Abstract
In the nervous system, a decrease in extracellular pH is a common feature of various physiological and pathological processes, including synaptic transmission, cerebral ischemia, epilepsy, brain trauma, and tissue inflammation. Acid-sensing ion channels (ASICs) are proton-gated cation channels that are distributed throughout the central and peripheral nervous systems. Following the recent identification of ASICs as critical acid-sensing extracellular proton receptors, growing evidence has suggested that the activation of ASICs plays important roles in physiological processes such as nociception, mechanosensation, synaptic plasticity, learning and memory. However, the over-activation of ASICs is also linked to adverse outcomes for certain pathological processes, such as brain ischemia and multiple sclerosis. Based on the well-demonstrated role of ASIC1a activation in acidosis-mediated brain injury, small molecule inhibitors of ASIC1a may represent novel therapeutic agents for the treatment of neurological disorders, such as stroke.
Similar content being viewed by others
Introduction
The maintenance of extracellular and intracellular pH levels within a physiological range is critical for normal cellular activity. Under physiological conditions, Na+/H+ and Cl−/HCO3− systems generally maintain the extracellular and intracellular pH at approximately 7.3 and 7.0, respectively1,2. However, a local decrease in the extracellular pH may occur in certain micro-domains, such as the synaptic cleft. The synaptic vesicles are acidic, and thus their release during synaptic transmission can reduce the local pH of the synaptic cleft3. An extracellular pH reduction is also observed in hippocampal slices following electrical stimulation4. Thus, local pH fluctuations may occur under normal conditions5, although the extent and the physiological significance of pH fluctuations remain poorly understood.
Extracellular acidosis is more commonly observed in pathological conditions, such as brain ischemia/stroke6, seizure7,8, and brain trauma9. Moreover, the extent of the extracellular acidosis is closely related to the outcomes of these disorders. For instance, slight acidosis has been reported to reduce neuronal injury, partially due to the inhibition of N-methyl-D-aspartate (NMDA) receptor channels10. By contrast, severe acidosis during brain ischemia, which can reduce the extracellular pH levels to as low as 6.0, can cause deleterious brain damage11,12. Although the underlying mechanism by which acidosis leads to adverse outcomes for certain neurological disorders has remained elusive, the discovery of acid-sensing ion channels (ASICs) has provided new potential explanations for this phenomenon.
ASICs are critical acid sensors in the nervous system. ASIC1a, for instance, can sense slight extracellular acidosis at pH levels of approximately 7.013. Increasing evidence has demonstrated that ASICs play crucial physiological roles in processes such as nociception, learning and memory, and synaptic plasticity14,15. More importantly, ASICs are implicated in neurological disorders such as stroke16,17, inflammatory pain18,19,20, and epilepsy21,22. In this review, we will discuss the pharmacological properties and therapeutic potential of small molecule inhibitors of ASICs for stroke intervention.
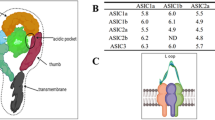
The molecular characterization and electrophysiological properties of ASICs
ASICs belong to the degenerin/epithelial Na+ channel (DEG/ENaC) superfamily, which also includes the FMRFamide-gated Na+ channel (FaNaC)13,23. ASICs possess short intracellular amino and carboxyl termini of 35–90 amino acids each and two hydrophobic transmembrane regions (approximately 20 amino acids each in size) that flank a large, cysteine-rich extracellular domain composed of approximately 370 amino acids24. In total, six ASIC isoforms have been described to date in mammals: ASIC1a, ASIC1b, ASIC2a, ASIC2b, ASIC3 and ASIC4; these isoforms are encoded by four genes25,26. The recent crystal structure of chicken ASIC1 has revealed the trimeric assembly of this protein27. The high sequence identity (90%) between chicken and human ASIC127 not only implies that ASIC1 fulfills important and conserved functions in the chordate nervous system but also suggests that the three-dimensional structure of the protein may be similar in these two species; this information may prove invaluable for examining the function of ASIC1 and the design of potent and selective ASIC1 inhibitors.
