Abstract
Background:
Aberrant Notch1 activation has been studied in many malignant tumours, but its role in gastric cancer remains unknown. This study is aimed to investigate the prognostic significance of Notch1 activation in patients with gastric cancer.
Methods:
In this study, we prospectively enrolled two independent sets of patients with gastric cancer from China and defined the activation of Notch1 by immunohistochemical staining of its active form, intracellular domain of Notch1 (ICN1). The prognostic value of Notch1 activation and clinical outcomes in gastric cancer were evaluated.
Results:
Expression of ICN1 is elevated in gastric cancer tissues and is predominately localised in the cell cytoplasm and/or membrane. High ICN1 expression positively correlates with tumour invasion depth (P=0.032), lymph node metastasis (P<0.001), advanced TNM stage (P=0.003) and reduced overall survival (P=0.0004) in the training set. Multivariate Cox regression analysis identified ICN1 as an independent prognostic factor (P=0.031), which could be incorporated into the TNM system to generate a better predictive model for patient outcomes. The c-index was 0.7375 when assessed with the TNM stage and improved to 0.8037 when ICN1 expression was added in the training set. These results were validated in the validation set.
Conclusions:
Notch1 activation was correlated with gastric cancer progression and defined as a novel independent prognostic factor. Combining ICN1 expression with TNM stage may provide a better predictive model for outcomes of gastric cancer patients.
Similar content being viewed by others
Main
Although the incidence of gastric cancer has declined in recent years for improvement on prevention strategy, it remains the fourth common malignant tumour and the second most common cause of tumour-associated death in the world (Jemal et al, 2011). New cases occurred in China, accounting for nearly half of the world total (Yang, 2006). A larger number of patients are diagnosed as unresectable owing to atypical symptoms at early stage. Traditional prognostic model for gastric cancer was based on tumour cell-centred phenotype such as the TNM stage. However, increasing evidences have shown that patients in the same stage may have quite different outcomes, partly owing to the heterogeneity of tumour (Lim et al, 2005; Stock and Otto, 2005). Thus, elucidation of the molecular mechanisms underlying the tumour heterogeneity may add some prognostic information for the current TNM prognostic model and may provide novel therapeutic targets for patients with gastric cancer.
Notch1 is a type I transmembrane heterodimeric receptor that directly activates transcription of gene targets upon productive interactions with Notch ligands (Fortini, 2009; Kopan and Ilagan, 2009). Sequential cleavage of Notch1 is required for activation of the full-length receptors. Intracellular domain of Notch 1 (ICN1), the active form of Notch1, is released by proteolysis from the full-length Notch1 and transferred to the cell nucleus to associate with DNA-binding protein to assemble a transcription complex that activates downstream target genes. Previous studies have identified a multifaceted functional role of Notch signal in diverse cellular processes such as cell differentiation, proliferation, apoptosis, adhesion, migration, epithelial-to-mesenchymal transition (EMT), angiogenesis and oncogenesis (Artavanis-Tsakonas et al, 1999; Bolos et al, 2007). Although aberrant expression of Notch1 has been reported in a growing number of solid tumours, whether Notch1 signalling will be oncogenic or tumour suppressive was decided by the specific cell type and the presence of specific cytokines/growth factors in the cellular microenvironment and the dosage of signalling (Leong and Karsan, 2006).
Previous studies revealed that high expression of Notch1 in breast cancer (Reedijk et al, 2005), colorectal tumour (Reedijk et al, 2008), glioblastoma (Kanamori et al, 2007), oral squamous cell carcinoma (Joo et al, 2009) and melanoma (Balint et al, 2005; Liu et al, 2006) is correlated with tumour progression, whereas Notch 1 acts as a tumour suppressor gene in prostate cancer (Whelan et al, 2009), liver cancer (Wang et al, 2009), pancreatic cancer (Mullendore et al, 2009) and skin tumour (Panelos et al, 2008). Moreover, evidence obtained from studies of cervix cancer suggests that Notch signalling during the initial stages of tumourigenesis can prevent tumour formation, in contrast to later stages of tumour development, in which Notch activation is required (Talora et al, 2002). On the basis of these results, the activation of Notch1 in different tumours may have diametrical functions. Previous studies have revealed that Notch receptors (Notch1–3) and Notch ligand Jagged1 are expressed in human gastric cancer (Sander and Powell, 2004). Activation of Notch1 signal could promote progression of gastric cancer, partly via cyclooxygenase-2 (Yeh et al, 2009). However, the clinical significance of Notch1 activation and its correlation with gastric cancer progression remains largely unknown and needs to be further established.
