Abstract
Erythropoiesis-stimulating agents (ESAs) increase red blood cell (RBC) production in bone marrow by activating the erythropoietin receptor (EpoR) on erythrocytic-progenitor cells. Erythropoiesis-stimulating agents are approved in the United States and Europe for treating anaemia in cancer patients receiving chemotherapy based on randomised, placebo-controlled trials showing that ESAs reduce RBC transfusions. Erythropoiesis-stimulating agent-safety issues include thromboembolic events and concerns regarding whether ESAs increase disease progression and/or mortality in cancer patients. Several trials have reported an association between ESA use and increased disease progression and/or mortality, whereas other trials in the same tumour types have not provided similar findings. This review thoroughly examines available evidence regarding whether ESAs affect disease progression. Both clinical-trial data on ESAs and disease progression, and preclinical data on how ESAs could affect tumour growth are summarised. Preclinical topics include (i) whether tumour cells express EpoR and could be directly stimulated to grow by ESA exposure and (ii) whether endothelial cells express EpoR and could be stimulated by ESA exposure to undergo angiogenesis and indirectly promote tumour growth. Although assessment and definition of disease progression vary across studies, the current clinical data suggest that ESAs may have little effect on disease progression in chemotherapy patients, and preclinical data indicate a direct or indirect effect of ESAs on tumour growth is not strongly supported.
Similar content being viewed by others
Main
Anaemia is often associated with chemotherapy treatment because of the myelosuppressive effects of chemotherapy and/or the cancer disease itself (Groopman and Itri, 1999; Ludwig et al, 2004). As anaemia can lead to fatigue and decreased quality of life (Cella et al, 2004), its management is important for patient care. Anaemia therapies include red blood cell (RBC) transfusions and erythropoiesis-stimulating agents (ESAs), which increase RBC production in bone marrow by activating the erythropoietin receptor (EpoR) on erythrocytic-progenitor cells (Egrie et al, 1986, 2003). Transfusions quickly increase haemoglobin levels but are associated with risks such as transmission of infectious pathogens and transfusion-related acute-lung injury (Klein et al, 2007). Large, placebo-controlled clinical trials have shown that ESAs decrease transfusion rates in cancer patients (Littlewood et al, 2001; Vansteenkiste et al, 2002; Hedenus et al, 2003). Based on these trials, ESAs such as epoetin alfa and darbepoetin alfa are approved in the United States (Amgen, 2011; Centocor Ortho Biotech Products, 2011) and other countries (EMEA, 2011; eMC, 2011) for treating anaemia in patients with non-myeloid malignancies receiving chemotherapy. Additional ESAs are approved outside the United States for this indication (Jelkmann, 2010).
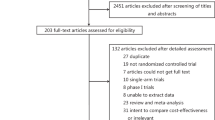
Clinical and preclinical research has examined the benefits and risks associated with ESA use. Although ESAs decrease transfusions, they are associated with an increase in thromboembolic events (Bennett et al, 2008; Glaspy et al, 2010). The potential for ESAs to affect disease progression and/or mortality in cancer patients has also been of concern (Bennett et al, 2008; Bohlius et al, 2009; Tonelli et al, 2009; Glaspy et al, 2010). To better understand ESA-related safety issues, several recent large meta-analyses have examined how ESAs affect thromboembolic events and mortality. Disease progression, however, was not always addressed (Bennett et al, 2008; Bohlius et al, 2009). Difficulties in analysing disease progression include variation in endpoints (e.g., progression-free survival, locoregional control, tumour response, etc.) and varying quality of disease-assessment measurements. Nonetheless, understanding if and how ESAs impact disease progression are key issues. This narrative review discusses clinical-trial data regarding ESAs and disease progression as well as preclinical research regarding how ESAs could affect disease progression at a cellular/molecular level.
Erythropoiesis-stimulating agents and disease progression: evidence from clinical trials
As anaemia is an independent-risk factor for mortality in many cancer types (Caro et al, 2001), one question of interest was whether treating anaemia with ESAs improves cancer-patient survival. Higher haemoglobin levels were postulated to enhance tumour-tissue oxygenation, leading to increased chemotherapy and/or radiotherapy efficacy (Hadland and Longmore, 2009). Though some preclinical (Thews et al, 1998; Mittelman et al, 2001) and early clinical data (Littlewood et al, 2001; Vansteenkiste et al, 2002) suggested an ESA-associated survival benefit, other trials suggested that ESAs increased disease progression and/or mortality. Currently, the ESA-product labelling (Amgen, 2011; Centocor Ortho Biotech Products, 2011; EMEA, 2011; eMC, 2011) describes eight clinical trials of concern that suggest ESA use increases disease progression and/or mortality in cancer patients (Table 1). Two studies were performed in the non-indicated setting of radiotherapy treatment only (Henke et al, 2003; Overgaard et al, 2010), two in the non-indicated anaemia-of-cancer setting (patients received neither chemotherapy nor radiotherapy) (Wright et al, 2007; Smith et al, 2008) and four in the indicated chemotherapy setting (Hedenus et al, 2003; Leyland-Jones et al, 2005; Thomas et al, 2008; Untch et al, 2011b). As these eight studies are a focus for concerns regarding ESAs, they are described in more detail below according to their oncology setting.
Radiotherapy only setting
The Erythropoietin in Head and Neck Cancer (ENHANCE) study was one of the first clinical trials to raise concerns about ESAs and disease progression (Table 1) (Henke et al, 2003). In this study, head and neck cancer patients scheduled to receive radiotherapy only (N=351) were randomised to placebo or epoetin beta 300IU kg−1 3 × weekly. This study tested whether using ESAs to increase haemoglobin to ⩾14 g dl−1 would enhance curative radiation by improving tumour oxygenation. An intent-to-treat analysis stratified by cancer stage and treatment indicated that ESA-treated patients experienced increased locoregional progression (relative risk (RR)=1.69; 95% CI: 1.16–2.47; P=0.007) and decreased survival (RR=1.39; 95% CI: 1.05–1.84; P=0.02). However, results analysed ‘per protocol’ indicated no significant effect of ESAs on disease progression. Study limitations included multiple protocol violations and imbalances in some baseline characteristics (e.g., more ESA-treated patients had relapsed cancer and were smokers). A post-hoc analysis of EpoR expression in tumour cells from ESA-treated and control patients suggested that locoregional progression-free survival was poorer in ESA-treated patients with EpoR-positive tumours (Henke et al, 2006). However, the EpoR antibody used was later shown to be non-specific because of cross-reactivity with heat-shock proteins (Elliott et al, 2006; Brown et al, 2007).
The Danish Head and Neck Cancer-10 (DAHANCA-10) study in head and neck cancer patients receiving radiotherapy only evaluated whether using darbepoetin alfa (150 μg weekly) to maintain haemoglobin between 14.5 and 15.5 g dl−1 could improve the effect of primary-curative radiotherapy (Overgaard et al, 2010). Study outcomes were recently reported (Overgaard et al, 2010) but have yet to be published in a manuscript. Overall, results from 514 patients showed poorer disease progression and survival outcomes in the darbepoetin arm. The RR was 1.51 (95% CI: 1.05–2.17) for 5-year locoregional control, 1.52 (95% CI: 1.07–2.16) for disease-free survival, and 1.39 (95% CI: 0.98–1.97) for overall survival (Overgaard et al, 2010).
Although the ENHANCE and DAHANCA-10 trials suggested ESA use increases disease progression, this finding was not replicated in two randomised, controlled trials in the radiotherapy setting for the treatment of patients with head and neck cancer (Table 1). The Radiation Therapy Oncology Group (RTOG 99-03) trial that evaluated 40 000 IU weekly erythropoietin (Epo) to maintain haemoglobin between 9.0 and 13.5 g dl−1 (Machtay et al, 2007) and the controlled EPO-GBR-7 trial (Hoskin et al, 2009) that evaluated 10 000 IU three times weekly epoetin alfa (haemoglobin <12.5 g/dl) or 4000 IU three times weekly epoetin alfa (haemoglobin ⩾12.5 g dl−1), did not show ESA use increased disease progression. Nonetheless, based on the ENHANCE and DAHANCA-10 studies, the ESA-product labelling does not recommend ESA use in the radiotherapy-only setting.
Anaemia of cancer setting
The EPO-CAN-20 study evaluated non-small cell lung cancer patients randomised to epoetin alfa (40 000 IU weekly) or placebo (Wright et al, 2007). Enrolled patients received neither chemotherapy nor radiotherapy, although this was not stipulated in the trial design. An unplanned-interim analysis (N=66) indicated that ESA use increased mortality (hazard ratio (HR)=1.84; 95% CI: 1.01–3.35; P=0.04). Though the target study size was 300 patients, concerns about ESA-associated mortality led to study termination after 70 patients were randomised. Final results indicated that death occurred in 32 out of 33 patients receiving ESA and in 34 out of 37 patients receiving placebo. Kaplan–Meier curves of overall survival indicated that the median time to death favored placebo treatment (131 days) compared with ESA (68 days; P=0.04). Disease progression data were not formally collected.