ASICs are highly enriched in the nervous system13,15,28. The combined results of studies involving in situ hybridization, immunohistochemistry and electrophysiology demonstrate that ASIC1a, ASIC2a, and ASIC2b are widely distributed in both the central and peripheral nervous systems13,15,17,29. By contrast, ASIC3 is preferentially expressed in dorsal root ganglion (DRG) neurons30, suggesting its potential involvement in nociception in the peripheral nervous system.
ASICs are proton-gated, voltage-independent cation channels. Different ASIC isoforms have distinct sensitivities to reductions in extracellular pH. For instance, ASIC1a and ASIC3 are the subunits that are most sensitive to H+, as these proteins can respond to pH levels that drop below 7.013,31,32. ASIC2a has the lowest sensitivity to reductions in extracellular pH; this protein has a pH0.5 of approximately 4.4, and its channels remain closed even at a local pH of 6.029,30. Homomeric ASIC2b and ASIC4 are completely insensitive to extracellular pH reductions29,33,34. ASIC activation is typically characterized by a transient inward current. Of the ASIC proteins, the desensitization of ASIC1a occurs most rapidly, with a time constant of 1–2 s13. ASIC2a desensitizes more slowly than ASIC1a, whereas ASIC3 has a non-desensitized current component that persists during prolonged acidosis30,31. It is worth noting that the properties of ASICs can be dramatically modulated by ischemia-related signaling molecules35.
ASICs are generally highly permeable to Na+ and almost impermeable to Ca2+; however, the homomeric ASIC1a demonstrates Ca2+ conductance13,16,25,36. The increase of Ca2+ concentration in the cell is critical for a number of physiological functions of neurons. However, Ca2+ overload can cause neuronal injury or death in the context of various neurological disorders, such as stroke37,38,39. The Ca2+ conductance of homomeric ASIC1a implies that this complex performs specific functions in Ca2+-related physiological and pathological processes.
Protons are the traditional agonists for ASICs; however, the existence of other endogenous activators cannot be excluded. Certain ASIC subunits, such as ASIC2b and ASIC4, form homomeric channels that cannot be gated by protons, and the potential role of ASICs in mechanoperception raises the possibility that ASIC ligands other than protons may exist40,41,42. This hypothesis is further supported by the recent identifications of a small molecule non-proton ligand 2-guanidine-4-methylquinazoline that activates ASIC3 and a toxin from the Texas coral snake that activates ASIC1a in the absence of acid19,43.
The pathological significance of ASICs in stroke
The detailed physiological functions of ASICs have been discussed in previous publications24,41,44.
In addition to fulfilling important physiological functions, ASICs are also well-known for their involvement in certain pathological conditions, most notably stroke/brain ischemia16,17,45,46. Due to the conductance of Ca2+, ASIC1a channels have been shown to contribute to the Ca2+ overload and subsequent neuronal injury that occur in brain ischemia. The activation of homomeric ASIC1a channels may cause Ca2+ overload not only through the direct conductance of Ca2+ but also through the indirect activation of NMDA receptors, which occurs as a result of the depolarization of the neuronal membrane. Amiloride, a nonspecific ASIC inhibitor, and PcTX1, a specific homomeric ASIC1a channel inhibitor, have been demonstrated to significantly protect neurons against oxygen-glucose deprivation and acid-induced injury in vitro16,47. Moreover, in mice and rats, these inhibitors dramatically reduced the volume of the infarcts that were induced by middle cerebral artery occlusion (MCAO). Additionally, ASIC1a knockout mice were resistant to MCAO-induced neuronal injury, further confirming that ASIC1a activation plays an important role in the pathophysiology of brain ischemia/stroke16. A particularly intriguing finding was that the ASIC1a inhibitor PcTX1 has a therapeutic time window of 5 h48,49, which is longer than the therapeutic time windows of 3 h and 1 h for tissue plasminogen activator and NMDA receptor antagonists, respectively50,51. As the present strategy to treat stroke remains limited to the use of preventative measures, the restoration of blood supply to the affected regions, and the implementation of procedures to decrease patient metabolism, small molecule inhibitors of ASIC1a may represent promising novel neuroprotective agents for stroke intervention.