In this study, we discovered that Notch1 activation, as indicated by elevated ICN1 levels, associates with gastric cancer progression. Intratumoral levels of ICN1 were positively correlated with tumour invasion depth, TNM stage and poor overall survival (OS) in gastric cancer patients. Notch1 activation can be used as an independent prognostic factor and should be incorporated with TNM stage to generate a better predictive model for outcomes of gastric cancer patients. These data identified the potential prognostic significance of Notch1 activation and may open a new avenue for therapeutic intervention with Notch1 for advanced-stage gastric cancer patients.
Materials and methods
Patients and specimens
Two independent sets comprising 191 gastric cancer patients who received standard gastrectomy with lymph node resection from two institutional clinical centres were enrolled in our study. The training set that comprised 101 consecutive patients with total or partial gastrectomy was obtained from Zhongshan Hospital (Shanghai, China) between 2000 and 2005. The validation set that comprised 90 consecutive patients was obtained from Nantong Tumor Hospital (Jiangsu, China) between May 2007 and February 2008 with the same enrolment critea. All specimens were obtained from patients with informed consent approved by the Clinical Research Ethics Committee of each hospital. Clinicopathological variables including age, sex, location, tumour size, tumour differentiation, Lauren classification and TNM stage were collected for each patient. Tumour size was defined as the longest diameter according to the pathology report. None of these patients received any preoperative anticancer treatment. All specimens were pathologically reassessed independently by two gastroenterology pathologists according to the 2010 International Union against Cancer TNM classification system.
Tissue microarray, immunohistochemistry and evaluation of immunohistochemical findings
Formalin-fixed, paraffin embedded surgical specimens were used for tissue microarray construction and for subsequent immunohistochemistry (IHC) study. Two cores were taken from each surgical sample by using punch cores that measured 1.5 mm in the greatest dimension from the centre of the tumour foci. Tissue blocks were mounted on glass slides by sequencing. The IHC protocols were as described previously (Liu et al, 2011). The primary antibody against ICN1 (Abcam, Cambridge, MA, USA) was used. The specificity of the antibody was demonstrated by IHC with peptide competition. The intensity of immunohistochemical staining of ICN1 was scored by two gastroenterology pathologists using the semiquantitative immunoreactivity scoring (IRS) system as described previously (Weichert et al, 2008). Immunoreactivity score was derived by multiplying the intensity of immunohistochemical staining and the percentage of immunoreactive cells ranged from 0 to 12, and we defined 8 as the cutoff value for high and low expression according to the ‘minimum P-value method’ on the basis of its relation with OS. The negative control staining was treated equally with the primary antibody omitted.
Statistical analysis
The analysis was performed with SPSS 19.0 (SPSS Inc., Chicago, IL, USA). Pearson’s χ2 test or Fisher’s exact test was used to compare qualitative variables. Kaplan–Meier analysis was used to determine the survival. Log-rank test was used to compare patient survival between subgroups. Numbers at risk were calculated at the beginning of each time period. The Cox proportional hazards regression model was used to perform univariate and multivariate analyses, and P>0.10 was the criterion used for variable deletions when performing stepwise regression. Receiver operating characteristic (ROC) curve analysis was used to determine the predictive value of the parameters. All significance tests were two-sided and P<0.05 was considered statistically significant. Results are reported according to the REMARK (Reporting Recommendations for Tumour Marker Prognostic Studies) guidelines (McShane et al, 2005).
Results
Patient characteristics
The detailed characteristics of patients were shown in Table 1. There were more patients diagnosed at an advanced stage (TNM III+IV) in the validation set compared with the training set (67.7% vs 46.5%) and more distal gastric cancer in the validation set compared with the training set (64.5% vs 41.6%). Overall survival was defined as the interval between surgery and last visit or death. The follow-up median time was 77 and 35 months for the training and validation sets, respectively. Such heterogeneity may help confirming that the predictor has universal applicability across heterogeneous population of patients from different districts.
