedesco F . The endothelium is an extrahepatic site of synthesis of the seventh component of the complement system. Clin Exp Immunol 2000; 121: 69–76.
Lévi-Strauss M, Mallat M . Primary cultures of murine astrocytes produce C3 and factor B, two components of the alternative pathway of complement activation. J Immunol 1987; 139: 2361–2366.
Barnum SR . Complement biosynthesis in the central nervous system. Crit Rev Oral Biol Med 1995; 6: 132–146.
Passwell J, Schreiner GF, Nonaka M, Beuscher HU, Colten HR . Local extrahepatic expression of complement genes C3, factor B, C2, and C4 is increased in murine lupus nephritis. J Clin Invest 1988; 82: 1676–1684.
Sacks S, Zhou W, Campbell RD, Martin J . C3 and C4 gene expression and interferon-gamma-mediated regulation in human glomerular mesangial cells. Clin Exp Immunol 1993; 93: 411–417.
Zhou W, Campbell RD, Martin J, Sacks SH . Interferon-gamma regulation of C4 gene expression in cultured human glomerular epithelial cells. Eur J Immunol 1993; 23: 2477–2481.
Richani K, Soto E, Romero R, Espinoza J, Chaiworapongsa T, Nien JK et al. Normal pregnancy is characterized by systemic activation of the complement system. J Matern Fetal Neonatal Med 2005; 17: 239–245.
Derzsy Z, Prohászka Z, Rigó J, Füst G, Molvarec A . Activation of the complement system in normal pregnancy and preeclampsia. Mol Immunol 2010; 47: 1500–1506.
White RT, Damm D, Hancock N, Rosen BS, Lowell BB, Usher P et al. Human adipsin is identical to complement factor D and is expressed at high levels in adipose tissue. J Biol Chem 1992; 267: 9210–9213.
Würzner R, Joysey VC, Lachmann PJ . Complement component C7. Assessment of in vivo synthesis after liver transplantation reveals that hepatocytes do not synthesize the majority of human C7. J Immunol 1994; 152: 4624–4629.
Høgåsen AK, Würzner R, Abrahamsen TG, Dierich MP . Human polymorphonuclear leukocytes store large amounts of terminal complement components C7 and C6, which may be released on stimulation. J Immunol 1995; 154: 4734–4740.
Li K, Sacks SH, Zhou W . The relative importance of local and systemic complement production in ischaemia, transplantation and other pathologies. Mol Immunol 2007; 44: 3866–3874.
Pangburn MK, Schreiber RD, Müller-Eberhard HJ . Formation of the initial C3 convertase of the alternative complement pathway. Acquisition of C3b-like activities by spontaneous hydrolysis of the putative thioester in native C3. J Exp Med 1981; 154: 856–867.
Pangburn MK, Müller-Eberhard HJ . Initiation of the alternative complement pathway due to spontaneous hydrolysis of the thioester of C3. Ann N Y Acad Sci 1983; 421: 291–298.
Sahu A, Lambris JD . Structure and biology of complement protein C3, a connecting link between innate and acquired immunity. Immunol Rev 2001; 180: 35–48.
Meehan SM, Kremer J, Ali FN, Curley J, Marino S, Chang A et al. Thrombotic microangiopathy and peritubular capillary C4d expression in renal allograft biopsies. Clin J Am Soc Nephrol 2011; 6: 395–403.
Chua JS, Baelde HJ, Zandbergen M, Wilhelmus S, van Es LA, de Fijter JW et al. Complement factor C4d is a common denominator in thrombotic microangiopathy. J Am Soc Nephrol 2015; 26: 2239–2247.
Roumenina LT, Loirat C, Dragon-Durey M-A, Halbwachs-Mecarelli L, Sautes-Fridman C, Fremeaux-Bacchi V . Alternative complement pathway assessment in patients with atypical HUS. J Immunol Methods 2011; 365: 8–26.
Meri S . Complement activation in diseases presenting with thrombotic microangiopathy. Eur J Intern Med 2013; 24: 496–502.
Noris M, Ruggenenti P, Perna A, Orisio S, Caprioli J, Skerka C et al. Hypocomplementemia discloses genetic predisposition to hemolytic uremic syndrome and thrombotic thrombocytopenic purpura: role of factor H abnormalities. Italian Registry of Familial and Recurrent Hemolytic Uremic Syndrome/Thrombotic Thrombocytopenic Purpura. J Am Soc Nephrol 1999; 10: 281–293.
Le Quintrec M, Zuber J, Moulin B, Kamar N, Jablonski M, Lionet A et al. Complement genes strongly predict recurrence and graft outcome in adult renal transplant recipients with atypical hemolytic and uremic syndrome. Am J Transplant 2013; 13: 663–675.
Sellier-Leclerc A-L, Fremeaux-Bacchi V, Dragon-Durey M-A, Macher M-A, Niaudet P, Guest G et al. Differential impact of complement mutations on clinical characteristics in atypical hemolytic uremic syndrome. J Am Soc Nephrol 2007; 18: 2392–2400.