The AMG 20010103 study evaluated 985 patients with non-myeloid malignancies and anaemia of cancer randomised to receive darbepoetin alfa (6.75 μg kg−1 every 4 weeks) or placebo (Smith et al, 2008). No disease progression data were collected per study protocol, but a mortality analysis adjusted for stratification factors that impact ESA response indicated increased mortality in the ESA arm (HR=1.22; 95% CI: 1.03–1.45; P=0.022) (Smith et al, 2008). However, exploratory analyses (adjusted for baseline imbalances or known prognostic factors and for stratification factors that impact ESA response) diminished the mortality HR and statistical significance (HR=1.15; 95% CI: 0.97–1.37; P=0.121), suggesting that the possible negative effect of ESAs did not apply to all patient subsets. Of note, the mortality HR (95% CI) was 0.95 (0.73–1.23) for female patients compared with 1.32 (1.05–1.66) for male patients; however, the interaction between sex and treatment group was not statistically significant (P=0.066) (Smith et al, 2008).
Based on mortality data from the EPO-CAN-20 and AMG 20010103 studies, the ESA-product labelling does not recommend ESA use in the anaemia-of-cancer setting.
Chemotherapy setting
The Breast Cancer Erythropoietin Survival Trial (BEST) was one of the first chemotherapy studies to report an association between increased mortality and ESA use (Leyland-Jones et al, 2005). Patients (N=939) with metastatic breast cancer were randomised to either epoetin alfa (40 000 IU weekly) or placebo as needed for up to 12 months; haemoglobin levels were maintained between 12 and 14 g dl−1. Although the target sample size was achieved, an independent data-monitoring committee recommended early termination of study-drug administration because of an interim analysis that indicated higher mortality in the ESA arm. In an intent-to-treat analysis adjusted for demographic and prognostic factors, mortality was reported as significantly higher in the ESA arm at 12 months (HR=1.36; 95% CI: 1.053–1.753; P=0.02). However, no difference in progression-free survival was observed (HR=1.00; P=0.98). An article written on behalf of the BEST investigators suggested that study-design issues (including possible imbalances in risk factors between study arms) (Leyland-Jones, 2003) may have prevented a conclusive interpretation of trial results. In addition, understanding the disease progression results may have been hampered by lack of prespecified tumour assessments at study entry, during the study, and during follow-up (Johnson and Johnson Pharmaceutical Research and Development LLC, 2004).
The AMG 20000161 study evaluated patients with lymphoproliferative malignancies receiving chemotherapy (N=344), who were randomised to receive darbepoetin alfa (2.25 μg kg−1 weekly) or placebo for 12 weeks. The target haemoglobin level was 13–14 g dl−1 for women and 13–15 g dl−1 for men (Hedenus et al, 2003). The protocol was amended to allow collection of long-term follow-up data for survival and disease progression. Hedenus et al (2003) reported that after a median follow-up of 11 months, an initial analysis of long-term data indicated no difference between treatment groups for disease progression or death. After a median follow-up of 29 months, a prespecified analysis indicated higher mortality rates in ESA-treated patients (HR=1.36; 95% CI: 1.02–1.82) (Amgen, 2011). Erythropoiesis-stimulating agent use was not reported to affect disease progression (Amgen, 2011). Only limited conclusions can be drawn, however, as this study was neither designed to evaluate long-term survival or disease progression outcomes nor stratified to balance relevant prognostic factors.
The Gynaecologic Oncology Group (GOG)-191 study was conducted in cervical cancer patients receiving chemoradiotherapy who were randomised to receive or not receive recombinant Epo (40 000 IU weekly) during treatment (the overall radiation treatment time was ⩽8 weeks). This trial assessed whether maintaining haemoglobin levels of 13–14 g dl−1 would improve survival and progression outcomes (Thomas et al, 2008). Based on concerns of increased thromboembolic events in the ESA arm, the study closed after <25% of the planned accrual (460 patients were targeted to allow for 165 recurrences within 2 years). After a median follow-up of 37 months, results from 109 patients (52 in the control arm and 57 in the ESA arm) indicated that 25% of control patients and 33.3% of ESA-treated patients experienced disease recurrences; however, this result was not statistically significant (P=0.65) (Thomas et al, 2008). At ∼3 years, 73% of control patients and 61% of ESA-treated patients were still alive; 65% of control patients and 60% of ESA-treated patients were progression-free (Thomas et al, 2008). As this trial closed prematurely, the effect of ESAs on progression and mortality in this study remains undetermined.
The Preoperative Epirubicin Paclitaxel Aranesp (PREPARE) study evaluated the effect of preoperative dose-dense, dose-intensified chemotherapy with anthracyclines and taxanes in breast cancer patients (N=733). A second randomisation assigned patients to receive or not receive darbepoetin alfa 4.5 μg kg−1 every 2 weeks to maintain haemoglobin concentrations between 12.5–13 g dl−1. Secondary endpoints included the effect of darbepoetin alfa on disease-free survival and overall survival. After a median follow-up of ∼3 years, an unplanned-interim analysis of 733 patients indicated that survival and progression-free survival rates were lower in ESA-treated patients (this difference was not statistically significant) (Amgen, 2008). Final results from the PREPARE trial were recently published in two manuscripts (Untch et al, 2011a, 2011b). When comparing ESA-treated patients with control patients, the 3-year estimated HR (95% CI) was 1.31 (0.99–1.74; P=0.061) for disease-free survival and 1.33 (0.91–1.95; P=0.139) for overall survival (Untch et al, 2011b). Though these results suggest a trend of decreased disease-free survival with darbepoetin alfa use, the findings were not statistically significant. Darbepoetin alfa use did not affect pathological-complete response (Untch et al, 2011a).
In summary, of the eight oncology studies of concern described in the ESA-product labelling, the two conducted in head and neck cancer patients receiving radiotherapy only showed the strongest evidence for an association between ESA use and disease progression. A recent study level meta-analysis by Glaspy et al (2010) reported an odds ratio (OR) for disease progression for each of the eight studies of concern. These results also suggested that only the ENHANCE and DAHANCA-10 studies demonstrated a statistically significant impact of ESA use on disease progression (Table 1).
Additional chemotherapy studies
As the eight studies of concern were added to the ESA-product labelling, several large trials published between 2008 and 2010 have reported data regarding ESAs and disease progression in the chemotherapy setting. Four larger additional studies are described below.
The randomised, placebo-controlled AMG 20010145 study in small-cell lung cancer patients receiving chemotherapy (N=596 evaluated) compared overall survival (primary endpoint) and disease progression (additional efficacy endpoint) in patients receiving darbepoetin alfa or placebo (haemoglobin <13 g dl−1) (Pirker et al, 2008). This is one of the few controlled ESA trials in which all patients received the same chemotherapy regimen and in which tumour progression was assessed radiographically using blinded-centralised review. Published results of analyses stratified by randomisation factors indicated no significant difference between the two arms for progression-free survival (HR=1.02; 95% CI: 0.86–1.21; P=0.82) or overall survival (HR=0.93; 95% CI: 0.78–1.11; P=0.43) (Pirker et al, 2008).
Results from an Arbeitsgemeinschaft Gynäkologische Onkologie (AGO) phase 3 trial (Moebus et al, 2010) were recently published. This trial compared dose-dense chemotherapy vs conventionally scheduled chemotherapy in high-risk primary breast cancer patients (stage II–IIIA with ⩾4 positive axillary lymph nodes). Patients in the dose-dense arm (N=641 evaluated) were additionally randomised to receive or not receive epoetin alfa (haemoglobin at 12.5–13 g dl−1). In ad-hoc analyses, the manuscript reported that epoetin alfa did not affect overall survival or event-free survival (defined as locoregional or distant relapse, contralateral breast cancer, second primary-cancer occurrence, or death) but that detailed information will be communicated in a later publication (Moebus et al, 2010). (Of note, the most recent available data from the AGO trial were used in the meta-analysis of controlled ESA trials by Glaspy et al (2010) that examined the impact of ESAs on mortality/disease progression).
Results from the large GHSG HD15EPO trial were also recently published. Patients (N=1328 evaluated for safety) with advanced Hodgkin's lymphoma receiving chemotherapy were randomised to epoetin alfa or placebo (haemoglobin at 12–14 g dl−1 during chemotherapy and <12 g dl−1 after chemotherapy) (Engert et al, 2010). Results indicated that after a median-observation period of 3 years, epoetin alfa had no impact on freedom-from-treatment failure (HR=0.87; 95% CI: 0.63–1.20) or overall survival (HR=0.74; 95% CI: 0.45–1.22) (Engert et al, 2010).
