Abstract
Background:
Somatostatin receptor 1 (SSTR1) was preferentially methylated in Epstein-Barr virus (EBV)-positive gastric cancer using promoter methylation array. We aimed to analyse the epigenetic alteration and biological function of SSTR1 in EBV-associated gastric cancer (EBVaGC).
Methods:
Promoter methylation was examined by combined bisulphite restriction analysis (COBRA) and pyrosequencing. The biological functions of SSTR1 were evaluated by loss- and gain-of-function assays.
Results:
Promoter hypermethylation of SSTR1 was detected in EBV-positive gastric cancer cell lines (AGS-EBV) with SSTR1 transcriptional silence, but not in EBV-negative gastric cancer cell lines with SSTR1 expression. Expression level of SSTR1 was restored in AGS-EBV by exposure to demethylating agent. Moreover, methylation level of SSTR1 was significantly higher in EBV-positive primary gastric cancers compared with EBV-negative gastric cancers (P=0.004). Knock-down of SSTR1 in gastric cancer cell lines (AGS and BGC823) increased cell proliferation and colony formation ability, and promoted G1 to S-phase transition, enhanced cell migration and invasive ability. In contrast, ectopic expression of SSTR1 in gastric cancer cell lines (MKN28 and MGC803) significantly suppressed cell growth in culture conditions and reduced tumour size in nude mice. The tumour suppressive effect of SSTR1 was associated with upregulation of cyclin-dependent kinase inhibitors (p16, p15, p27 and p21); downregulation of oncogenes (MYC and MDM2), key cell proliferation and pro-survival regulators (PI3KR1, AKT, BCL-XL and MET); and inhibition of the migration/invasion-related genes (integrins, MMP1 (matrix metallopeptidase 1), PLAUR (plasminogen activator urokinase receptor) and IL8 (interleukin 8)).
Conclusion:
Somatostatin receptor 1 is a novel methylated gene driven by EBV infection in gastric cancer cells and acts as a potential tumour suppressor.
Similar content being viewed by others
Main
Epstein-Barr virus (EBV) was first reported to be detected in a subset of gastric cancers in 1992 by the uniform occurrence of EBV in all gastric cancer cells but not in the adjacent normal cells (Shibata and Weiss, 1992). Since then, many reports have showed this strong association and the role of EBV in gastric carcinogenesis has been recognised as new evidence (Herrmann and Niedobitek, 2003; Zur Hausen et al, 2004). EBV-associated gastric cancer (EBVaGC) harbours distinct chromosomal aberrations and is characterised by a unique transcription pattern that resembles but is not identical to that of nasopharyngeal carcinomas (NPC) (Imai et al, 1994). It shows distinct clinicopathological features compared with EBV-negative gastric carcinoma (Uozaki and Fukayama, 2008). These findings suggest that EBV has an important role in the development of EBV-positive gastric carcinomas. Gastric cancer is one of the most common malignance, and the worldwide occurrence of EBV-positive gastric carcinoma is estimated at >90 000 patients annually (Fukayama et al, 2008). However, the oncogenic role of EBV in gastric cancer development remains largely unknown.
Recent studies indicated that epigenetic alterations, particularly promoter methylation of tumour suppressor genes were demonstrated more frequently in EBV-positive than in EBV-negative gastric cancer (Kaneda et al, 2012). Moreover, the mechanism of promoter methylation in association with EBV infection was also studied. DNA methyltransferase (DNMT), which is considered to have a key role in methylation in mammals, was reported to be activated by EBV infection in gastric cancer (Hino et al, 2009). Our previous study demonstrated that EBV infection induced the activation of DNMT3b and caused genome-wide methylation in a gastric cancer cell line (Zhao et al, 2012). Epithelial cells are refractory to EBV infection in vitro. This has hampered the study of the role of EBV in epithelial malignancies. The use of recombinant EBV-infected immortalised gastric epithelial cell model with stable EBV infection (AGS-EBV) has enabled this difficulty to be overcome. This cell model facilitated us for a genome-wide scan of promoter methylated genes to identify the EBV-associated methylation candidates by comparing AGS-EBV with its parental AGS cells using the methylated DNA immunoprecipitation microarray (MeDIP-chip) (Zhao et al, 2013). Of note, 886 candidates were detected with promoter hypermethylation, and one of them named as Somatostatin receptor 1 (SSTR1) was validated to be a novel CpG hypermethylated gene in EBVaGC (Zhao et al, 2013), Methylation level of SSTR1 is eight-fold higher in AGS-EBV cells as compared with AGS cells using MeDIP-chip assay (Zhao et al, 2013).
SSTR genes belong to G protein-coupled receptors family (Patel et al, 1995). They are crucial in regulating the growth inhibitory effect of somatostatin and reducing the tumour cells growth. SSTR1 is located on chromosome 14q13 and its mRNA is widely distributed in human tissues including stomach (Patel, 1999). Loss of SSTR1 has been found in pancreatic cancer, and overexpression of SSTR1 in pancreatic cancer cell lines induced cell-cycle arrest and inhibited tumour cell proliferation (Li et al, 2005, 2008). However, the role of SSTR1 in gastric cancer remains elusive. In this study, the epigenetic regulation, biological function, molecular mechanism and clinical application of SSTR1 in EBVaGC were examined.