Innmunohistochemical findings
To ascertain the expression of activated Notch1 in gastric tumour tissue, we examined the expression of ICN1 in the training and validation sets of specimens and matched the non-tumour specimens by IHC staining. The expression of ICN1 was mainly localised in the cell cytoplasm and/or membrane in the tumour area, and showed variable staining intensity, whereas stroma cells showed negative staining (Figure 1A–D). The expression level was elevated in tumour tissues compared with non-tumour tissues. High ICN1 expression was more easily seen in advanced tumour stage and the percentage of positive IHC staining increased with tumour progression according to the TNM stage (Figure 1E). Conclusively, the expression of ICN1 was elevated in gastric tumour tissues compared with non-tumour tissues, especially in advanced tumour stage, indicating the potential oncogenic role of Notch1 activation in gastric cancer.
Expression of ICN1 in sections of gastric cancer. Representative microphotographs of ICN1 expression (A–D). Negative control (A); non-tumour weak intensity (B); intratumoral moderate intensity (C); intratumoral strong intensity (D). (E) The percentage of patients with ICN1 high or low expression according to the TNM stage in the training (left panel) and validation (right panel) sets. Original magnification: × 200.
Relation between ICN1 expression and clinicopathological features in gastric cancer patients
The correlation between ICN1 expression and clincopahtological features in gastric cancer patients were shown in Table 1. According to the cutoff value derived from IRS score, 48.5% (49–101) and 50% (45–90) were ICN1 low expression in the training and validation sets, respectively. Intracellular domain of Notch1 expression was correlated with tumour invasion depth (P=0.032 and 0.013, respectively) and TNM stage (P=0.003 and 0.031, respectively) in the two independent sets. In addition, in the training set, ICN1 expression was associated with lymph node metastasis (P<0.001), and in the validation set, ICN1 expression was correlated with tumour differentiation (P=0.048). High ICN1 expression was more easily seen in patients with increased tumour invasion depth and advanced TNM stage. In conclusion, intratumoral ICN1 expression may correlate with gastric cancer progression.
Association between ICN1 expression and OS in patients with gastric cancer
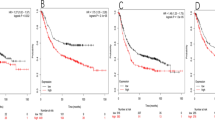
To further investigate the relation between ICN1 expression and OS, we compared the OS between ICN1 high expression and ICN1 low expression subgroups by using Kaplan–Meier analysis and log-rank test. Intracellular domain of Notch1 low expression has a survival benefit compared with high expression (Figure 2A, P=0.0004 and 0.0001, respectively) in two independent sets, indicating that intratumoral ICN1 expression may be an important molecular mechanism in identifying outcomes for gastric cancer patients. For further investigation of the effect of ICN1 expression in stratifying patients with different TNM stratum, we combined TNM I+II and TNM III+IV as an early-stage tumour and as an advanced-stage tumour, respectively. In the early stage, ICN1 expression did not show prognostic significance with OS (Figure 2B, P=0.6817 and 0.1702, respectively), whereas for patients in advanced stage, ICN1 low expression had a great survival benefit compared with high expression (Figure 2C, P=0.0094 and 0.0026, respectively) in the training and validation sets. All these results here showed that ICN1 expression correlates with OS for patients with gastric cancer, especially for the advanced stage.
Kaplan–Meier analysis for OS of patients with gastric cancer according to the ICN1 expression. (A–C) Kaplan–Meier analysis for OS of patients with gastric cancer according to ICN1 expression in (A) all patients (left panel, training set, n=101, P=0.0004; right panel, validation set, n=90, P=0.0001), (B) TNM I+II (left panel, training set, n=54, P=0.6817; right panel, validation set, n=29, P=0.1702) and (C) TNM III+IV (left panel, training set, n=47, P=0.0094; right panel, validation set, n=61, P=0.0026). P-value was calculated by log-rank test.