Noris M, Caprioli J, Bresin E, Mossali C, Pianetti G, Gamba S et al. Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype. Clin J Am Soc Nephrol 2010; 5: 1844–1859.
Kavanagh D, Goodship T . Genetics and complement in atypical HUS. Pediatr Nephrol 2010; 25: 2431–2442.
Maga TK, Nishimura CJ, Weaver AE, Frees KL, Smith RJ . Mutations in alternative pathway complement proteins in American patients with atypical hemolytic uremic syndrome. Hum Mutat 2010; 31: E1445–E1460.
Loirat C, Noris M, Fremeaux-Bacchi V . Complement and the atypical hemolytic uremic syndrome in children. Pediatr Nephrol 2008; 23: 1957–1972.
Caprioli J, Castelletti F, Bucchioni S, Bettinaglio P, Bresin E, Pianetti G et al. Complement factor H mutations and gene polymorphisms in haemolytic uraemic syndrome: the C-257T, the A2089G and the G2881T polymorphisms are strongly associated with the disease. Hum Mol Genet 2003; 12: 3385–3395.
Richards A, Buddles MR, Donne RL, Kaplan BS, Kirk E, Venning MC et al. Factor H mutations in hemolytic uremic syndrome cluster in exons 18-20, a domain important for host cell recognition. Am J Hum Genet 2001; 68: 485–490.
Kavanagh D, Richards A, Noris M, Hauhart R, Liszewski MK, Karpman D et al. Characterization of mutations in complement factor I (CFI) associated with hemolytic uremic syndrome. Mol Immunol 2008; 45: 95–105.
Fremeaux-Bacchi V, Dragon-Durey M, Blouin J, Vigneau C, Kuypers D, Boudailliez B et al. Complement factor I: a susceptibility gene for atypical haemolytic uraemic syndrome. J Med Genet 2004; 41: e84.
Frémeaux-Bacchi V, Miller EC, Liszewski MK, Strain L, Blouin J, Brown AL et al. Mutations in complement C3 predispose to development of atypical hemolytic uremic syndrome. Blood 2008; 112: 4948–4952.
Fremeaux-Bacchi V, Moulton EA, Kavanagh D, Dragon-Durey M-A, Blouin J, Caudy A et al. Genetic and functional analyses of membrane cofactor protein (CD46) mutations in atypical hemolytic uremic syndrome. J Am Soc Nephrol 2006; 17: 2017–2025.
Noris M, Brioschi S, Caprioli J, Todeschini M, Bresin E, Porrati F et al. Familial haemolytic uraemic syndrome and an MCP mutation. Lancet 2003; 362: 1542–1547.
Goicoechea de Jorge E, Harris CL, Esparza-Gordillo J, Carreras L, Arranz EA, Garrido CA et al. Gain-of-function mutations in complement factor B are associated with atypical hemolytic uremic syndrome. Proc Natl Acad Sci USA 2007; 104: 240–245.
Jodele S, Zhang K, Zou F, Laskin B, Dandoy CE, Myers KC et al. The genetic fingerprint of susceptibility for transplant associated thrombotic microangiopathy. Blood 2015; 127: 989–996.
Goldberg RJ, Nakagawa T, Johnson RJ, Thurman JM . The role of endothelial cell injury in thrombotic microangiopathy. Am J Kidney Dis 2010; 56: 1168–1174.
Robson M, Côte I, Abbs I, Koffman G, Goldsmith D . Thrombotic micro-angiopathy with sirolimus-based immunosuppression: potentiation of calcineurin-inhibitor-induced endothelial damage? Am J Transplant 2003; 3: 324–327.
Garcia-Maldonado M, Kaufman CE, Comp PC . Decrease in endothelial cell-dependent protein C activation induced by thrombomodulin by treatment with cyclosporine. Transplantation 1991; 51: 701–705.
Brown Z, Neild GH . Cyclosporine inhibits prostacyclin production by cultured human endothelial cells. Transplant Proc 1987; 19: 1178–1180.
Renner B, Klawitter J, Goldberg R, McCullough JW, Ferreira VP, Cooper JE et al. Cyclosporine induces endothelial cell release of complement-activating microparticles. J Am Soc Nephrol 2013; 24: 1849–1862.
Kim YO, Lim SW, Li C, Kang HJ, Ahn KO, Yang HJ et al. Activation of intrarenal complement system in mouse model for chronic cyclosporine nephrotoxicity. Yonsei Med J 2007; 48: 517–525.
Vercellotti GM, Moldow CF, Jacob HS . Complement, oxidants, and endothelial injury: how a bedside observation opened a door to vascular biology. J Clin Invest 2012; 122: 3044–3045.
Sacks T, Moldow CF, Craddock PR, Bowers TK, Jacob HS . Oxygen radicals mediate endothelial cell damage by complement-stimulated granulocytes. an in vitro model of immune vascular damage. J Clin Invest 1978; 61: 1161–1167.
Eremina V, Jefferson JA, Kowalewska J, Hochster H, Haas M, Weisstuch J et al. VEGF inhibition and renal thrombotic microangiopathy. N Engl J Med 2008; 358: 1129–1136.