Materials and methods
Cancer cell lines and culture condition
Gastric cancer cell lines (AGS, AGS-EBV, BGC823, MGC803, MKN28 and MKN45) were used in this study. AGS-EBV, an EBV-infected gastric cancer cell line (Feng et al, 2002), was a gift from Dr Shannon C. Kenney (Department of Oncology and Medicine, McArdle Laboratory for Cancer Research at the University of Wisconsin, Madison, Wisconsin). MKN28 and MKN45 were obtained from Riken Cell Bank (Tsukuba, Japan). BGC823 and MGC803 were gifts from Oncology Hospital, Beijing University, China. AGS was purchased from American Type Culture Collection (Manassas, VA, USA). The DNA samples isolated from five NPC cell lines (C666-1, CNE1, HK1, HONE1 and HNE1) and one immortalised normal nasopharyngeal epithelial cell line NP69 were gifts from Department of Clinical Oncology, the Chinese University of Hong Kong.
Human samples
Gastric cancer tissue samples including 12 EBV-positive gastric cancers and 14 EBV-negative gastric cancers, and 4 normal gastric biopsies were obtained from Prince Wales of Hospital, The Chinese University of Hong Kong, Hong Kong. All patients and controls gave informed consent for participation in this study and the study protocol was approved by the Ethics Committee of the Chinese University of Hong Kong.
Demethylation with 5-Aza-2′deoxycytidine agent treatment
Gastric cancer cells were treated with 2 μ M DNA demethylation agent 5-Aza-2′deoxycytidine (5-Aza) (Sigma-Aldrich, St Louis, MO, USA) for 5 days and medium was refreshed every day.
Combined bisulphite restriction analysis
Combined bisulphite restriction analysis (COBRA) is performed to determine methylation levels at specific gene loci in genomic DNA after sodium bisulphite conversion by restriction enzyme digestion. Amplification of PCR was performed with 2 μl bisulphite-converted DNA. The PCR products were digested with BstU I (New England Biolabs, Ipswich, MA, USA) and separated on 2% agarose gels.
Pyrosequencing
Pyrosequencing is a loci-specific quantitative method, which is based on sequencing-by-synthesis (Tost and Gut, 2007a). The methylation percentage of each CpG site was calculated by PyroMark CpG SW 1.0 software (Qiagen, Hilden, Germany). The peak showed the ratio of cytosine to thymine at each analysed CpG site, reflecting the proportion of methylated DNA (Tost and Gut, 2007b).
In situ hybridisation for EBV-encoded small RNA
To examine the EBV infection in gastric cancer tissues, detection of EBV-encoded small RNA (EBER) was carried out as reported by us (Zhao et al, 2012).
Cell viability assay
Cell viability was assessed by the MTT assay (Promega, Madison, MI, USA) (Zhao et al, 2012). The experiments were performed in triplicate for three times.
Colony formation assay
Colony formation was performed as described previously (Zhao et al, 2012). The experiments were performed in triplicate for three times.
Cell-cycle analysis
About 50 000 propidium iodide-stained cells were counted and sorted by FACS Calibur Flow Cytometer (BD Biosciences, Franklin Lakes, NJ, USA) and cell-cycle distributions were analysed using the ModFitLT software (BD Biosciences) (Zhao et al, 2012).
Cell migration assay
Cellular migration was evaluated using wound-healing assay in triplicate for three independent experiments.
Invasion assay
Invasion ability of gastric cells was determined using Matrigel Invasion chambers (BD Biosciences).
Human cancer pathway finder RT2 profiler PCR array analysis
Gene expression profiles of gastric cancer cell lines stably transfected with sh-SSTR1 or sh-ctrl plasmid were analysed by the Human Cancer PathwayFinder RT2 Profiler PCR Array (Qiagen), which contained 84 well-characterised genes with representative roles in tumorigenesis.
In vivo tumorigenicity
Gastric cancer cell line MGC803 (1 × 106 cells in 0.1 ml PBS) stably transfected with SSTR1 expression vector or empty vector was injected subcutaneously into the dorsal flank of 4-week-old male Balb/c nude mice (n=9/group). Tumour diameter was measured every 4 days until 24 days. Animal experimental procedures were approved by the Animal Ethics Committee of the Chinese University of Hong Kong.
Statistical analysis
The results were expressed as mean±standard deviation (s.d.). Mann–Whitney U test was performed to compare the variables of the two sample groups. Receiver Operating Characteristic (ROC) curve was used to estimate the cutoff value of the methylation percentage. The difference in tumour growth rate between the two groups of nude mice was determined by repeated-measures analysis of variance. Value of P<0.05 was taken as statistical significance.