Prognostic factor
To identify the prognostic significance of clinicopathological factors for OS, univariate Cox analysis was conducted. T classification (HR, 7.996; 95% CI, 1.905–35.559, P=0.005), N classification (HR, 14.251; 95% CI, 3.394–59.843, P<0.001), distant metastasis (HR, 13.121; 95% CI, 3.538–48.665, P<0.001), TNM stage (HR, 10.648; 95% CI, 3.713–30.538, P<0.001) and ICN1 expression (HR, 4.072; 95% CI, 1.752–9.466, P=0.001) were identified as risk factors that may affect the OS of gastric cancer patients in the training set, whereas distant metastasis (HR, 3.346; 95% CI, 1.012–11.069, P=0.048), TNM stage (HR, 2.879; 95% CI, 1.521–5.450, P=0.001) and ICN1 expression (HR, 2.797; 95% CI, 1.645–4.755, P<0.001) were identified as risk factors for OS in the validation set (Table 2). Further adjustment of covariate factors by using multivariate Cox analysis identified TNM stage (HR, 8.547; 95% CI, 2.931–24.925, P<0.001 and HR, 2.427; 95% CI, 1.267–4.646, P=0.007) and ICN1 expression (HR, 2.579; 95% CI, 1.093–6.086, P=0.031 and HR, 2.414; 95% CI, 1.407–4.143, P=0.001) as independent prognostic factors for the training and validation sets, respectively (Figure 3A). Patients with ICN1 high expression in the advanced stage showed more risk for a reduced OS (HR, 3.688; 95% CI, 1.219–10.715, P=0.016 and HR, 2.475; 95% CI, 1.338–4.577, P=0.004), whereas patients in early stage did not have such a risk (HR, 0.625; 95% CI, 0.065–6.014, P=0.625 and HR, 2.187; 95% CI, 0.689–6.924, P=0.184) in the two independent sets (Figure 3A). In conclusion, intratumoral ICN1 expression may be a novel defined independent prognostic factor for gastric cancer patients, especially for advanced tumour.
Multivariate Cox analysis and ROC analysis for the predictive value of ICN1 expression in gastric cancer patients. (A) Multivariate Cox analysis identified independent prognostic factors for the training and validation sets. (B) Receiver operating characteristic analysis of the sensitivity and specificity for the predictive value of combined TNM and ICN1 stratification model, TNM model, ICN1 model in the training (left panel) and validation (right panel). P-value <0.05 was considered statistically significant.
Combination of ICN1 expression and TNM stage and ROC analysis
To generate a more sensitive predictive model for outcomes of patients with gastric cancer, we combined ICN1 expression and TNM stage to create a prognostic score system. Receiver operating characteristic analysis was used to compare the prognostic validity of the combination between ICN1 or TNM stage alone. The combination of ICN1 and TNM stage showed better prognostic value (AUC (95%), 0.854 (0.770–0.916)) compared with TNM stage (AUC (95%), 0.793 (0.701–0.867), P=0.0263) or ICN1 expression (AUC (95%), 0.687 (0.587–0.776), P<0.0001) alone in the training set and (AUC (95%), 0.756 (0.654–0.840)) compared with TNM stage (AUC (95%), 0.683 (0.577–0.777), P=0.0149) or ICN1 expression (AUC (95%), 0.675 (0.568–0.770), P<0.01) alone in the validation set (Figure 3B). The c-index was 0.7375 when assessed with TNM stage and improved to 0.8037 when ICN1 expression was added in the training set (Table 3). The AIC was 244.32 when assessed with TNM stage and reduced to 231.31 when ICN1 expression was added in the training set (Table 3). These results were validated in the validation set (Table 3). All these results proved that combination of ICN1 and TNM stage can generate a better predictive model for OS of gastric cancer patients.
Discussion
Traditional predictive model for outcomes of patients with gastric cancer relies on TNM stage and is limited in its ability to discriminate a subset of patients for the heterogeneity of tumour. In fact, tumour cells acquired different biological phenotype by various mechanisms in disease initiation and progression. Thus, elucidation of the molecular mechanisms underlying the tumour heterogeneity may shed light on better prediction for patient outcomes. In our study, we have demonstrated the prognostic power of Notch1 activation for gastric cancer and revealed that Notch1 activation may be a potential mechanism under tumour heterogeneity. These results have both prognostic and therapeutic implications.