A LNH03-6B Groupe d’ Etude des Lymphomes de l’ Adulte (GELA) study is currently being conducted in patients with large B-cell lymphoma receiving chemotherapy (R-CHOP) (Delarue et al, 2011). Patients were secondarily randomised to darbepoetin alfa (N=238; initially to maintain haemoglobin at 13–15 g dl−1 and later amended to 13–14 g dl−1) or to receive best-supportive care (ESA and transfusions administered according to usual practices; N=362). A second interim analysis was recently reported and indicated that 3-year progression-free survival was 66% in the darbepoetin alfa arm and 58% in the control arm (HR=0.77; 95% CI: 0.59–0.99). In an exploratory analysis comparing patients treated with or without ESAs (40% of controls received ESAs as supportive care), the HR for progression-free survival was 0.73 (95% CI: 0.57–0.94) (Delarue et al, 2011).
Recent randomised, controlled ESA studies also suggest no significant impact of ESAs on disease progression in chemotherapy patients (Wagner et al, 2004; Reed et al, 2005; Bohlius et al, 2009; Gupta et al, 2009; Ludwig et al, 2009; Nagel et al, 2011). Of note, a retrospective study in 323 multiple myeloma patients receiving chemotherapy reported that median progression-free survival was significantly shorter (P<0.001) in ESA-treated patients compared with non-ESA-treated patients (Katodritou et al, 2008). In contrast, a retrospective study (Hershman et al, 2009) of chemotherapy patient data from the SEER-Medicare database (from 1991 to 2002) indicated that overall survival was similar between patients receiving ESAs (N=12 522) or not receiving ESAs (N=34 820). In recently reported preliminary final results, the ARA Plus study (N=1234) prospectively evaluated event-free survival and overall survival in a randomised controlled study of adjuvant chemotherapy with or without darbepoetin in node-positive breast cancer patients (Nitz et al, 2011). After a median follow-up of 40 months, there were no significant differences in 3-year event-free survival (89.2% vs 87.6%, P=0.97) or overall survival (95.4% vs 95.1%, P=0.85) between patients receiving darbepoetin vs standard of care, respectively.
Meta-analyses of ESA trials
Several recent meta-analyses have examined ESA use and safety outcomes in cancer patients. The large meta-analyses by Bennett et al (2008) and Bohlius et al (2009) reported a negative ESA impact risk on mortality but not on how ESAs affect disease progression. A recent meta-analysis by Tonelli et al (2009) analysed 52 controlled ESA-oncology trials; this meta-analysis was unique in that it did not include the BEST trial (Leyland-Jones et al, 2005) and included studies examining preoperative-ESA therapy. This meta-analysis did summarise two trials (N=247) that reported numbers of complete and partial tumour responses. These numbers did not differ significantly between ESA-treated and control patients (risk ratio for complete response=0.88; 95% CI: 0.69–1.12; risk ratio for partial response=0.70; 95% CI: 0.44–1.11).
Table 2 lists six meta-analyses that examined disease progression data from more than two controlled-ESA studies. These six meta-analyses examine overlapping data as they include subsets of the same studies. The publications by Hedenus et al (2005), Boogaerts et al (2006), and Seidenfeld et al (2006) reported results from three smaller meta-analyses (<1200 patients each). These meta-analyses suggested no significant impact of ESAs on disease progression (Table 2) (Hedenus et al, 2005; Boogaerts et al, 2006; Seidenfeld et al, 2006). The larger meta-analysis by Ludwig et al (2009) described a patient-level analysis of six randomised, controlled darbepoetin alfa trials performed in chemotherapy patients (N=2122). Analyses stratified by study indicated that darbepoetin alfa had no effect on disease progression (HR=0.92; 95% CI: 0.82–1.03), progression-free survival (HR=0.93; 95% CI: 0.84–1.04), or mortality (HR=0.97; 95% CI: 0.85–1.1). Aapro et al (2009b) described a meta-analysis using individual patient-level data from 12 randomised, controlled epoetin beta studies (N=2297) conducted in the oncology settings of chemotherapy, radiotherapy only, and surgery. An un-stratified analysis indicated a reduced risk of disease progression in the epoetin beta-treated patients (HR=0.85; 95% CI: 0.72–1.01). A study-level meta-analysis by Glaspy et al (2010) examined disease progression in 26 controlled-ESA studies (N=9646). These studies were a subset of 60 studies identified in a literature search for controlled-ESA trials that reported mortality data in the chemotherapy, radiotherapy only, and anaemia-of-cancer settings (Table 1) (Glaspy et al, 2010). Results indicated that ESA use did not significantly impact disease progression (OR=1.01; 95% CI: 0.90–1.14) (Table 2).
Based on the balance of evidence to date, the six meta-analyses described above do not support an effect of ESAs on disease progression. However, safety data from some individual, controlled trials suggest that ESAs might affect disease progression and/or mortality in certain cancer patient populations (head and neck cancer patients receiving radiotherapy only may be at particular risk). The need for additional research to understand whether and how ESAs affect tumour cell growth has stimulated much preclinical work in this field.
ESAs and disease progression mechanisms: evidence from preclinical studies
To explain the conflicting clinical data, several mechanisms for disease progression have been postulated. The most widely studied is whether an Epo-specific receptor exists on tumour cells, endothelial cells, or other non-erythrocyte progenitor cells.
The EpoR and tumour cells
Like endogenous Epo, ESAs bind to and activate EpoR on erythrocytic progenitors (colony-forming units erythroid) in bone marrow (Broudy et al, 1991). This stimulates erythrocytic progenitor cells to proliferate and differentiate into RBCs. Without an ESA or endogenous Epo, erythrocytic precursors at the proerythroblast stage undergo apoptosis (Koury and Bondurant, 1988). Activation of EpoR stimulates JAK2 kinase, which binds to the cytosolic domains of the EpoR dimers (Figure 1) (Witthuhn et al, 1993). Activated JAK2 kinase stimulates multiple signalling pathways in erythrocytic precursor cells (Huang et al, 2001; Jelkmann et al, 2008). The JAK2 kinase is also an essential chaperone for translocating EpoR to the cell surface (Huang et al, 2001). It has been postulated that if tumour cells express EpoR, ESAs could activate these receptors to induce tumour cell proliferation (Hadland and Longmore, 2009). Thus, examining whether tumour cells express ESA-responsive EpoR has been of interest.
Schematic presentation of the signalling pathways activated by the EpoR on erythrocytic progenitor cells in response to Epo. When the surface of an erythrocytic progenitor cell is exposed to Epo, the pre-formed EpoR dimer undergoes a conformational change that stimulates autophosphorylation of JAK2 kinase, which is associated with the EpoR intracellular domains. In turn, JAK2 kinases phosphorylate tyrosine residues on the EpoR intracellular domains, which then serve as docking sites for various cytoplasmic signalling proteins such as the transcription factor STAT5 (signal transducer and activator of transcription 5). Stimulation of cytoplasmic signalling proteins such as STAT5, AKT, and ERK1/2 activates signalling cascades that can lead to cellular differentiation, anti-apoptotic effects, and cellular proliferation.
Several studies have suggested that tumour tissues and tumour cell lines express EpoR mRNA and also contain EpoR protein as demonstrated by western-blot analysis or immunohistochemistry (Sinclair et al, 2007; Jelkmann et al, 2008). However, technical issues have limited the validity of these findings and often qualitative, rather than quantitative, studies were performed. For example, studies examining EpoR-mRNA levels often used bulk tumour tissue, which can contain stromal cells and other cell types that infiltrate from blood. Moreover, several studies using western blot and/or immunohistochemistry may have yielded false-positive results because of use of commercially available polyclonal or monoclonal anti-EpoR antibodies later shown to lack specificity for EpoR (Elliott et al, 2006; Brown et al, 2007). In addition, many studies did not address whether EpoR was localised to the cell surface and/or whether it could be activated by an ESA. In a study suggesting that neuroblastoma SH-SY5Y cells contain EpoR molecules (<50 receptors per cell surface) that transmit an anti-apoptotic signal when exposed to an ESA (Um et al, 2007), cell surface EpoR could not be reliably detected using a radioactive Epo-binding assay.
Recent results have suggested that Epo can activate Jak2-mediated signalling and antagonise anti-HER2 (trastuzumab) therapy in breast cancer cells, and a non-significant decrease was observed in progression-free survival for patients treated with Epo and trastuzumab in a small, retrospective subgroup analysis (Liang et al, 2010). Another recent study also indicated partial reduction in the efficacy of cytotoxic therapy when combined with Epo in a mouse model of metastatic breast cancer (Hedley et al, 2011). However, interpretation of these studies is difficult because of the non-specific antibodies used to establish EpoR expression.
Although some studies have reported that hypoxia increases EpoR expression in non-haematopoietic cells (Farrell and Lee, 2004), research in breast carcinoma cell lines (LaMontagne et al, 2006) indicated that hypoxia did not affect EpoR expression and that Epo exposure did not induce cell proliferation or activate signalling molecules such as MAPK or Akt, which act downstream of EpoR. Studies in other tumour cell lines have also shown little/or no expression of EpoR protein and/or a lack of functional EpoR (Laugsch et al, 2008; Sinclair et al, 2008). Additional studies indicate that the EpoR gene is not amplified in tumour cells (Sinclair et al, 2008) and that Epo exposure does not induce tumour cell line proliferation or affect mortality in many animal tumour models (Osterborg et al, 2007; Sinclair et al, 2007).