The pharmacological characterization and therapeutic potential of small molecule inhibitors of ASICs
The function of many ion channels, including ASICs, can often be modulated by metal ions, including Zn2+, Ca2+, Mg2+, and Cu2+, among others35. However, metal ions cannot be effectively used to treat ASIC-related diseases because of their diverse physiological functions and poor selectivity. In addition to metal ions, certain naturally occurring venom polypeptides could also modulate ASICs. For instance, PcTX1, a polypeptide purified from the venom of the south American tarantula Psalmopoeus cambridgei, can specifically and potently inhibit homomeric ASIC1a current52 by promoting a desensitized state of ASIC1a53, while APETx2, a sea anemone toxin, is a potent inhibitor of ASIC3 channels54. By contrast, the toxin of the Texas coral snake can activate ASIC1a at neutral pH19. Although all of these polypeptides constitute good pharmacological tools for elucidating the functions of ASICs, they cannot be employed in clinical practice to treat neurological disorders such as stroke because their large molecular size limits their penetration across the blood-brain barrier (BBB)55. However, small molecule compounds can penetrate the BBB and have been used successfully in treating certain disorders of the CNS. Thus, small molecule inhibitors that target ASICs may represent promising therapeutic agents for the treatment of stroke.
Amiloride
Amiloride, which blocks ENaC, Na+/H+exchanger, and Na+/Ca2+ exchanger, was once used as a diuretic agent56,57. In addition, amiloride is a nonspecific blocker of ASICs that inhibits ASIC1a, ASIC1b and ASIC2a current with an IC50 of approximately 10–20 μmol/L and inhibits the transient ASIC3 current with an IC50 of approximately 60 μmol/L13,30,58,59. However, the sustained ASIC3 current is completely resistant to amiloride30,60. In fact, a study has reported that amiloride slightly potentiated the sustained ASIC3 current in cardiac sensory neurons61. Nevertheless, in the absence of more specific ASIC inhibitors or modulators, amiloride, in conjunction with molecular biology approaches, is a useful pharmacological tool for studying the functions of ASICs.
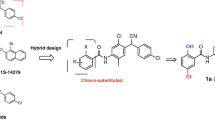
Consistent with its role as an ASIC inhibitor, amiloride has been shown to be capable of suppressing acid-induced pain in the peripheral sensory system and reducing acid-mediated ischemic neuronal injury and axonal degeneration in the CNS14,62,63. These effects support the potential of using amiloride for the treatment of certain neurological disorders. However, from a therapeutic point of view, the use of amiloride may be limited by its poor selectivity for ASICs and its interactions with the other ion channels/ion exchangers mentioned above. For instance, the Na+/Ca2+ exchanger is critical for normal neuronal function and survival because it maintains the stable homeostasis of intracellular Ca2+ concentrations. If the function of this exchanger is compromised by amiloride, a transient physiological Ca2+ influx may produce a lethal Ca2+ overload, a well-known pathological process that causes neuronal injury and death55. The inhibitory effect of amiloride on the Na+/Ca2+ exchanger may be partially responsible for the death of cultured cortical neurons that are incubated with amiloride in vitro for 5 h16,55. This effect may also explain the fact that PcTX1 (a specific ASIC1a inhibitor) produces a greater neuroprotective effect than amiloride in in vivo studies of cerebral ischemia16. Although amiloride itself may not be an ideal agent for combating neurological disorders such as stroke, its use has provided important information regarding the structure and activity of ASICs. Further structural modifications of amiloride with the goal of obtaining a more selective and potent ASIC1a inhibitor may facilitate the identification of ideal agents for the treatment of stroke.