Results
SSTR1 was a novel EBV-driven methylated gene in gastric cancer
SSTR1 was reduced in EBV-positive cell lines AGS-EBV, while it was expressed in EBV-negative cell lines AGS, BGC823 and MKN45 as well as normal gastric tissues (Figure 1A). We validated the SSTR1 methylation status in both EBV-positive and EBV-negative gastric cancer cells using COBRA. CpG hypermethylation was detected in EBV-positive AGS-EBV cells with SSTR1 downregulation, whereas methylation was not found in EBV-negative gastric cancer cell lines including AGS, BGC823 and MKN45 cells which expressed SSTR1 (Figure 1A). We then treated AGS-EBV and AGS cell lines with DNA demethylation agent 5-Aza. The SSTR1 mRNA expression was restored in AGS-EBV cells, but not in AGS cells by 5-Aza treatment (Figure 1B), indicating that the transcriptional silence of SSTR1 in AGS-EBV is mediated by its promoter methylation. The SSTR1 methylation status was further evaluated and compared in AGS-EBV and AGS by pyrosequencing, as shown in Figure 1C, promoter methylation level of SSTR1 was significantly higher in AGS-EBV than in AGS (31.25±4.03% vs 1.25±0.5%, P<0.0001).
(A ) SSTR1 mRNA expression was determined by RT–PCR. Promoter methylation of SSTR1 was detected by combined bisulphite restriction analysis (COBRA). U=unmethylation; M=methylation. (B) SSTR1 mRNA expression was restored after treatment with demethylation reagent 5-Aza in AGS-EBV. (C) (Upper panel) Diagram of SSTR1 CpG island. Each vertical red bar represents one CpG site. (Lower panel) Average methylaiton levels of SSTR1 in AGS-EBV and in AGS by pyrosequencing. (D, 1) Representative image of EBV infection in gastric cancer detected by in situ hybridisation for Epstein-Barr virus-encoded RNA (EBER). Dark brown nuclear staining indicates a positive hybridisation signal. (2) SSTR1 methylation was determined in primary EBV-positive and EBV-negative gastric cancers by pyrosequencing. (3) Receiver operating characteristics (ROC) curve analysis of the correlation between SSTR1 methylation and EBV infection in primary gastric cancers.
SSTR1 hypermethylation was associated with EBV-positive primary gastric cancer
To verify the correlation between SSTR1 methylation and EBV infection, SSTR1 methylation status was compared in primary EBV-positive and EBV-negative gastric cancers by pyrosequencing. The EBV infection in gastric cancer tissues was confirmed by EBER in situ hybridisation (Figure 1D1). Promoter methylation level of SSTR1 was significantly higher in EBV-positive gastric cancers (15.04±8.69%) than in EBV-negative gastric cancers (6.93±3.01%) (P=0.004) as determined by pyrosequencing (Figure 1D2).
The ROC curve analysis indicated that a cutoff value of 9.675% SSTR1 methylation status in EBV-positive gastric cancers with a sensitivity and specificity of 75% and 85.7%, respectively (AUC=0.777; 95% CI=0.579∼0.974) (Figure 1D3). Using the cutoff value of 9.675% SSTR1 methylation, the association between clinicopathologic features of gastric cancers and the methylation levels of SSTR1 was evaluated. The SSTR1 methylation was associated with male gender (P=0.024) and EBER-positive staining (P<0.005) (Table 1), indicating a positive correlation between SSTR1 methylation and EBV infection.
SSTR1 knock-down induced cell proliferation in gastric cancer cell lines
To investigate the biological function of SSTR1 in gastric cancer, we first examined the effect of SSTR1 knock-down on cell growth through RNA interference in AGS and BGC823 cells, which showed high expression of SSTR1. Successful SSTR1 knock-down by stable transfection with shRNA-SSTR1 plasmid was confirmed by real-time qRT–PCR and western blot (Figure 2A). Knock-down of SSTR1 significantly promoted cell viability both in AGS (P<0.001) and in BGC823 (P<0.05) compared with the control cells (Figure 2B). The growth enhancive effect of SSTR1 knock-down was further proved by colony formation assay. The colonies formed by shRNA-SSTR1 transfected cells were significantly more in number and larger in size both in AGS (224.1±54.8% increase, P<0.01) and in BGC823 (52.6±9.1% increase, P<0.05) as compared with those formed by control shRNA-transfected cells (Figure 2C).
SSTR1 knock-down increased gastric cancer cell growth. (A) Knock-down of SSTR1 was evidenced at mRNA (1) and protein (2) level by RT–PCR and western blot, respectively. (B) SSTR1 knock-down increased cell proliferation in cancer cell lines. (C) Representative dishes of colony formation. Quantitative analyses of colony numbers indicated SSTR1 knock-down significantly increased clonogenicity in both AGS (224.1±54.8% increase, P<0.001) and BGC823 (52.6±9.1% increase, P<0.05).