Recently, a monoclonal antibody specific for EpoR was developed enabling detailed analysis of EpoR-protein expression and function (Elliott et al, 2010). Studies using this antibody have indicated that many tumour cell lines express low-to-undetectable levels of EpoR and that any EpoR present is not functional (exposure of the cell lines to Epo does not activate signalling molecules such as STAT5 that function downstream of EpoR) (Swift et al, 2010). In a study performed in primary human tumour samples from multiple epithelial tumour types, no cell surface or functional EpoR was detected (Rossi et al, 2009). These findings do not support the hypothesis that ESAs could increase the risk of disease progression by activating EpoR on tumour cells.
Indirect mechanisms
Erythropoiesis-stimulating agent exposure could theoretically increase the risk of disease progression via indirect mechanisms. Intriguingly, recent findings suggest that activated monocyte/macrophage cells express EpoR and that binding of Epo to these cells can prevent NF-κB activation, repress pro-inflammatory genes, and induce an immunosuppressive effect (Nairz et al, 2011). However, the possible immunomodulatory role of Epo influences on tumour growth is unknown. Tumour growth could also theoretically be influenced by changes in iron-dependent metabolism (especially in iron-deficient patients) (Shander et al, 2010) that result from an ESA-induced increase in RBC production. Research is needed to examine this possibility.
It has been proposed that ESAs could affect the cardiovascular system (van der Meer et al, 2004; Ribatti, 2010). There are reports showing in vitro angiogenic effects of Epo on human bone marrow-derived endothelial progenitor cells (EPCs) (Muller-Ehmsen et al, 2006; Zwezdaryk et al, 2007) and on endothelial cells derived from human adult myocardial tissue (Jaquet et al, 2002). Erythropoiesis-stimulating agent therapy has also been reported to increase circulating levels of EPCs (Bahlmann et al, 2003) and endogenous Epo levels were found to correlate with circulating EPCs in patients with ischaemic cardiomyopathy (Heeschen et al, 2003). However, ESA therapy did not affect the number of EPCs in donors for allogeneic peripheral blood stem cell transplantation (Kim et al, 2009) nor in patients with acute myocardial infarction (Taniguchi et al, 2010). In addition, long-term ESA treatment did not affect endothelial markers in patients on haemodialyses (Pawlak et al, 2007). At present, convincing evidence for an effect of ESAs on EPCs is missing in the clinical setting.
If blood vessel endothelial cells express EpoR, then ESA exposure could hypothetically stimulate neovascularisation or angiogenesis; blood vessel growth in a tumour could then enhance tumour proliferation. Some studies have suggested that endothelial cells contain EpoR mRNA and that Epo can stimulate endothelial cell proliferation (Anagnostou et al, 1990, 1994). However, a recent study demonstrated that human endothelial, renal, cardiac, and neuronal cells contain EpoR mRNA at levels 10–100-fold lower than those in cells highly responsive to Epo (Sinclair et al, 2010). In addition, low or no EpoR-protein expression was detected in these cell types using a recently developed specific anti-EpoR monoclonal antibody (Elliott et al, 2010). Erythropoiesis-stimulating agents were also observed to have no effect in a rat angiogenesis assay (Sinclair et al, 2010). These findings call into the question whether ESAs could indirectly stimulate disease progression via angiogenesis.
Venous thromboembolic events
Venous thromboembolic events (VTEs) represent a known risk associated with ESA use in cancer patients (Bennett et al, 2008; Glaspy et al, 2010). This risk is described in the ESA-product labelling (Amgen, 2011; Centocor Ortho Biotech Products, 2011) and can be managed clinically (of note, a recent exploratory analysis of a controlled-ESA trial suggested that administering anti-thrombotic therapy with ESAs may lower VTE rates) (Aapro et al, 2009a). Although a link between VTEs and disease progression has not been established, it has been hypothesised that VTEs may account for the increased mortality associated with ESAs in some studies (Hadland and Longmore, 2009). One proposed hypothesis is that ESAs could increase the incidence of VTEs by stimulating platelet production. Although some results suggest that Epo binds to megakaryocytes (but not platelets) (Fraser et al, 1988), whether functional EpoR is expressed on megakaryocytes remains unclear (Grossi et al, 1989; Yonemura et al, 1992) and high levels of endogenous Epo do not appear to elevate platelet counts in humans (Akan et al, 2000). Studies evaluating platelet counts after ESA administration have reported varying results (Grossi et al, 1989; Yonemura et al, 1992; Ait-Oudhia et al, 2010). Furthermore, a clear association between increased platelet counts and an increased incidence of VTEs has not been demonstrated (Buss et al, 1994; Basser et al, 1997).
Another hypothesis is that as JAK2 kinase is a key mediator of EpoR activity (Figure 1), an association may exist between VTEs and JAK2 kinase activation. Research has shown that 30–50% of patients with splanchnic-vein thromboses associated with Budd-Chiari syndrome (including portal-venous and hepatic-vein thrombosis) harbour a somatic mutation of the JAK2 gene (JAK2 V617F) that constitutively activates JAK2 kinase (Kiladjian et al, 2008). However, the JAK2V617F mutation is detected in multiple haematopoietic lineages (Ishii et al, 2006), and JAK2 kinase is essential for mediating signalling pathways for many cytokine receptors other than EpoR (Seidel et al, 2000). Therefore, no direct link between ESA-mediated JAK2 kinase activation and VTEs in cancer patients has been definitively established. Additional studies are required to understand the precise mechanism underlying the increased risk of VTEs associated with ESA use.
Summary and conclusion
This review summarised results from clinical and preclinical studies that evaluated whether ESAs affect disease progression. Although there are important limitations on the quality and assessment of disease progression in these studies, the current meta-analyses suggest no overall effect of ESAs on disease progression. Several individual studies have shown a potential trend associating ESA use with increased disease progression. This suggests that ESAs may affect disease progression in particular cancer patient populations (e.g., head and neck cancer patients receiving radiotherapy only) and that additional research is needed to define these populations and how ESAs mediate this effect. Although indirect effects on tumours induced by increased RBC production are theoretically possible, preclinical data to date suggest that tumour cells either do not express EpoR or express low levels of EpoR molecules that are non-functional and/or are not present at the cell surface. Overall, the balance of current evidence does not support an effect of ESAs on either activating EpoR on tumour cells or indirectly stimulating disease progression via angiogenesis. Future clinical trials, meta-analyses, and preclinical research should provide additional data to guide evidence-based use of ESAs in cancer patients.