A-317567
A-317567 is a non-specific small molecule inhibitor of ASICs that is structurally unrelated to amiloride64. In contrast to amiloride, this compound can inhibit the sustained ASIC3 current64, a current component closely associated with chronic pain sensations. The inhibitory effect of A-317567 on sustained ASIC3 current may partially explain the fact that A-317567 demonstrates greater efficacy than amiloride in reducing acid-induced pain64.
A-317567 has no diuretic or natriuretic effect and has little influence on other members of the ENaC superfamily. Therefore, this molecule appears to have a higher selectivity for ASICs than amiloride; however, it is not yet known whether A-317567 can influence other channels or membrane receptors. In addition to relieving chronic pain, A-317567 might have the potential for treating ischemic stroke due to its potent inhibition on ASIC1a-like current (IC50: ∼2 μmol/L). However, there has been a lack of direct experimental evidence that confirms its neuroprotective activity either in vitro or in vivo. The poor penetration of A-317567 across the BBB may limit its use in the treatment of neurological disorders in the CNS64, although the BBB may be compromised in certain conditions, such as ischemic stroke. The pursuit of further structural modifications to improve the lipophilic properties of A-317567 without decreasing its potency and selectivity may be a promising strategy for producing efficacious agents for stroke treatment.
Non-steroidal anti-inflammatory (NSAIDs) drugs
Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used in clinical practice to relieve pain and treat inflammatory diseases. Furthermore, low dosages of aspirin are routinely used to prevent ischemic stroke by reducing patients' risk of having blood clot65. The well-known mechanism underlying the analgesic effects is the inhibition of cyclooxygenase enzyme (COX) activity by NSAIDs. However, other mechanism(s) may exist, given the fact that NSAIDs appear to retain their analgesic activity even if COX is inhibited or knocked out66,67.
Recently, it has been demonstrated that some NSAIDs, ibuprofen and flurbiprofen for example, can inhibit ASIC3 current and ASIC3 expression in the peripheral nervous system at clinically relevant concentrations68. This observation may disclose a novel mechanism that mediates the analgesic effect of NSAIDs, as the activation of ASIC3 is associated with multiple painful sensations9,19,69. In addition to their effects on ASIC3, certain NSAIDs can also inhibit ASIC1a or ASIC1a-like current. For instance, aspirin can rapidly and reversibly inhibit 83.7% of the peak ASIC current in cultured rat cortical neurons at 3 mmol/L70, a concentration that can be reached in clinical use. Ibuprofen and flurbiprofen can inhibit ASIC1a current with an IC50 of approximately 350 μmol/L68. The inhibitory effects of NSAIDs on ASIC1a current imply that these molecules are potential therapeutic agents for the treatment of ischemic stroke. However, high dosages of NSAIDs may increase the incidence of intracerebral hemorrhages, which can produce adverse consequences in cases of stroke; this potential drawback of NSAIDs should therefore be considered in analyses of the therapeutic uses of these molecules.
Diamidines
Aromatic diamidines are synthetic small molecules that bind to the minor groove of DNA71. These compounds have traditionally been used to treat leishmaniasis, trypanosomiasis, pneumocystis pneumonia and babesiosis72. Recently, Chen and colleagues performed a small-scale screen of aromatic diamidines to search for potent ASIC inhibitors. These researchers found that 4',6-diamidino-2-phenylindole (DAPI), diminazene, hydroxystilbamidine (HSB) and pentamidine potently inhibit the ASIC current in primary cultured hippocampal neurons with IC50 values of 2.8±0.7 μmol/L, 0.29±0.11 μmol/L, 1.5±0.6 μmol/L, and 38±11 μmol/L, respectively73. These compounds have more potent inhibitory effects on ASICs compared with amiloride, which has an IC50 for ASIC current of 10–20 μmol/L and completely blocks neuronal ASIC currents at concentrations of 200–500 μmol/L74,75. The co-application of diminazene with acidic solution could also shorten the desensitization time constant of ASICs73, suggesting that diminazene may promote ASIC closure. Interestingly, this effect appears to be specific to diminazene, as other aromatic diminazenes do not have effects on the desensitization rate of ASIC currents. Currently, diminazene is the most potent known small molecular inhibitor of ASICs. Its neuroprotective effects, however, have not been demonstrated directly, either in vitro or in vivo.