SSTR1 knock-down promoted cells to enter into S phase
We investigated the effect of SSTR1 on cell-cycle regulation by flow cytometry. Knock-down of SSTR1 led to significant decrease in the number of cells accumulating in the G1 phase of AGS (P<0.01) and BGC823 (P<0.001) compared with the control groups (Figure 3A). Concomitantly, there were significant increases in the number of the S-phase cells of AGS (P<0.001) and BGC823 (P<0.001) (Figure 3A). These results indicated that knock-down of SSTR1 induced cancer cell growth by promoting cells to enter into S phase, which was confirmed by the reduced protein expression of key G1 checkpoint regulators including cyclin-dependent inhibitors p21, p27 and p15 (Figure 3B).
Knock-down of SSTR1 promoted cell-cycle progression. (A) The cell-cycle proportion was analysed using flow cytometry in AGS and BGC823 cells transfected with sh-control and sh-SSTR1, respectively. Quantitative analyses on the fraction of cells indicated significant differences between control and SSTR1 knock-down cells in cell-cycle phase distribution of G1 (AGS: P<0.01, BGC823: P<0.0001) and S (AGS: P<0.001, BGC823: P<0.001) phases. The data are mean±s.d. of three independent experiments. (B) Effects of SSTR1 knock-down on protein expression of cell-cycle regulators p15, p21 and p27 by western blot.
SSTR1 knock-down increased migration and invasion ability of gastric cancer cells
Stable knock-down of SSTR1 markedly accelerated cell migration at the edges of scratch wound of AGS and BGC823 cells (Figure 4A). Quantitative analyses at 24 h showed significant increases in wound closure in AGS (4.3±0.1-fold, P<0.001) and in BGC823 (1.2±0.0-fold, P<0.01) cells transfected with sh-SSTR1 compared with the control cells (Figure 4A). Stable knock-down of SSTR1 also significantly increased the invasiveness of both AGS (2.5±0.2-fold, P<0.001) and BGC823 (1.9±0.4-fold, P<0.01) cells (Figure 4B).
Ectopic expression of SSTR1 inhibited proliferation and clonogenicity in gastric cancer cells
The effects of SSTR1 in gastric cancer were further examined by gain-of-function study, MKN28 and MGC803 cells were transfected with either an SSTR1 expression construct (pcDNA3.1-SSTR1) or an empty vector (pcDNA3.1). Ectopic expression of SSTR1 in these cells was confirmed by RT–PCR and western blot (Figure 5A). The SSTR1 significantly decreased cell viability both in MKN28 (P<0.001) and in MGC803 (P<0.001) cells compared with the empty vector-transfected cells (Figure 5B). In addition, the colonies formed by SSTR1-transfected cells were dramatically fewer and smaller in MKN28 (74.5±2.8% decrease, P<0.01) and in MGC803 (68.8±10.9% decrease, P<0.05) (Figure 5C).
Ectopic expression of SSTR1 inhibited gastric cancer cell growth. (A) Ectopic expression of SSTR1 in MKN28 and MGC803 cell lines was evidenced by RT–PCR and western blot, respectively. (B) SSTR1 significantly suppressed the cell viability. (C) SSTR1 inhibited tumour cell clonogenicity of MKN28 (74.5±2.8% decrease, P<0.01) and MGC803 (68.8±10.9% decrease, P<0.01) by colony formation assay. (D) SSTR1 inhibits growth of xenograft tumours derived from MGC803 in vivo (n=9/group).
To assess whether the level of SSTR1 gene expression affects EBV gene expression, we examined the expression of the immediate early lytic gene BZLF1, which is essential for the latent-lytic switch of EBV, and the representative latent gene EBNA1 (Zhao et al, 2012) in SSTR1-overexpressed and control vector-transfected AGS-EBV cells by qRT–PCR. Results showed that expression of BZLF1 and EBNA1 was not changed by SSTR1 re-expression (Supplementary Figure 1), demonstrating that the level of SSTR1 gene expression does not affect EBV gene expression in EBVaGC.
SSTR1 inhibited xenograft tumour growth in nude mice
We examined whether SSTR1 could suppress the growth of gastric cancer cells in nude mice in vivo. The tumour growth curve of MGC803 cells, stably transfected with SSTR1 expression vector or vector control in nude mice was shown in Figure 5D. The tumour size was significantly smaller in SSTR1-transfected nude mice as compared with the vector control mice (P<0.05).