Change history
28 March 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Aapro M, Barnadas A, Leonard RC, Marangolo M, Untch M, Ukarma L, Burger HU, Scherhag A, Osterwalder B ( 2009a ) What is the impact of antithrombotic therapy and risk factors on the frequency of thrombovascular events in patients with metastatic breast cancer receiving epoetin beta? Eur J Cancer 45 : 2984 – 2991
Aapro M, Leonard RC, Barnadas A, Marangolo M, Untch M, Malamos N, Mayordomo J, Reichert D, Pedrini JL, Ukarma L, Scherhag A, Burger HU ( 2008 ) Effect of once-weekly epoetin beta on survival in patients with metastatic breast cancer receiving anthracycline- and/or taxane-based chemotherapy: results of the Breast Cancer-Anemia and the Value of Erythropoietin (BRAVE) study . J Clin Oncol 26 : 592 – 598
Aapro M, Osterwalder B, Scherhag A, Burger HU ( 2009b ) Epoetin-beta treatment in patients with cancer chemotherapy-induced anaemia: the impact of initial haemoglobin and target haemoglobin levels on survival, tumour progression and thromboembolic events . Br J Cancer 101 : 1961 – 1971
Ait-Oudhia S, Scherrmann JM, Krzyzanski W ( 2010 ) Simultaneous pharmacokinetics/pharmacodynamics modeling of recombinant human erythropoietin upon multiple intravenous dosing in rats . J Pharmacol Exp Ther 334 : 897 – 910
Akan H, Guven N, Aydogdu I, Arat M, Beksac M, Dalva K ( 2000 ) Thrombopoietic cytokines in patients with iron deficiency anemia with or without thrombocytosis . Acta Haematol 103 : 152 – 156
Amgen ( 2008 ) Amgen Inc. in collaboration with Johnson & Johnson Pharmaceutical Research and Development, L.L.C.Background Information . For The Oncologic Drugs Advisory Comittee (ODAC) Meeting . 13 March 2008 available from http://www.fda.gov/ohrms/dockets/ac/08/briefing/2008-4345b2-00-FDA-index.htm
Amgen . Aranesp®(Darbepoetin alfa) Package Insert . Amgen Inc., Thousand Oaks, CA, ( 2011 )
Anagnostou A, Lee ES, Kessimian N, Levinson R, Steiner M ( 1990 ) Erythropoietin has a mitogenic and positive chemotactic effect on endothelial cells . Proc Natl Acad Sci USA 87 : 5978 – 5982
Anagnostou A, Liu Z, Steiner M, Chin K, Lee ES, Kessimian N, Noguchi CT ( 1994 ) Erythropoietin receptor mRNA expression in human endothelial cells . Proc Natl Acad Sci USA 91 : 3974 – 3978
Bahlmann FH, DeGroot K, Duckert T, Niemczyk E, Bahlmann E, Boehm SM, Haller H, Fliser D ( 2003 ) Endothelial progenitor cell proliferation and differentiation is regulated by erythropoietin . Kidney Int 64 : 1648 – 1652
Basser RL, Rasko JE, Clarke K, Cebon J, Green MD, Grigg AP, Zalcberg J, Cohen B, O’Byrne J, Menchaca DM, Fox RM, Begley CG ( 1997 ) Randomized, blinded, placebo-controlled phase I trial of pegylated recombinant human megakaryocyte growth and development factor with filgrastim after dose-intensive chemotherapy in patients with advanced cancer . Blood 89 : 3118 – 3128
Bennett CL, Silver SM, Djulbegovic B, Samaras AT, Blau CA, Gleason KJ, Barnato SE, Elverman KM, Courtney DM, McKoy JM, Edwards BJ, Tigue CC, Raisch DW, Yarnold PR, Dorr DA, Kuzel TM, Tallman MS, Trifilio SM, West DP, Lai SY, Henke M ( 2008 ) Venous thromboembolism and mortality associated with recombinant erythropoietin and darbepoetin administration for the treatment of cancer-associated anemia . JAMA 299 : 914 – 924
Blohmer J-U, Wurschmidt F, Petry U, Weise G, Sehouli J, Kimming R, Dressler P, Kentenich H, Kohls A, Lichtenegger W ( 2004 ) Results with sequential adjuvant chemo-radiotherapy with vs without epoetin alfa for patients with high-risk cervical cancer: Results of a prospective, randomized, open and controlled AGO- and NOGGO-intergroup study . Ann Oncol 15 (Suppl 3) : 128
Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, Zwahlen M, Clarke M, Weingart O, Kluge S, Piper M, Rades D, Steensma DP, Djulbegovic B, Fey MF, Ray-Coquard I, Machtay M, Moebus V, Thomas G, Untch M, Schumacher M, Egger M, Engert A ( 2009 ) Recombinant human erythropoiesis-stimulating agents and mortality in patients with cancer: a meta-analysis of randomised trials . Lancet 373 : 1532 – 1542
Boogaerts M, Oberhoff C, Ten Bokkel Huinink W, Nowrousian MR, Hayward CR, Burger HU ( 2006 ) Epoetin beta (NeoRecormon) therapy in patients with solid tumours receiving platinum and non-platinum chemotherapy: a meta-analysis . Anticancer Res 26 : 479 – 484
Broudy VC, Lin N, Brice M, Nakamoto B, Papayannopoulou T ( 1991 ) Erythropoietin receptor characteristics on primary human erythroid cells . Blood 77 : 2583 – 2590
Brown WM, Maxwell P, Graham AN, Yakkundi A, Dunlop EA, Shi Z, Johnston PG, Lappin TR ( 2007 ) Erythropoietin receptor expression in non-small cell lung carcinoma: a question of antibody specificity . Stem Cells 25 : 718 – 722
Buss DH, Cashell AW, O’Connor ML, Richards 2nd F, Case LD ( 1994 ) Occurrence, etiology, and clinical significance of extreme thrombocytosis: a study of 280 cases . Am J Med 96 : 247 – 253
Caro JJ, Salas M, Ward A, Goss G ( 2001 ) Anemia as an independent prognostic factor for survival in patients with cancer: a systemic, quantitative review . Cancer 91 : 2214 – 2221
Cella D, Kallich J, McDermott A, Xu X ( 2004 ) The longitudinal relationship of hemoglobin, fatigue and quality of life in anemic cancer patients: results from five randomized clinical trials . Ann Oncol 15 : 979 – 986
Centocor Ortho Biotech Products ( 2011 ) Procrit® (Epoetin alfa) Package Insert . Centocor Ortho Biotech Products, L.P.: Raritan, NJ
Chang J, Couture F, Young S, McWatters KL, Lau CY ( 2005 ) Weekly epoetin alfa maintains hemoglobin, improves quality of life, and reduces transfusion in breast cancer patients receiving chemotherapy . J Clin Oncol 23 : 2597 – 2605
Delarue R, Haioun C, Coiffier B, Fornecker L, Fournier M, Mounier N, Molina TJ, Bologna S, Fruchart C, Picard S, Tilly H, Bosly A ( 2011 ) Survival effect of darbepoetin alfa in patients with diffuse large B-cell lymphoma (DLBCL) treated with immunochemotherapy: The LNH03-6B study . J Clin Oncol 29 (Suppl 15) : abstract 9048
Egrie JC, Dwyer E, Browne JK, Hitz A, Lykos MA ( 2003 ) Darbepoetin alfa has a longer circulating half-life and greater in vivo potency than recombinant human erythropoietin . Exp Hematol 31 : 290 – 299
Egrie JC, Strickland TW, Lane J, Aoki K, Cohen AM, Smalling R, Trail G, Lin FK, Browne JK, Hines DK ( 1986 ) Characterization and biological effects of recombinant human erythropoietin . Immunobiology 172 : 213 – 224
Elliott S, Busse L, Bass MB, Lu H, Sarosi I, Sinclair AM, Spahr C, Um M, Van G, Begley CG ( 2006 ) Anti-Epo receptor antibodies do not predict Epo receptor expression . Blood 107 : 1892 – 1895
Elliott S, Busse L, McCaffery I, Rossi J, Sinclair A, Spahr C, Swift S, Begley CG ( 2010 ) Identification of a sensitive anti-erythropoietin receptor monoclonal antibody allows detection of low levels of EpoR in cells . J Immunol Methods 352 : 126 – 139
eMC ( 2011 ) Electronic Medicines Compendium (eMC) website Available from http://emc.medicines.org.uk
EMEA ( 2011 ) European public assessment reports for authorised medicinal products for human use . European Medicines Agency website Available from http://www.emea.europa.eu/htms/human/epar/a.htm
Engert A, Diehl V, Stein H, Mueller R-P, Eich H, Dietlein M, Paulus U, Pfistner B, Josting A, Borchmann P, Fuchs M, Haferkamp H, Nisters-Backes H, Koch B ( 2007 ) Role of erythropoetin (EPO) in patients with Hodgkin lymphoma . Paper presented at The 7th International Symposium on Hodgkin Lymphoma ; November 3-7, 2007; Cologne, Germany
Engert A, Josting A, Haverkamp H, Villalobos M, Lohri A, Sokler M, Zijlstra J, Sturm I, Topp MS, Rank A, Zenz T, Vogelhuber M, Nogova L, Borchmann P, Fuchs M, Flechtner HH, Diehl V ( 2010 ) Epoetin alfa in patients with advanced-stage Hodgkin's lymphoma: results of the randomized placebo-controlled GHSG HD15EPO trial . J Clin Oncol 28 : 2239 – 2245
Farrell F, Lee A ( 2004 ) The erythropoietin receptor and its expression in tumor cells and other tissues . Oncologist 9 : 18 – 30