Notch signalling defines an evolutionarily conserved local cell interaction mechanism that participates in a variety of cellular processes (Bolos et al, 2007). Aberrant expression of Notch has been reported in various solid malignancies and function as an oncogene or as a tumour suppressor gene (Balint et al, 2005; Reedijk et al, 2005; Liu et al, 2006; Kanamori et al, 2007; Panelos et al, 2008; Reedijk et al, 2008; Joo et al, 2009; Mullendore et al, 2009; Wang et al, 2009; Whelan et al, 2009). In this study, we focused mainly on Notch1 and found that Notch1 activation, represented by ICN1 expression, correlates with outcomes of gastric cancer patients and can be used as a novel independent prognostic factor. Early-stage gastric cancer exhibited relative lower portion of ICN1 staining, whereas advanced-stage gastric cancer showed elevated ICN1 staining (Figure 1). Intracellular domain of Notch1 high expression in advanced-stage gastric cancer indicated its possible role in the maintenance of stem cell-like property. All these results further confirmed the functional role of ICN1 expression in tumour progression.
Further analysis of the relation between ICN1 expression and OS of gastric cancer patients revealed a negative correlation. Survival of advanced-stage gastric cancer patients can be stratified by ICN1 expression, whereas patients in early stage cannot (Figure 2). Incorporating ICN1 expression into current prognostic TNM staging system improved the prognostic value for OS (Figure 3B). These results showed that ICN1 expression might add some prognostic information for patients with gastric cancer and lead to a more precise classification integrated with TNM stage. However, the results of combination of intratumoral ICN1 expression into the current prognostic model need an independent and larger data set to validate.
Numerous mechanisms have suggested to have a role in Notch-induced solid tumourigenesis, but the exact mechanisms were diverse in different tumours. Activated Notch signalling can suppress p53 activity in T-acute lymphoblastic leukemia and breast cancer to promote oncogenesis through increased cell survival and genomic instability (Beverly et al, 2005; Mungamuri et al, 2006). Increased Notch signalling has also been associated with the maintenance of a stem-like cell population in medulloblastoma by interacting with hedgehog signalling (Hallahan et al, 2004), and by activation of PI3K-AKT pathways in melanoma (Liu et al, 2006). Activation of the Notch1 signalling pathway could promote gastric cancer progression at least in part through COX-2 (Yeh et al, 2009). All these results revealed a multifaceted pathway of Notch1 activation underlies tumour progression. However, the exact molecular function roles of Notch1 activation in gastric cancer progression remain far from being fully elucidated and is awaiting further investigation.
As Notch1 activation indicate tumour progression and poor outcome in patients with gastric cancer, targeting Notch1 signalling steps, including ligand/receptor binding, release of ICN1, interaction of ICN1 and downstream target genes, as well as ICN1 protein stability, may have antitumour effects. Currently, blocking Notch1 signalling by suppressing the proteolytic step, which is mediated by γ-secretase, leads to the generation of ICN1 becoming plausible (Shih and Wang, 2007). Inhibitors of γ-secretase have been studied worldwide in the past decades for their potential to block the generation of Aβ peptide that is associated with Alzheimer’s disease (Selkoe and Kopan, 2003). Thus, γ-secretase inhibitors tested clinically for Alzheimer’s disease may be applicable to treat tumours that have constitutive Notch1 activation. Previous studies have also revealed that Notch signalling pathway activation may have a critical role in the regulation of chemotherapy resistance via promoting EMT and stem-cell like property (Wang et al, 2010). Blocking Notch1 activation may restore the sensitivity of tumour to chemotherapy treatment. These data suggest that targeting Notch1 signal with γ-secretase inhibitors may be a novel and efficient strategy for the treatment in advanced gastric cancer patients alone or combined with traditional cytotoxic drugs.
Although our study proved the prognostic significance of Notch1 activation in patients with gastric cancer, there are some limitations. The study is retrospective in nature and the number of patients enrolled is relatively small. A larger, multicentred, prospective data are needed to validate these results.
In conclusion, we have identified that Notch1 activation correlates with gastric cancer progression and can be used as a novel prognostic factor for patient outcomes. Incorporating ICN1 expression into TNM stage can provide a better prognostic model for patients with gastric cancer. Targeting Notch1 activation may open a new avenue for treatment of advanced-stage gastric cancer.