Although ASICs share considerable homology with ENaC proteins, even the high concentration of 100 μmol/L of diminazene has no effect on ENaCs73, implying that diminazene has a higher selectivity for ASICs than amiloride. Furthermore, the long-term clinical use of diminazene for treating the diseases mentioned above suggests that this drug is relatively safe and has a low probability of causing intolerable side effects. However, diminazene still displays poor selectivity among the ASICs, and its highly hydrophilic nature may limit its penetration across the BBB72. Both of these concerns may limit the usefulness of diminazene in the treatment of stroke. DB829, the first aromatic diamidine derivative, can penetrate the BBB via an unknown transporter72. However, the toxicity and efficacy studies of DB829 have not been completed, and its effect on ASICs is unknown. It may be possible to construct a chimeric molecule that contains the diamidine functional group to inhibit ASIC1a channels and the critical group of DB829 to enhance penetration of the BBB.
Local anesthetics
Local anesthetics have various effects, including antiarrhythmia, antinociception, neuroprotection and analgesia76. The blocking of voltage-gated Na+ channels is a well-known mechanism shared by many local anesthetics77. However, the multiple effects of these molecules cannot be explained solely in terms of the blocking of voltage-gated sodium channels. Other mechanisms must be involved in anesthetic effects, particularly during severe acidosis, as the activities of voltage-gated sodium channels, the primary target of local anesthetics, are significantly suppressed by protons78,79.
Recently, we demonstrated that lidocaine could reversibly inhibit ASIC1a current without affecting ASIC2a current76. Similarly, tetracaine can inhibit ASIC1a current in a use-dependent manner80. Moreover, this anesthetic can inhibit both the transient and sustained ASIC3 currents without significantly affecting ASIC2a current80. By contrast, other amide-based local anesthetics, such as mepivacaine, bupivacaine, and ropivacine, can block voltage-gated sodium channels but do not affect ASICs76. The concentration of lidocaine that is sufficient for the inhibition of ASIC1a can be achieved in clinical practice through direct local exposure76. Thus, lidocaine could be a potential candidate for stroke intervention. However, it has not yet been determined whether the potential side effects caused by the blockade of voltage-gated Na+ channels would be minimal enough to allow lidocaine to be systemically used for the treatment of stroke. Undoubtedly, the triple blockage of voltage-gated Na+ channels, ASIC1a channels and ASIC3 channels by tetracaine endows this molecule with the potential for being a potent painkiller. In addition, the use-dependent inhibition of ASIC1a by tetracaine makes it particularly effective at suppressing the higher-frequency activations of ASIC1a, which implies that this molecule will have a greater impact on abnormal ASIC1a activity than on the physiological functions of ASIC1a.
Conclusion
The lack of effective treatments for stroke damage emphasizes the urgent need for a better understanding of brain injury mechanisms and a wider range of neuroprotective agents. The targeting of ASICs by small molecule inhibitors may represent a promising strategy for combating ASIC-related neurodegenerative diseases, such as stroke. These neuroprotective agents should ideally not only display high selectivity and efficacy in the inhibition of ASIC1a channels but also possess the capability to effectively penetrate the BBB. The small molecule inhibitors of ASICs that are currently available display low selectivity for any specific ASIC subunit. Although the inhibition of Ca2+-permeable ASIC1a channels can provide neuroprotection, the blockade of other isoforms of ASICs may induce undesirable side effects. Moreover, a highly selective ASIC1a inhibitor may still produce side effects, as the complete inhibition of this channel may interfere with the important physiological functions of its channels; this lesson can be learned from the clinical failure of many putative NMDA receptor antagonists. Thus, a mild modulator that can attenuate the over-activation of ASICs but retain the physiological functions of these channels may be a good candidate for a stroke treatment drug. Finally, a large-scale structure-activity relationship study, based on the presently available structural data regarding ASIC1a inhibitors and the known crystal structure of ASIC1a, may expedite the search for a highly selective, potent and lipophilic small molecule that can effectively treat ischemic stroke.