Fraser JK, Lin FK, Berridge MV ( 1988 ) Expression of high affinity receptors for erythropoietin on human bone marrow cells and on the human erythroleukemic cell line, HEL . Exp Hematol 16 : 836 – 842
Glaspy J, Crawford J, Vansteenkiste J, Henry D, Rao S, Bowers P, Berlin JA, Tomita D, Bridges K, Ludwig H ( 2010 ) Erythropoiesis-stimulating agents in oncology: a study-level meta-analysis of survival and other safety outcomes . Br J Cancer 102 : 301 – 315
Groopman JE, Itri LM ( 1999 ) Chemotherapy-induced anemia in adults: incidence and treatment . J Natl Cancer Inst 91 : 1616 – 1634
Grossi A, Vannucchi AM, Rafanelli D, Rossi Ferrini P ( 1989 ) Recombinant human erythropoietin has little influence on megakaryocytopoiesis in mice . Br J Haematol 71 : 463 – 468
Grote T, Yeilding AL, Castillo R, Butler D, Fishkin E, Henry DH, DeLeo M, Fink K, Sullivan DJ ( 2005 ) Efficacy and safety analysis of epoetin alfa in patients with small-cell lung cancer: a randomized, double-blind, placebo-controlled trial . J Clin Oncol 23 : 9377 – 9386
Gupta S, Singh PK, Bisth SS, Bhatt ML, Pant M, Gupta R, Singh S, Negi MP ( 2009 ) Role of recombinant human erythropoietin in patients of advanced cervical cancer treated ‘by chemoradiotherapy‘ . Cancer Biol Ther 8 : 13 – 17
Hadland BK, Longmore GD ( 2009 ) Erythroid-stimulating agents in cancer therapy: potential dangers and biologic mechanisms . J Clin Oncol 27 : 4217 – 4226
Hedenus M, Adriansson M, San Miguel J, Kramer MH, Schipperus MR, Juvonen E, Taylor K, Belch A, Altes A, Martinelli G, Watson D, Matcham J, Rossi G, Littlewood TJ, Darbepoetin alfa 20000161 Study Group ( 2003 ) Efficacy and safety of darbepoetin alfa in anaemic patients with lymphoproliferative malignancies: a randomized, double-blind, placebo-controlled study . Br J Haematol 122 : 394 – 403
Hedenus M, Vansteenkiste J, Kotasek D, Austin M, Amado RG ( 2005 ) Darbepoetin alfa for the treatment of chemotherapy-induced anemia: disease progression and survival analysis from four randomized, double-blind, placebo-controlled trials . J Clin Oncol 23 : 6941 – 6948
Hedley BD, Chu JE, Ormond DG, Beausoleil MS, Boasie A, Allan AL, Xenocostas A ( 2011 ) Recombinant human erythropoietin in combination with chemotherapy increases breast cancer metastasis in preclinical mouse models . Clin Cancer Res 17 : 6151 – 6162
Heeschen C, Aicher A, Lehmann R, Fichtlscherer S, Vasa M, Urbich C, Mildner-Rihm C, Martin H, Zeiher AM, Dimmeler S ( 2003 ) Erythropoietin is a potent physiologic stimulus for endothelial progenitor cell mobilization . Blood 102 : 1340 – 1346
Henke M, Laszig R, Rube C, Schafer U, Haase KD, Schilcher B, Mose S, Beer KT, Burger U, Dougherty C, Frommhold H ( 2003 ) Erythropoietin to treat head and neck cancer patients with anaemia undergoing radiotherapy: randomised, double-blind, placebo-controlled trial . Lancet 362 : 1255 – 1260
Henke M, Mattern D, Pepe M, Bezay C, Weissenberger C, Werner M, Pajonk F ( 2006 ) Do erythropoietin receptors on cancer cells explain unexpected clinical findings? J Clin Oncol 24 : 4708 – 4713
Hershman DL, Buono DL, Malin J, McBride R, Tsai WY, Neugut AI ( 2009 ) Patterns of use and risks associated with erythropoiesis-stimulating agents among Medicare patients with cancer . J Natl Cancer Inst 101 : 1633 – 1641
Hoskin PJ, Robinson M, Slevin N, Morgan D, Harrington K, Gaffney C ( 2009 ) Effect of epoetin alfa on survival and cancer treatment-related anemia and fatigue in patients receiving radical radiotherapy with curative intent for head and neck cancer . J Clin Oncol 27 : 5751 – 5756
Huang LJ, Constantinescu SN, Lodish HF ( 2001 ) The N-terminal domain of Janus kinase 2 is required for Golgi processing and cell surface expression of erythropoietin receptor . Mol Cell 8 : 1327 – 1338
Ishii T, Bruno E, Hoffman R, Xu M ( 2006 ) Involvement of various hematopoietic-cell lineages by the JAK2V617F mutation in polycythemia vera . Blood 108 : 3128 – 3134
Jaquet K, Krause K, Tawakol-Khodai M, Geidel S, Kuck KH ( 2002 ) Erythropoietin and VEGF exhibit equal angiogenic potential . Microvasc Res 64 : 326 – 333
Jelkmann W ( 2010 ) Biosimilar epoetins and other ‘follow-on‘ biologics: update on the European experiences . Am J Hematol 85 : 771 – 780
Jelkmann W, Bohlius J, Hallek M, Sytkowski AJ ( 2008 ) The erythropoietin receptor in normal and cancer tissues . Crit Rev Oncol Hematol 67 : 39 – 61
Johnson & Johnson Pharmaceutical Research and Development LLC ( 2004 ) Safety of erythropoietin receptor agonists (ERAs) in patients with cancer . Background Information for Oncologic Drugs Advisory Committee Meeting 4 May 2004. Available from http://www.fda.gov/ohrms/dockets/ac/04/briefing/4037b2.htm
Katodritou E, Verrou E, Hadjiaggelidou C, Gastari V, Laschos K, Kontovinis L, Kapetanos D, Constantinou N, Terpos E, Zervas K ( 2008 ) Erythropoiesis-stimulating agents are associated with reduced survival in patients with multiple myeloma . Am J Hematol 83 : 697 – 701
Kiladjian JJ, Cervantes F, Leebeek FW, Marzac C, Cassinat B, Chevret S, Cazals-Hatem D, Plessier A, Garcia-Pagan JC, Darwish Murad S, Raffa S, Janssen HL, Gardin C, Cereja S, Tonetti C, Giraudier S, Condat B, Casadevall N, Fenaux P, Valla DC ( 2008 ) The impact of JAK2 and MPL mutations on diagnosis and prognosis of splanchnic vein thrombosis: a report on 241 cases . Blood 111 : 4922 – 4929
Kim SN, Moon JH, Kim JG, Chae YS, Cho YY, Lee SJ, Kim YJ, Lee YJ, Suh JS, Lee KS, Sohn SK ( 2009 ) Mobilization effects of G-CSF, GM-CSF, and darbepoetin-alpha for allogeneic peripheral blood stem cell transplantation . J Clin Apher 24 : 173 – 179
Klein HG, Spahn DR, Carson JL ( 2007 ) Red blood cell transfusion in clinical practice . Lancet 370 : 415 – 426
Koury MJ, Bondurant MC ( 1988 ) Maintenance by erythropoietin of viability and maturation of murine erythroid precursor cells . J Cell Physiol 137 : 65 – 74
LaMontagne KR, Butler J, Marshall DJ, Tullai J, Gechtman Z, Hall C, Meshaw A, Farrell FX ( 2006 ) Recombinant epoetins do not stimulate tumor growth in erythropoietin receptor-positive breast carcinoma models . Mol Cancer Ther 5 : 347 – 355
Laugsch M, Metzen E, Svensson T, Depping R, Jelkmann W ( 2008 ) Lack of functional erythropoietin receptors of cancer cell lines . Int J Cancer 122 : 1005 – 1011
Leyland-Jones B ( 2003 ) BEST Investigators and Study Group: breast cancer trial with erythropoietin terminated unexpectedly . Lancet Oncol 4 : 459 – 460
Leyland-Jones B, Semiglazov V, Pawlicki M, Pienkowski T, Tjulandin S, Manikhas G, Makhson A, Roth A, Dodwell D, Baselga J, Biakhov M, Valuckas K, Voznyi E, Liu X, Vercammen E ( 2005 ) Maintaining normal hemoglobin levels with epoetin alfa in mainly nonanemic patients with metastatic breast cancer receiving first-line chemotherapy: a survival study . J Clin Oncol 23 : 5960 – 5972
Liang K, Esteva FJ, Albarracin C, Stemke-Hale K, Lu Y, Bianchini G, Yang CY, Li Y, Li X, Chen CT, Mills GB, Hortobagyi GN, Mendelsohn J, Hung MC, Fan Z ( 2010 ) Recombinant human erythropoietin antagonizes trastuzumab treatment of breast cancer cells via Jak2-mediated Src activation and PTEN inactivation . Cancer Cell 18 : 423 – 435
Littlewood TJ, Bajetta E, Nortier JW, Vercammen E, Rapoport B ( 2001 ) Effects of epoetin alfa on hematologic parameters and quality of life in cancer patients receiving nonplatinum chemotherapy: results of a randomized, double-blind, placebo-controlled trial . J Clin Oncol 19 : 2865 – 2874
Ludwig H, Crawford J, Osterborg A, Vansteenkiste J, Henry DH, Fleishman A, Bridges K, Glaspy JA ( 2009 ) Pooled analysis of individual patient-level data from all randomized, double-blind, placebo-controlled trials of darbepoetin alfa in the treatment of patients with chemotherapy-induced anemia . J Clin Oncol 27 : 2838 – 2847
Ludwig H, Van Belle S, Barrett-Lee P, Birgegard G, Bokemeyer C, Gascon P, Kosmidis P, Krzakowski M, Nortier J, Olmi P, Schneider M, Schrijvers D ( 2004 ) The European Cancer Anaemia Survey (ECAS): a large, multinational, prospective survey defining the prevalence, incidence, and treatment of anaemia in cancer patients . Eur J Cancer 40 : 2293 – 2306