Change history
29 April 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Artavanis-Tsakonas S, Rand MD, Lake RJ (1999) Notch signaling: cell fate control and signal integration in development. Science 284: 770–776.
Balint K, Xiao M, Pinnix CC, Soma A, Veres I, Juhasz I, Brown EJ, Capobianco AJ, Herlyn M, Liu ZJ (2005) Activation of Notch1 signaling is required for beta-catenin-mediated human primary melanoma progression. J Clin Invest 115: 3166–3176.
Beverly LJ, Felsher DW, Capobianco AJ (2005) Suppression of p53 by Notch in lymphomagenesis: implications for initiation and regression. Cancer Res 65: 7159–7168.
Bolos V, Grego-Bessa J, de la Pompa JL (2007) Notch signaling in development and cancer. Endocr Rev 28: 339–363.
Fortini ME (2009) Notch signaling: the core pathway and its posttranslational regulation. Dev Cell 16: 633–647.
Hallahan AR, Pritchard JI, Hansen S, Benson M, Stoeck J, Hatton BA, Russell TL, Ellenbogen RG, Bernstein ID, Beachy PA, Olson JM (2004) The SmoA1 mouse model reveals that notch signaling is critical for the growth and survival of sonic hedgehog-induced medulloblastomas. Cancer Res 64: 7794–7800.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61: 69–90.
Joo YH, Jung CK, Kim MS, Sun DI (2009) Relationship between vascular endothelial growth factor and Notch1 expression and lymphatic metastasis in tongue cancer. Otolaryngol Head Neck Surg 140: 512–518.
Kanamori M, Kawaguchi T, Nigro JM, Feuerstein BG, Berger MS, Miele L, Pieper RO (2007) Contribution of Notch signaling activation to human glioblastoma multiforme. J Neurosurg 106: 417–427.
Kopan R, Ilagan MX (2009) The canonical Notch signaling pathway: unfolding the activation mechanism. Cell 137: 216–233.
Leong KG, Karsan A (2006) Recent insights into the role of Notch signaling in tumorigenesis. Blood 107: 2223–2233.
Lim L, Michael M, Mann GB, Leong T (2005) Adjuvant therapy in gastric cancer. J Clin Oncol 23: 6220–6232.
Liu H, Xu J, Zhou L, Yun X, Chen L, Wang S, Sun L, Wen Y, Gu J (2011) Hepatitis B virus large surface antigen promotes liver carcinogenesis by activating the Src/PI3K/Akt pathway. Cancer Res 71: 7547–7557.
Liu ZJ, Xiao M, Balint K, Smalley KS, Brafford P, Qiu R, Pinnix CC, Li X, Herlyn M (2006) Notch1 signaling promotes primary melanoma progression by activating mitogen-activated protein kinase/phosphatidylinositol 3-kinase-Akt pathways and up-regulating N-cadherin expression. Cancer Res 66: 4182–4190.
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM (2005) Reporting recommendations for tumor marker prognostic studies. J Clin Oncol 23: 9067–9072.
Mullendore ME, Koorstra JB, Li YM, Offerhaus GJ, Fan X, Henderson CM, Matsui W, Eberhart CG, Maitra A, Feldmann G (2009) Ligand-dependent Notch signaling is involved in tumor initiation and tumor maintenance in pancreatic cancer. Clin Cancer Res 15: 2291–2301.
Mungamuri SK, Yang X, Thor AD, Somasundaram K (2006) Survival signaling by Notch1: mammalian target of rapamycin (mTOR)-dependent inhibition of p53. Cancer Res 66: 4715–4724.
Panelos J, Tarantini F, Paglierani M, Di Serio C, Maio V, Pellerito S, Pimpinelli N, Santucci M, Massi D (2008) Photoexposition discriminates Notch 1 expression in human cutaneous squamous cell carcinoma. Mod Pathol 21: 316–325.
Reedijk M, Odorcic S, Chang L, Zhang H, Miller N, McCready DR, Lockwood G, Egan SE (2005) High-level coexpression of JAG1 and NOTCH1 is observed in human breast cancer and is associated with poor overall survival. Cancer Res 65: 8530–8537.