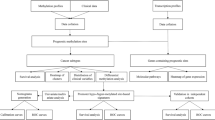
Identification of genes modulated by SSTR1
To gain insight into the molecular mechanism underlying the tumour suppressive effect of SSTR1, gene expression profiles of BGC823 cells with or without stable SSTR1 knock-down were analysed by cDNA microarray. The SSTR1 was found to modulate the expressions of many important genes involved in multiple cellular process, including cell cycle, apoptosis, migration and invasion (Figure 6A). As shown in Figure 6A, SSTR1 induced cyclin-dependent inhibitors p16 (2.5-fold) and inhibited cell divison cycle 25 homologue A (CDC25A) (−6.0-fold) and MYC (−3.26-fold). The SSTR1 also reduced expression of apoptosis regulators, including AKT (−3.19-fold), BCL2-like 1 (BCL-XL) (−10.98-fold), p53 E3 ubiquitin protein ligase homologue (MDM2) (−1.61-fold), met proto-oncogene (MET) (−1.77-fold) and phosphoinositide-3-kinase, regulatory subunit 1 (alpha) (PI3KR1) (−1.51-fold). Morover, SSTR1 significantly downregulated the expression of migration-related genes, including four integrins ITGA1 (−1.51-fold), ITGA2 (−2.51-fold), ITGA3 (−2.20-fold) and ITGB5 (−2.60-fold), interleukin 8 (IL8) (−2.03-fold), matrix metallopeptidase 1 (MMP1) (−4.49-fold) and plasminogen activator urokinase receptor (PLAUR) (−5.54-fold).
(A ) Human cancer pathway cDNA microarray was applied to analyse the molecular basis of SSTR1 as a potential tumour suppressor gene. Downregulated or upregulated genes by SSTR1 are shown. (B) Schematic diagram of the molecular events for SSTR1 function as a tumour suppressor through regulating cell-cycle progression, inhibiting proliferation, inducing apoptosis and suppressing migration/invasion.
Discussion
We found that SSTR1 expression was significantly suppressed in AGS-EBV, while expressed in gastric cancer cells without EBV infection (Figure 1A). The decreased expression of SSTR1 can be reversed by pharmacological demethylation treatment in AGS-EBV (Figure 1B2). Consistent with the high methylation level identified in the promoter region of SSTR1 in AGS-EBV (eight-fold increase) by MeDIP-chip, dense promoter methylation of SSTR1 in AGS-EBV cells was confirmed in this study by COBRA (Figure 1B2). Collectively, these results suggest that promoter hypermethylation is the principle mechanism for inactivation of SSTR1 in AGS-EBV cells.
To determine the methylation status of SSTR1 in EBVaGC in vivo, we compared the promoter methylation levels of SSTR1 by pyrosequencing in EBV-positive and EBV-negative gastric cancers. We found that methylation of SSTR1 was significantly higher in EBV-positive gastric cancer tissues compared with EBV-negative gastric cancer tissues (P=0.004, Figure 1D). In this regard, we examined the association between SSTR1 methylation and the clinical outcome of EBV-positive gastric cancer patients. Our results showed that SSTR1 methylation was significantly associated with male gender (Table 1), which is in line with other observation that EBV-positive gastric cancer was more prevalent in male than in female gastric cancer patients (Koriyama et al, 2005). Moreover, SSTR1 methylation was demonstrated to be correlated with EBER-positive staining in gastric cancer tissues (P=0.004) (Table 1). These results provide important evidence that the promoter methylation of SSTR1 is associated with EBV infection, which may have a crucial role in the development of EBVaGC.
In addition to gastric cancer, there are several other types of EBV-associated cancers, such as NPC and Hodgkin’s lymphoma. Hypermethylation of multiple genes (RASSFIA, SHP1, DAPK, P16, RARβ2, etc.) was reported to be common alterations in NPC, thus epigenetic change may have a role in NPC (Challouf et al, 2012). The genome-wide host gene methylation changes caused by EBV infection in germinal centre B cells indicated that EBV-caused aberrant methylation involves in the pathogenesis of Hodgkin’s lymphoma (Leonard et al, 2011). To evaluate if SSTR1 methylation can also be observed in other EBV-associated cancer, we examined the methylation status of SSTR1 in five NPC cell lines (C666-1, CNE1, HK1, HONE1 and HNE1), and one immortalised normal nasopharyngeal epithelial cell line NP69 by COBRA. We demonstrated that SSTR1 was completely methylated in the EBV-positive NPC cell line C666-1, partially methylated in four other EBV-negative NPC cell lines (CNE1, HK1, HONE1 and HNE1), and unmethylated in NP69 (Supplementary Figure 2). This result suggested that SSTR1 promoter methylation may be a common event in EBV-associated cancer.