Machtay M, Pajak TF, Suntharalingam M, Shenouda G, Hershock D, Stripp DC, Cmelak AJ, Schulsinger A, Fu KK ( 2007 ) Radiotherapy with or without erythropoietin for anemic patients with head and neck cancer: a randomized trial of the Radiation Therapy Oncology Group (RTOG 99-03) . Int J Radiat Oncol Biol Phys 69 : 1008 – 1017
Milroy R, Scagliotti G, van den Berg PM, Galanis NE, Gomez RG, Greil R, Krzakowski M ( 2003 ) Early intervention with epoetin alfa maintains hemoglobin (HB) in advanced non-small-cell lung cancer (NSCLC) patients . Lung Cancer 41 (Suppl 2) : S74
Mittelman M, Neumann D, Peled A, Kanter P, Haran-Ghera N ( 2001 ) Erythropoietin induces tumor regression and antitumor immune responses in murine myeloma models . Proc Natl Acad Sci USA 98 : 5181 – 5186
Moebus V, Jackisch C, Lueck HJ, du Bois A, Thomssen C, Kurbacher C, Kuhn W, Nitz U, Schneeweiss A, Huober J, Harbeck N, von Minckwitz G, Runnebaum IB, Hinke A, Kreienberg R, Konecny GE, Untch M ( 2010 ) Intense dose-dense sequential chemotherapy with epirubicin, paclitaxel, and cyclophosphamide compared with conventionally scheduled chemotherapy in high-risk primary breast cancer: mature results of an AGO phase III study . J Clin Oncol 28 : 2874 – 2880
Moebus V, Lueck H, Thomssen C, Harbeck N, Nitz U, Kreienberg R, Jackisch C, Schneeweiss A, Huober J, du Bois A, Untch M ( 2007 ) The impact of epoetin-alpha on anemia, red blood cell (RBC) transfusions, and survival in breast cancer patients (pts) treated with dose-dense sequential chemotherapy: mature results of an AGO phase III study (ETC trial) . J Clin Oncol 25 (Suppl 18) : abstract 569
Muller-Ehmsen J, Schmidt A, Krausgrill B, Schwinger RH, Bloch W ( 2006 ) Role of erythropoietin for angiogenesis and vasculogenesis: from embryonic development through adulthood . Am J Physiol Heart Circ Physiol 290 : 331 – 340
Nagel S, Kellner O, Engel-Riedel W, Guetz S, Schumann C, Gieseler F, Schuette W ( 2011 ) Addition of darbepoetin alfa to dose-dense chemotherapy: results from a randomized phase II trial in small-cell lung cancer patients receiving carboplatin plus etoposide . Clin Lung Cancer 12 : 62 – 69
Nairz M, Schroll A, Moschen AR, Sonnweber T, Theurl M, Theurl I, Taub N, Jamnig C, Neurauter D, Huber LA, Tilg H, Moser PL, Weiss G ( 2011 ) Erythropoietin contrastingly affects bacterial infection and experimental colitis by inhibiting nuclear factor-κB-inducible immune pathways . Immunity 34 : 61 – 74
Nitz U, Gluz O, Oberhoff C, Reimer T, Schumacher C, Hackmann J, Warm M, Uleer C, Runde V, Kuemmel S, Zuna I, Harbeck N ( 2011 ) Adjuvant chemotherapy with or without darbepoetin alpha in node-positive breast cancer: survival and quality of life analysis from the prospective randomized WSG ARA Plus trial . Paper presented at The 34th San Antonio Breast Cancer Symposium; December 6-10, 2011; San Antonio, United States
Osterborg A, Aapro M, Cornes P, Haselbeck A, Hayward CR, Jelkmann W ( 2007 ) Preclinical studies of erythropoietin receptor expression in tumour cells: impact on clinical use of erythropoietic proteins to correct cancer-related anaemia . Eur J Cancer 43 : 510 – 519
Osterborg A, Boogaerts MA, Cimino R, Essers U, Holowiecki J, Juliusson G, Jager G, Najman A, Peest D ( 1996 ) Recombinant human erythropoietin in transfusion-dependent anemic patients with multiple myeloma and non-Hodgkin's lymphoma--a randomized multicenter study. The European Study Group of Erythropoietin (Epoetin Beta) Treatment in Multiple Myeloma and Non-Hodgkin's Lymphoma . Blood 87 : 2675 – 2682
Osterborg A, Brandberg Y, Hedenus M ( 2005 ) Impact of epoetin-beta on survival of patients with lymphoproliferative malignancies: long-term follow up of a large randomized study . Br J Haematol 129 : 206 – 209
Overgaard J, Hoff C, Hansen HS, Specht L, Overgaard M, Grau C, Andersen E, Johansen J, Andersen LJ, Evensen JF ( 2010 ) Randomized study of Aranesp as modifier of radiotherapy in patients with primary squamous cell carcinoma of the head and neck (HNSCC) - Final outcome of the DAHANCA 10 trial . Radiother Oncol 96 (Suppl 15) : abstract 197
Overgaard J, Hoff C, Sand Hansen H, Specht L, Overgaard M, Grau C, Andersen E, Johansen J, Andersen L, Evensen J ( 2007 ) Randomized study of the importance of Novel Erythropoiesis Stimulating Protein (Aranesp®) for the effect of radiotherapy in patients with primary squamous cell carcinoma of the head and neck (HNSCC)- the Danish Head and Neck Cancer Group DAHANCA 10 randomized trial . Eur J Cancer 5 (Suppl 7) : 7
Pawlak K, Pawlak D, Mysliwiec M ( 2007 ) Long-term erythropoietin therapy does not affect endothelial markers, coagulation activation and oxidative stress in haemodialyzed patients . Thromb Res 120 : 797 – 803
Pirker R, Ramlau RA, Schuette W, Zatloukal P, Ferreira I, Lillie T, Vansteenkiste JF ( 2008 ) Safety and efficacy of darbepoetin alfa in previously untreated extensive-stage small-cell lung cancer treated with platinum plus etoposide . J Clin Oncol 26 : 2342 – 2349
Pronzato P, Cortesi E, van der Rijt C, Moreno-Nogueira A, Raimundo D, Ostler P, Bols A, Rosso R ( 2002 ) Early intervention with epoetin alfa in breast cancer (BC) patients (pts) undergoing chemotherapy (CT): Results of a randomized, multicenter, phase IIIb study (EPO-INT-47 Study Group) . Ann Oncol 13 (Suppl 5) : 168
Reed SD, Radeva JI, Daniel DB, Fastenau JM, Williams D, Schulman KA ( 2005 ) Early hemoglobin response and alternative metrics of efficacy with erythropoietic agents for chemotherapy-related anemia . Curr Med Res Opin 21 : 1527 – 1533
Ribatti D ( 2010 ) Erythropoietin and tumor angiogenesis . Stem Cells Dev 19 : 1 – 4
Rossi J, McCaffery I, Paweletz K, Tudor Y, Elliott S, Fitzpatrick VD, Patterson SD ( 2009 ) Analysis of cell surface erythropoietin receptor (EpoR) expression and function in human epithelial tumor tissues . J Clin Oncol 27 (Suppl 15) : abstract 11104
Seidel HM, Lamb P, Rosen J ( 2000 ) Pharmaceutical intervention in the JAK/STAT signaling pathway . Oncogene 19 : 2645 – 2656
Seidenfeld J, Piper M, Bohlius J, Weingart O, Trelle S, Engert A, Skoetz N, Schwarzer G, Wilson J, Brunskill S, Hyde C, Bonnell C, Ziegler KM, Aronson N ( 2006 ) Comparative Effectiveness of Epoetin and Darbepoetin for Managing Anemia in Patients Undergoing Cancer Treatment Comparative Effectiveness Review No. 3. (Prepared by Blue Cross and Blue Shield Association Technology Evaluation Center Evidence-based Practice Center under Contract No. 290-02-0026). Agency for Healthcare Research and Quality: Rockville, MD . May 2006 Available from http://effectivehealthcare.ahrq.gov/repFiles/EPO%20Final.pdf
Shander A, Spence RK, Auerbach M ( 2010 ) Can intravenous iron therapy meet the unmet needs created by the new restrictions on erythropoietic stimulating agents? Transfusion 50 : 719 – 732
Sinclair AM, Coxon A, McCaffery I, Kaufman S, Paweletz K, Liu L, Busse L, Swift S, Elliott S, Begley CG ( 2010 ) Functional erythropoietin receptor is undetectable in endothelial, cardiac, neuronal, and renal cells . Blood 115 : 4264 – 4272
Sinclair AM, Rogers N, Busse L, Archibeque I, Brown W, Kassner PD, Watson JEV, Arnold GE, Nguyen KCQ, Powers S, Elliott S ( 2008 ) Erythropoietin receptor transcription is neither elevated nor predictive of surface expression in human tumour cells . Br J Cancer 98 : 1059 – 1067
Sinclair AM, Todd MD, Forsythe K, Knox SJ, Elliott S, Begley CG ( 2007 ) Expression and function of erythropoietin receptors in tumors: implications for the use of erythropoiesis-stimulating agents in cancer patients . Cancer 110 : 477 – 488
Smith Jr RE, Aapro MS, Ludwig H, Pinter T, Smakal M, Ciuleanu TE, Chen L, Lillie T, Glaspy JA ( 2008 ) Darbepoetin alfa for the treatment of anemia in patients with active cancer not receiving chemotherapy or radiotherapy: results of a phase III, multicenter, randomized, double-blind, placebo-controlled study . J Clin Oncol 26 : 1040 – 1050