References
Chesler M . The regulation and modulation of pH in the nervous system. Prog Neurobiol 1990; 34: 401–27.
Nedergaard M, Kraig RP, Tanabe J, Pulsinelli WA . Dynamics of interstitial and intracellular pH in evolving brain infarct. Am J Physiol 1991; 260: R581–R588.
Miesenbock G, De Angelis DA, Rothman JE . Visualizing secretion and synaptic transmission with pH-sensitive green fluorescent proteins. Nature 1998; 394: 192–5.
Krishtal OA, Osipchuk YV, Shelest TN, Smirnoff SV . Rapid extracellular pH transients related to synaptic transmission in rat hippocampal slices. Brain Res 1987; 436: 352–6.
Chesler M, Kaila K . Modulation of pH by neuronal activity. Trends Neurosci 1992; 15: 396–402.
Rehncrona S . Brain acidosis. Ann Emerg Med 1985; 14: 770–6.
Somjen GG . Acidification of interstitial fluid in hippocampal formation caused by seizures and by spreading depression. Brain Res 1984; 311: 186–8.
Wang RI, Sonnenschein RR . PH of cerebral cortex during induced convulsions. J Neurophysiol 1955; 18: 130–7.
Deval E, Gasull X, Noel J, Salinas M, Baron A, Diochot S, et al. Acid-sensing ion channels (ASICs): pharmacology and implication in pain. Pharmacol Ther 2010; 128: 549–58.
Kaku DA, Giffard RG, Choi DW . Neuroprotective effects of glutamate antagonists and extracellular acidity. Science 2010; 260: 1516–8.
Siesjo BK . Acidosis and ischemic brain damage. Neurochem Pathol 1988; 9: 31–88.
Nedergaard M, Goldman SA, Desai S, Pulsinelli WA . Acid-induced death in neurons and glia. J.Neurosci 1991; 11: 2489–97.
Waldmann R, Champigny G, Bassilana F, Heurteaux C, Lazdunski M . A proton-gated cation channel involved in acid-sensing. Nature 1997; 386: 173–7.
Ugawa S, Ueda T, Ishida Y, Nishigaki M, Shibata Y, Shimada S . Amiloride-blockable acid-sensing ion channels are leading acid sensors expressed in human nociceptors. J Clin Invest 2002; 110: 1185–90.
Wemmie JA, Chen J, Askwith CC, Hruska-Hageman AM, Price MP, Nolan BC, et al. The acid-activated ion channel ASIC contributes to synaptic plasticity, learning, and memory. Neuron 2002; 34: 463–77.
Xiong ZG, Zhu XM, Chu XP, Minami M, Hey J, Wei WL, et al. Neuroprotection in ischemia: blocking calcium-permeable acid-sensing ion channels. Cell 2004; 118: 687–98.
Duan B, Wang YZ, Yang T, Chu XP, Yu Y, Huang Y, et al. Extracellular spermine exacerbates ischemic neuronal injury through sensitization of ASIC1a channels to extracellular acidosis. J Neurosci 2011; 31: 2101–12.
Andreev YA, Vassilevski AA, Kozlov SA . Molecules to selectively target receptors for treatment of pain and neurogenic inflammation. Recent Pat Inflamm Allergy Drug Discov 2012; 6: 35–45.
Bohlen CJ, Chesler AT, Sharif-Naeini R, Medzihradszky KF, Zhou S, King D, et al. A heteromeric Texas coral snake toxin targets acid-sensing ion channels to produce pain. Nature 2011; 479: 410–4.
Deval E, Noel J, Gasull X, Delaunay A, Alloui A, Friend V, et al. Acid-sensing ion channels in postoperative pain. J Neurosci 2011; 31: 6059–66.