The putative tumour suppressor function of SSTR1 in gastric cancer was further examined by both in vitro and in vivo assays. Knock-down of SSTR1 in gastric cancer cell lines significantly induced cell growth by increasing cell viability and clonogenicity (Figure 2B and C). While, ectopic expression of SSTR1 exhibited marked growth-suppressing effect in culture conditions and also reduced tumour size in nude mice (Figure 5). Collectively, these results indicate that SSTR1 functions as a tumour suppressor in gastric cancer. We further revealed the molecular basis of how SSTR1 exerts the tumour suppressor effect in gastric cancer (Figure 6). Using a cDNA microarray, we identified that SSTR1 exerted its tumour suppressive function through inhibiting the key cell proliferation and apoptosis regulators, inducing MDM2, AKT, PI3KR1, BCL-XL and MET. The MDM2 functions as an oncogene and controls the activity of p53 in many human tumours (Momand et al, 2000). After phosphorylation by AKT, MDM2 is activated and localised in the nucleus to induce p53 degradation and cell survival (Jeong et al, 2005). Akt can block apoptosis and thereby promote cell survival. The PI3KR1 recruits the catalytic subunit of PI3K (Hixon et al, 2010). The PI3K-Akt signalling pathway has been implicated as a major pro-survival factor in many types of cancer (Hixon et al, 2010). BCLXL is a member of the anti-apoptotic BCL2 family (Plas and Thompson, 2002). AKT also confers survival signals through phosphorylation of the effector sequestered from BCLXL, leading to cell survival (Flusberg et al, 2001). The MET proto-oncogene has been found in a number of human cancers and has an important role in cancer development through activation of key oncogenic pathways such as PI3K-Akt signalling pathway (Gherardi et al, 2012).
To evaluate the cell-cycle regulation in contributing to the diminution of tumour growth by SSTR1, we performed Flow cytometry analysis of sh-SSTR1-transfected AGS and BGC823. Cell-cycle distribution analysis revealed that knock-down of SSTR1 significantly reduced proportion of cells in the G1 phase, with a concomitant increase of cells in S phase, inferring that SSTR1 knock-down promoted cell-cycle transition from G1 to S phase. To disclose the molecular basis underlying G1-S phase transition by SSTR1, we evaluated expression of the key regulatory factors that control G1-S checkpoint. The increased G1-S phase transition by SSTR1 knock-down was identified to be associated with downregulation of cyclin-dependent kinase inhibitors p15, p16, p21 and p27 and upregulation of MYC and CDC25A (Figure 3C and 6) by western blot and cDNA expression array. The role of p15, p16, p21 and p27 as major players in G1 arrest has been well documented (Sherr, 1996). p21 and p27 are potent inhibitors of cyclin D/Cdk4 and cyclin E/Cdk2 activities; p15 is an important inhibitor of cyclin D/CDK4/6 activity (Sherr, 1996). MYC is an oncogene in human cancers (Alitalo et al, 1987). MYC expression is critical for entry of cells into S phase of cell cycle (Amati and Land, 1994). The CDC25A encodes an important G1-specific protein phosphatase and is required for the cell-cycle initiation and the progression through G1 phase (Zornig and Evan, 1996). The CDC25A has been identified as a direct transcriptional target of MYC and has a pivotal role in regulating MYC and cell cycle (Galaktionov et al, 1996). In addition, AKT negatively regulates p21 and p27 by direct phosphorylation (Rossig et al, 2001; Shin et al, 2002). It has been reported that SSTR1 was silenced in human pancreatic cancer and ectopic expression of SSTR1 caused cell-cycle arrest at the G0/G1 phase and inhibited pancreatic cancer cell proliferation (Li et al, 2005, 2008). Thus, the mechanism of SSTR1 mediated cell-cycle progression is most likely associated with deregulation of cell-cycle regulators in gastric cancer, thereby promoting cell proliferation.
Moreover, ablation of SSTR1 in gastric cancer cells increased migration and invasion (Figure 4). The suppressive effect of SSTR1 on migration and invasion ability is at least due to the downregulation of integrin family member (ITGA1, ITGA2, ITGA3 and ITGB5), and other important migration/invasion-related genes MMP1, PLAUR and IL8 (Figure 6). Integrins take part in cell migration and invasion during tumorigenesis through directly binding to extracellular matrix (ECM) (Guo and Giancotti, 2004). Integrins also regulate cell proliferation and enhance cell survival through activation of PI3K/AKT signalling pathway (Assoian and Klein, 2008). The anti-migration effect by SSTR1 is also attributed to the downregulation of MMP1, PLAUR and IL8. Matrix metallopeptidase 1 belongs to MMPs family of proteolytic enzymes, which degrade the components of ECM (Brinckerhoff and Matrisian, 2002). Matrix metallopeptidases have a crucial role in inducing invasion and migration of tumour cells (Egeblad and Werb, 2002). The PLAUR has the ability to degradate ECM and is associated with wound healing, invasion and metastasis (Ploug et al, 2002). Interleukin 8 is a potential stimulator of neutrophil transendothelial migration (Koch et al, 1992). Thus, the induction of cell invasion and migration by SSTR1 knock-down could be mediated by these downstream effectors of SSTR1 (Figure 6).
In conclusion, we have identified that SSTR1 is a novel EBV-associated promoter hypermethylation gene in gastric cancer. SSTR1 has an important tumour suppressive role in gastric cancer through modulating the expression of the important effectors involved in the regulation of cell proliferation, apoptosis, cell cycle and invasion. Epigenetic silencing of SSTR1 by EBV infection may contribute to the pathogenesis of EBV-associated gastric cancer.