Strauss HG, Haensgen G, Dunst J, Hayward CR, Burger HU, Scherhag A, Koelbl H ( 2008 ) Effects of anemia correction with epoetin beta in patients receiving radiochemotherapy for advanced cervical cancer . Int J Gynecol Cancer 18 : 515 – 524
Swift S, Ellison AR, Kassner P, McCaffery I, Rossi J, Sinclair AM, Begley CG, Elliott S ( 2010 ) Absence of functional EpoR expression in human tumor cell lines . Blood 115 : 4254 – 4263
Taniguchi N, Nakamura T, Sawada T, Matsubara K, Furukawa K, Hadase M, Nakahara Y, Matsubara H ( 2010 ) Erythropoietin prevention trial of coronary restenosis and cardiac remodeling after ST-elevated acute myocardial infarction (EPOC-AMI): a pilot, randomized, placebo-controlled study . Circ J 74 : 2365 – 2371
Thews O, Koenig R, Kelleher DK, Kutzner J, Vaupel P ( 1998 ) Enhanced radiosensitivity in experimental tumours following erythropoietin treatment of chemotherapy-induced anaemia . Br J Cancer 78 : 752 – 756
Thomas G, Ali S, Hoebers FJ, Darcy KM, Rodgers WH, Patel M, Abulafia O, Lucci 3rd JA, Begg AC ( 2008 ) Phase III trial to evaluate the efficacy of maintaining hemoglobin levels above 12.0 g/dl with erythropoietin vs above 10.0 g/dl without erythropoietin in anemic patients receiving concurrent radiation and cisplatin for cervical cancer . Gynecol Oncol 108 : 317 – 325
Tonelli M, Hemmelgarn B, Reiman T, Manns B, Reaume MN, Lloyd A, Wiebe N, Klarenbach S ( 2009 ) Benefits and harms of erythropoiesis-stimulating agents for anemia related to cancer: a meta-analysis . CMAJ 180 : 62 – 71
Um M, Gross AW, Lodish HF ( 2007 ) A ‘classical’ homodimeric erythropoietin receptor is essential for the antiapoptotic effects of erythropoietin on differentiated neuroblastoma SH-SY5Y and pheochromocytoma PC-12 cells . Cell Signal 19 : 634 – 645
Untch M, Fasching PA, Bauerfeind I, Conrad U, Camara O, Fett W, Kuzeder W, Lück H, Loibl S, Von Minckwitz G ( 2008 ) PREPARE trial. A randomized phase III trial comparing preoperative, dose-dense, dose-intensified chemotherapy with epirubicin, paclitaxel, and CMF with a standard dosed epirubicin/cyclophosphamide followed by paclitaxel ± darbepoetin alfa in primary breast cancer: A preplanned interim analysis of efficacy at surgery . J Clin Oncol 26 (Suppl 15) : abstract 517
Untch M, Fasching PA, Konecny GE, von Koch F, Conrad U, Fett W, Kurzeder C, Luck HJ, Stickeler E, Urbaczyk H, Liedtke B, Salat C, Harbeck N, Muller V, Schmidt M, Hasmuller S, Lenhard M, Schuster T, Nekljudova V, Loibl S, von Minckwitz G ( 2011a ) PREPARE trial: a randomized phase III trial comparing preoperative, dose-dense, dose-intensified chemotherapy with epirubicin, paclitaxel and CMF versus a standard-dosed epirubicin/cyclophosphamide followed by paclitaxel {+/-} darbepoetin alfa in primary breast cancer--results at the time of surgery . Ann Oncol 22 : 1988 – 1998
Untch M, von Minckwitz G, Konecny GE, Conrad U, Fett W, Kurzeder C, Luck HJ, Stickeler E, Urbaczyk H, Liedtke B, Beckmann MW, Salat C, Harbeck N, Muller V, Schmidt M, Hasmuller S, Lenhard M, Nekljudova V, Loibl S, Fasching PA ( 2011b ) PREPARE trial: a randomized phase III trial comparing preoperative, dose-dense, dose-intensified chemotherapy with epirubicin, paclitaxel, and CMF versus a standard-dosed epirubicin-cyclophosphamide followed by paclitaxel with or without darbepoetin alfa in primary breast cancer--outcome on prognosis . Ann Oncol 22 : 1999 – 2006
Vadhan-Raj S, Skibber JM, Crane C, Bueso-Ramos CE, Rodriguez-Bigas MA, Feig BW, Lin EH, Ajani JA, Collard M, Johnson MM, Hamilton SR, JanJan N ( 2004 ) Randomized, double-blind, placebo-controlled trial of epoetin alfa (Procrit) in patients with rectal and gastric cancer undergoing chemo-radiotherapy (CT/RT) followed by surgery: Early termination of the trial due to increased incidence of thrombo-embolic events (TEE) . Blood 104 : abstract 2915
van der Meer P, Voors AA, Lipsic E, van Gilst WH, van Veldhuisen DJ ( 2004 ) Erythropoietin in cardiovascular diseases . Eur Heart J 25 (4) : 285 – 291
Vansteenkiste J, Pirker R, Massuti B, Barata F, Font A, Fiegl M, Siena S, Gateley J, Tomita D, Colowick AB, Musil J, Aranesp 980297 Study Group ( 2002 ) Double-blind, placebo-controlled, randomized phase III trial of darbepoetin alfa in lung cancer patients receiving chemotherapy . J Natl Cancer Inst 94 : 1211 – 1220
Wagner LM, Billups CA, Furman WL, Rao BN, Santana VM ( 2004 ) Combined use of erythropoietin and granulocyte colony-stimulating factor does not decrease blood transfusion requirements during induction therapy for high-risk neuroblastoma: a randomized controlled trial . J Clin Oncol 22 : 1886 – 1893
Wilkinson PM, Antonopoulos M, Lahousen M, Lind M, Kosmidis P ( 2006 ) Epoetin alfa in platinum-treated ovarian cancer patients: results of a multinational, multicentre, randomised trial . Br J Cancer 94 : 947 – 954
Witthuhn BA, Quelle FW, Silvennoinen O, Yi T, Tang B, Miura O, Ihle JN ( 1993 ) JAK2 associates with the erythropoietin receptor and is tyrosine phosphorylated and activated following stimulation with erythropoietin . Cell 74 : 227 – 236
Witzig TE, Silberstein PT, Loprinzi CL, Sloan JA, Novotny PJ, Mailliard JA, Rowland KM, Alberts SR, Krook JE, Levitt R, Morton RF ( 2005 ) Phase III, randomized, double-blind study of epoetin alfa compared with placebo in anemic patients receiving chemotherapy . J Clin Oncol 23 : 2606 – 2617
Wright JR, Ung YC, Julian JA, Pritchard KI, Whelan TJ, Smith C, Szechtman B, Roa W, Mulroy L, Rudinskas L, Gagnon B, Okawara GS, Levine MN ( 2007 ) Randomized, double-blind, placebo-controlled trial of erythropoietin in non-small-cell lung cancer with disease-related anemia . J Clin Oncol 25 : 1027 – 1032
Yonemura Y, Kawakita M, Fujimoto K, Sakaguchi M, Kusuyama T, Hirose J, Kato K, Takatsuki K ( 1992 ) Effects of short-term administration of recombinant human erythropoietin on rat megakaryopoiesis . Int J Cell Cloning 10 : 18 – 27
Zwezdaryk KJ, Coffelt SB, Figueroa YG, Liu J, Phinney DG, LaMarca HL, Florez L, Morris CB, Hoyle GW, Scandurro AB ( 2007 ) Erythropoietin, a hypoxia-regulated factor, elicits a pro-angiogenic program in human mesenchymal stem cells . Exp Hematol 35 : 640 – 652
Acknowledgements
We thank Linda Rice and Shawn Lee at Amgen Inc. who provided writing assistance. Amgen Inc. reviewed this article for data accuracy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
M Aapro has received honoraria from and has had a consultant or advisory relationship with Amgen, Roche, and Sandoz. In addition, M Aapro has received research funding from Sandoz. W Jelkmann has received honoraria from and has had a consultant or advisory relationship with Amgen and Sandoz. In addition, W Jelkmann holds stock in Amgen and Roche, which are makers of Aranesp and NeoRecormon, respectively. SN Constantinescu has received honoraria from and has had a consultant or advisory relationship with Amgen. B Leyland-Jones declares no conflicts of interest.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Aapro, M., Jelkmann, W., Constantinescu, S. et al. Effects of erythropoietin receptors and erythropoiesis-stimulating agents on disease progression in cancer. Br J Cancer 106, 1249–1258 (2012). https://doi.org/10.1038/bjc.2012.42
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.42
Keywords
This article is cited by
-
The impact of erythropoiesis-stimulating agents administration concomitantly with adjuvant anti-HER2 treatments on the outcomes of patients with early breast cancer: a sub-analysis of the ALTTO study
Breast Cancer Research and Treatment (2024)
-
Synergistic immunotherapy targeting cancer-associated anemia: prospects of a combination strategy
Cell Communication and Signaling (2023)
-
Role of the initial degree of anaemia and treatment model in the prognosis of gastric cancer patients treated by chemotherapy: a retrospective analysis
BMC Cancer (2020)
-
Prevalence, etiology and risk factors of anemia in patients with newly diagnosed cancer
Supportive Care in Cancer (2020)
-
Erythropoietin inhibits chemotherapy-induced cell death and promotes a senescence-like state in leukemia cells
Cell Death & Disease (2019)