Takatsuka H, Wakae T, Mori A, Okada M, Okamoto T, Kakishita E . Effects of total body irradiation on the vascular endothelium. Clin Transplant 2002; 16: 374–377.
Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 2006; 355: 1572–1582.
Kersting S, Koomans HA, Hené RJ, Verdonck LF . Acute renal failure after allogeneic myeloablative stem cell transplantation: retrospective analysis of incidence, risk factors and survival. Bone Marrow Transplant 2007; 39: 359–365.
Gooley TA, Chien JW, Pergam SA, Hingorani S, Sorror ML, Boeckh M et al. Reduced mortality after allogeneic hematopoietic cell transplantation. N Engl J Med 2010; 363: 2091–2101.
Schwarz A, Haller H, Schmitt R, Schiffer M, Koenecke C, Strassburg C et al. Biopsy-diagnosed renal disease in patients after transplantation of other organs and tissues. Am J Transplant 2010; 10: 2017–2025.
Glezerman IG, Jhaveri KD, Watson TH, Edwards AM, Papadopoulos EB, Young JW et al. Chronic kidney disease, thrombotic microangiopathy, and hypertension following T cell-depleted hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2010; 16: 976–984.
Kim SS, Patel M, Yum K, Keyzner A . Hematopoietic stem cell transplant-associated thrombotic microangiopathy: review of pharmacologic treatment options. Transfusion 2015; 55: 452–458.
Sarode R, McFarland JG, Flomenberg N, Casper JT, Cohen EP, Drobyski WR et al. Therapeutic plasma exchange does not appear to be effective in the management of thrombotic thrombocytopenic purpura/hemolytic uremic syndrome following bone marrow transplantation. Bone Marrow Transplant 1995; 16: 271–275.
Rizvi MA, Vesely SK, George JN, Chandler L, Duvall D, Smith JW et al. Complications of plasma exchange in 71 consecutive patients treated for clinically suspected thrombotic thrombocytopenic purpura-hemolytic-uremic syndrome. Transfusion 2000; 40: 896–901.
Roy V, Rizvi MA, Vesely SK, George JN . Thrombotic thrombocytopenic purpura-like syndromes following bone marrow transplantation: an analysis of associated conditions and clinical outcomes. Bone Marrow Transplant 2001; 27: 641–646.
Stegmayr B, Tärnvik A . Complement activation in plasma exchange by single filtration and centrifugation and in cascade filtration. Blood Purif 1989; 7: 10–15.
Burnouf T, Eber M, Kientz D, Cazenave J-P, Burkhardt T . Assessment of complement activation during membrane-based plasmapheresis procedures. J Clin Apher 2004; 19: 142–147.
Mache CJ, Acham-Roschitz B, Frémeaux-Bacchi V, Kirschfink M, Zipfel PF, Roedl S et al. Complement inhibitor eculizumab in atypical hemolytic uremic syndrome. Clin J Am Soc Nephrol 2009; 4: 1312–1316.
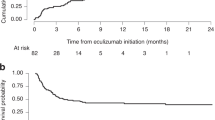
Jodele S, Fukuda T, Vinks A, Mizuno K, Laskin BL, Goebel J et al. Eculizumab therapy in children with severe hematopoietic stem cell transplantation-associated thrombotic microangiopathy. Biol Blood Marrow Transplant 2014; 20: 518–525.
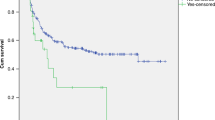
Legendre CM, Licht C, Muus P, Greenbaum LA, Babu S, Bedrosian C et al. Terminal complement inhibitor eculizumab in atypical hemolytic-uremic syndrome. N Engl J Med 2013; 368: 2169–2181.
Zuber J, Le Quintrec M, Morris H, Frémeaux-Bacchi V, Loirat C, Legendre C . Targeted strategies in the prevention and management of atypical HUS recurrence after kidney transplantation. Transplant Rev (Orlando) 2013; 27: 117–125.
Baskin E, Gulleroglu K, Kantar A, Bayrakci U, Ozkaya O . Success of eculizumab in the treatment of atypical hemolytic uremic syndrome. Pediatr Nephrol 2015; 30: 783–789.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Obut, F., Kasinath, V. & Abdi, R. Post-bone marrow transplant thrombotic microangiopathy. Bone Marrow Transplant 51, 891–897 (2016). https://doi.org/10.1038/bmt.2016.61
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.61
This article is cited by
-
Use of defibrotide to treat adult patients with transplant-associated thrombotic microangiopathy
Bone Marrow Transplantation (2019)
-
High mortality in hematopoietic stem cell transplant-associated thrombotic microangiopathy with and without concomitant acute graft-versus-host disease
Bone Marrow Transplantation (2019)
-
Use of Defibrotide to help prevent post-transplant endothelial injury in a genetically predisposed infant with metachromatic leukodystrophy undergoing hematopoietic stem cell gene therapy
Bone Marrow Transplantation (2018)