Change history
25 June 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Alitalo K, Koskinen P, Makela TP, Saksela K, Sistonen L, Winqvist R (1987) myc oncogenes: activation and amplification. Biochim Biophys Acta 907: 1–32.
Amati B, Land H (1994) Myc-Max-Mad: a transcription factor network controlling cell cycle progression, differentiation and death. Curr Opin Genet Dev 4: 102–108.
Assoian RK, Klein EA (2008) Growth control by intracellular tension and extracellular stiffness. Trends Cell Biol 18: 347–352.
Baudino TA, Cleveland JL (2001) The Max network gone mad. Mol Cell Biol 21: 691–702.
Brinckerhoff CE, Matrisian LM (2002) Matrix metalloproteinases: a tail of a frog that became a prince. Nat Rev Mol Cell Biol 3: 207–214.
Challouf S, Ziadi S, Zaghdoudi R, Ksiaa F, Ben Gacem R, Trimeche M (2012) Patterns of aberrant DNA hypermethylation in nasopharyngeal carcinoma in Tunisian patients. Clin Chim Acta 413: 795–802.
Egeblad M, Werb Z (2002) New functions for the matrix metalloproteinases in cancer progression. Nat Rev Cancer 2: 161–174.
Feng WH, Israel B, Raab-Traub N, Busson P, Kenney SC (2002) Chemotherapy induces lytic EBV replication and confers ganciclovir susceptibility to EBV-positive epithelial cell tumors. Cancer Res 62: 1920–1926.
Flusberg DA, Numaguchi Y, Ingber DE (2001) Cooperative control of Akt phosphorylation, bcl-2 expression, and apoptosis by cytoskeletal microfilaments and microtubules in capillary endothelial cells. Mol Biol Cell 12: 3087–3094.
Fukayama M, Hino R, Uozaki H (2008) Epstein-Barr virus and gastric carcinoma: virus-host interactions leading to carcinoma. Cancer Sci 99: 1726–1733.
Galaktionov K, Chen X, Beach D (1996) Cdc25 cell-cycle phosphatase as a target of c-myc. Nature 382: 511–517.
Gherardi E, Birchmeier W, Birchmeier C, Vande Woude G (2012) Targeting MET in cancer: rationale and progress. Nat Rev Cancer 12: 89–103.
Guo W, Giancotti FG (2004) Integrin signalling during tumour progression. Nat Rev Mol Cell Biol 5: 816–826.
Herrmann K, Niedobitek G (2003) Epstein-Barr virus-associated carcinomas: facts and fiction. J Pathol 199: 140–145.
Hino R, Uozaki H, Murakami N, Ushiku T, Shinozaki A, Ishikawa S, Morikawa T, Nakaya T, Sakatani T, Takada K, Fukayama M (2009) Activation of DNA methyltransferase 1 by EBV latent membrane protein 2A leads to promoter hypermethylation of PTEN gene in gastric carcinoma. Cancer Res 69: 2766–2774.
Hixon ML, Paccagnella L, Millham R, Perez-Olle R, Gualberto A (2010) Development of inhibitors of the IGF-IR/PI3K/Akt/mTOR pathway. Rev Recent Clin Trials 5: 189–208.
Imai S, Koizumi S, Sugiura M, Tokunaga M, Uemura Y, Yamamoto N, Tanaka S, Sato E, Osato T (1994) Gastric carcinoma: monoclonal epithelial malignant cells expressing Epstein-Barr virus latent infection protein. Proc Natl Acad Sci USA 91: 9131–9135.
Jeong SJ, Pise-Masison CA, Radonovich MF, Park HU, Brady JN (2005) Activated AKT regulates NF-kappaB activation, p53 inhibition and cell survival in HTLV-1-transformed cells. Oncogene 24: 6719–6728.
Kaneda A, Matsusaka K, Aburatani H, Fukayama M (2012) Epstein-Barr virus infection as an epigenetic driver of tumorigenesis. Cancer Res 72: 3445–3450.
Koch AE, Polverini PJ, Kunkel SL, Harlow LA, DiPietro LA, Elner VM, Elner SG, Strieter RM (1992) Interleukin-8 as a macrophage-derived mediator of angiogenesis. Science 258: 1798–1801.
Koriyama C, Akiba S, Minakami Y, Eizuru Y (2005) Environmental factors related to Epstein-Barr virus-associated gastric cancer in Japan. J Exp Clin Cancer Res 24: 547–553.
Leonard S, Wei W, Anderton J, Vockerodt M, Rowe M, Murray PG, Woodman CB (2011) Epigenetic and transcriptional changes which follow Epstein-Barr virus infection of germinal center B cells and their relevance to the pathogenesis of Hodgkin's lymphoma. J Virol 85: 9568–9577.
Li M, Wang X, Li W, Li F, Yang H, Wang H, Brunicardi FC, Chen C, Yao Q, Fisher WE (2008) Somatostatin receptor-1 induces cell cycle arrest and inhibits tumor growth in pancreatic cancer. Cancer Sci 99: 2218–2223.