Reedijk M, Odorcic S, Zhang H, Chetty R, Tennert C, Dickson BC, Lockwood G, Gallinger S, Egan SE (2008) Activation of Notch signaling in human colon adenocarcinoma. Int J Oncol 33: 1223–1229.
Sander GR, Powell BC (2004) Expression of notch receptors and ligands in the adult gut. J Histochem Cytochem 52: 509–516.
Selkoe D, Kopan R (2003) Notch and Presenilin: regulated intramembrane proteolysis links development and degeneration. Annu Rev Neurosci 26: 565–597.
Shih IeM, Wang TL (2007) Notch signaling, gamma-secretase inhibitors, and cancer therapy. Cancer Res 67: 1879–1882.
Stock M, Otto F (2005) Gene deregulation in gastric cancer. Gene 360: 1–19.
Talora C, Sgroi DC, Crum CP, Dotto GP (2002) Specific down-modulation of Notch1 signaling in cervical cancer cells is required for sustained HPV-E6/E7 expression and late steps of malignant transformation. Genes Dev 16: 2252–2263.
Wang M, Xue L, Cao Q, Lin Y, Ding Y, Yang P, Che L (2009) Expression of Notch1, Jagged1 and beta-catenin and their clinicopathological significance in hepatocellular carcinoma. Neoplasma 56: 533–541.
Wang Z, Li Y, Ahmad A, Azmi AS, Banerjee S, Kong D, Sarkar FH (2010) Targeting Notch signaling pathway to overcome drug resistance for cancer therapy. Biochim Biophys Acta 1806: 258–267.
Weichert W, Roske A, Gekeler V, Beckers T, Ebert MP, Pross M, Dietel M, Denkert C, Rocken C (2008) Association of patterns of class I histone deacetylase expression with patient prognosis in gastric cancer: a retrospective analysis. Lancet Oncol 9: 139–148.
Whelan JT, Kellogg A, Shewchuk BM, Hewan-Lowe K, Bertrand FE (2009) Notch-1 signaling is lost in prostate adenocarcinoma and promotes PTEN gene expression. J Cell Biochem 107: 992–1001.
Yang L (2006) Incidence and mortality of gastric cancer in China. World J Gastroenterol 12: 17–20.
Yeh TS, Wu CW, Hsu KW, Liao WJ, Yang MC, Li AF, Wang AM, Kuo ML, Chi CW (2009) The activated Notch1 signal pathway is associated with gastric cancer progression through cyclooxygenase-2. Cancer Res 69: 5039–5048.
Acknowledgements
This work was supported by grants from National Basic Research Program of China (2013CB910503), National Key Projects for Infectious Disease of China (2012ZX10002-012), National Natural Science Foundation of China (31100629, 31270863, 31300671), Program for New Century Excellent Talents in University (NCET-13-0146), Shanghai Rising-Star Program (13QA1400300), Key Project of Science and Technology Commission of Shanghai Municipality (09DZ1950101, 11411951000) and Research Fund for Excellent Doctor of Shanghai Medical College of Fudan University (EZF152309).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Zhang, H., Wang, X., Xu, J. et al. Notch1 activation is a poor prognostic factor in patients with gastric cancer. Br J Cancer 110, 2283–2290 (2014). https://doi.org/10.1038/bjc.2014.135
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2014.135
Keywords
This article is cited by
-
Ubiquilin-4 induces immune escape in gastric cancer by activating the notch signaling pathway
Cellular Oncology (2024)
-
RHBDL2 promotes the proliferation, migration, and invasion of pancreatic cancer by stabilizing the N1ICD via the OTUD7B and activating the Notch signaling pathway
Cell Death & Disease (2022)
-
NOTCH3, a crucial target of miR-491-5p/miR-875-5p, promotes gastric carcinogenesis by upregulating PHLDB2 expression and activating Akt pathway
Oncogene (2021)
-
Non-coding RNAs underlying chemoresistance in gastric cancer
Cellular Oncology (2020)
-
Targeting the Notch1 oncogene by miR-139-5p inhibits glioma metastasis and epithelial-mesenchymal transition (EMT)
BMC Neurology (2018)