Li M, Zhang R, Li F, Wang H, Kim HJ, Becnel L, Yao Q, Chen C, Fisher WE (2005) Transfection of SSTR-1 and SSTR-2 inhibits Panc-1 cell proliferation and renders Panc-1 cells responsive to somatostatin analogue. J Am Coll Surg 201: 571–578.
Momand J, Wu HH, Dasgupta G (2000) MDM2--master regulator of the p53 tumor suppressor protein. Gene 242: 15–29.
Patel YC (1999) Somatostatin and its receptor family. Front Neuroendocrinol 20: 157–198.
Patel YC, Greenwood MT, Panetta R, Demchyshyn L, Niznik H, Srikant CB (1995) The somatostatin receptor family. Life Sci 57: 1249–1265.
Plas DR, Thompson CB (2002) Cell metabolism in the regulation of programmed cell death. Trends Endocrinol Metab 13: 75–78.
Ploug M, Gardsvoll H, Jorgensen TJ, Lonborg Hansen L, Dano K (2002) Structural analysis of the interaction between urokinase-type plasminogen activator and its receptor: a potential target for anti-invasive cancer therapy. Biochem Soc Trans 30: 177–183.
Rossig L, Jadidi AS, Urbich C, Badorff C, Zeiher AM, Dimmeler S (2001) Akt-dependent phosphorylation of p21(Cip1) regulates PCNA binding and proliferation of endothelial cells. Mol Cell Biol 21: 5644–5657.
Sherr CJ (1996) Cancer cell cycles. Science 274: 1672–1677.
Shibata D, Weiss LM (1992) Epstein-Barr virus-associated gastric adenocarcinoma. Am J Pathol 140: 769–774.
Shin I, Yakes FM, Rojo F, Shin NY, Bakin AV, Baselga J, Arteaga CL (2002) PKB/Akt mediates cell-cycle progression by phosphorylation of p27(Kip1) at threonine 157 and modulation of its cellular localization. Nat Med 8: 1145–1152.
Tost J, Gut IG (2007a) Analysis of gene-specific DNA methylation patterns by pyrosequencing technology. Methods Mol Biol 373: 89–102.
Tost J, Gut IG (2007b) DNA methylation analysis by pyrosequencing. Nat Protoc 2: 2265–2275.
Uozaki H, Fukayama M (2008) Epstein-Barr virus and gastric carcinoma—viral carcinogenesis through epigenetic mechanisms. Int J Clin Exp Pathol 1: 198–216.
Zhao J, Jin H, Cheung KF, Tong JH, Zhang S, Go MY, Tian L, Kang W, Leung PP, Zeng Z, Li X, To KF, Sung JJ, Yu J (2012) Zinc finger E-box binding factor 1 plays a central role in regulating Epstein-Barr virus (EBV) latent-lytic switch and acts as a therapeutic target in EBV-associated gastric cancer. Cancer 118: 924–936.
Zhao J, Liang Q, Cheung KF, Kang W, Lung RW, Tong JH, To KF, Sung JJ, Yu J (2013) Genome-wide identification of Epstein-Barr virus-driven promoter methylation profiles of human genes in gastric cancer cells. Cancer 119: 304–312.
Zornig M, Evan GI (1996) Cell cycle: on target with Myc. Curr Biol 6: 1553–1556.
Zur Hausen A, van Rees BP, van Beek J, Craanen ME, Bloemena E, Offerhaus GJ, Meijer CJ, van den Brule AJ (2004) Epstein-Barr virus in gastric carcinomas and gastric stump carcinomas: a late event in gastric carcinogenesis. J Clin Pathol 57: 487–491.
Acknowledgements
This project was supported by research funds of RFCID (11100022 and 10090942), China 973 Program (2010CB529305), China 863 Program (2012AA02A504), CUHK Focused Investments (2041423) and China National Science and Technology Major Projects (2011ZX09307-001-05).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Zhao, J., Liang, Q., Cheung, KF. et al. Somatostatin Receptor 1, a novel EBV-associated CpG hypermethylated gene, contributes to the pathogenesis of EBV-associated gastric cancer. Br J Cancer 108, 2557–2564 (2013). https://doi.org/10.1038/bjc.2013.263
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.263
Keywords
This article is cited by
-
Targeting the signaling in Epstein–Barr virus-associated diseases: mechanism, regulation, and clinical study
Signal Transduction and Targeted Therapy (2021)
-
Expression of potential therapeutic target SSTR2a in primary and metastatic non-keratinizing nasopharyngeal carcinoma
Virchows Archiv (2020)
-
An orthotopic mouse model of gastric cancer invasion and metastasis
Scientific Reports (2018)
-
Epigenetic reprogramming using 5-azacytidine promotes an anti-cancer response in pancreatic adenocarcinoma cells
Cell Death & Disease (2018)
-
REC8 functions as a tumor suppressor and is epigenetically downregulated in gastric cancer, especially in EBV-positive subtype
Oncogene (2017)