Ziemann AE, Schnizler MK, Albert GW, Severson MA, Howard MA III, Welsh MJ, et al. Seizure termination by acidosis depends on ASIC1a. Nat Neurosci 2008; 11: 816–22.
Lv RJ, He JS, Fu YH, Zhang YQ, Shao XQ, Wu LW, et al. ASIC1a polymorphism is associated with temporal lobe epilepsy. Epilepsy Res 2011; 96: 74–80.
Alvarez d lR, Canessa CM, Fyfe GK, Zhang P . Structure and regulation of amiloride-sensitive sodium channels. Annu Rev Physiol 2000; 62: 573–94.
Grunder S, Chen X . Structure, function, and pharmacology of acid-sensing ion channels (ASICs): focus on ASIC1a. Int J Physiol Pathophysiol Pharmacol 2010; 2: 73–94.
Waldmann R, Lazdunski M . H(+)-gated cation channels: neuronal acid sensors in the NaC/DEG family of ion channels. Curr Opin Neurobiol 1998; 8: 418–24.
Krishtal O . The ASICs: signaling molecules? Modulators? Trends Neurosci 2003; 26: 477–83.
Jasti J, Furukawa H, Gonzales EB, Gouaux E . Structure of acid-sensing ion channel 1 at 1.9 A resolution and low pH. Nature 2007; 449: 316–23.
Alvarez d lR, Krueger SR, Kolar A, Shao D, Fitzsimonds RM, Canessa CM . Distribution, subcellular localization and ontogeny of ASIC1 in the mammalian central nervous system. J Physiol 2003; 546: 77–87.
Lingueglia E, de Weille JR, Bassilana F, Heurteaux C, Sakai H, Waldmann R, et al. A modulatory subunit of acid sensing ion channels in brain and dorsal root ganglion cells. J Biol Chem 1997; 272: 29778–83.
Waldmann R, Bassilana F, de Weille J, Champigny G, Heurteaux C, Lazdunski M . Molecular cloning of a non-inactivating proton-gated Na+ channel specific for sensory neurons. J Biol Chem 1997; 272: 20975–8.
Sutherland SP, Benson CJ, Adelman JP, McCleskey EW . Acid-sensing ion channel 3 matches the acid-gated current in cardiac ischemia-sensing neurons. Proc Natl Acad Sci U S A 2001; 98: 711–6.
Ziemann AE, Allen JE, Dahdaleh NS, Drebot II, Coryell MW, Wunsch AM, et al. The amygdala is a chemosensor that detects carbon dioxide and acidosis to elicit fear behavior. Cell 2009; 139: 1012–21.
Grunder S, Geissler HS, Bassler EL, Ruppersberg JP . A new member of acid-sensing ion channels from pituitary gland. Neuroreport 2000; 11: 1607–11.
Akopian AN, Chen CC, Ding Y, Cesare P, Wood JN . A new member of the acid-sensing ion channel family. Neuroreport 2000; 11: 2217–22.
Chu XP, Papasian CJ, Wang JQ, Xiong ZG . Modulation of acid-sensing ion channels: molecular mechanisms and therapeutic potential. Int J Physiol Pathophysiol Pharmacol 2011; 3: 288–309.
Bassler EL, Ngo-Anh TJ, Geisler HS, Ruppersberg JP, Grunder S . Molecular and functional characterization of acid-sensing ion channel (ASIC) 1b. J Biol Chem 2001; 276: 33782–7.
Choi DW . Calcium-mediated neurotoxicity: relationship to specific channel types and role in ischemic damage. Trends Neurosci 1988; 11: 465–9.
Choi DW . Excitotoxic cell death. J Neurobiol 1992; 23: 1261–76.
Sattler R, Tymianski M . Molecular mechanisms of glutamate receptor-mediated excitotoxic neuronal cell death. Mol Neurobiol 2001; 24: 107–29.
Sole-Magdalena A, Revuelta EG, Menenez-Diaz I, Calavia MG, Cobo T, Garcia-Suarez O, et al. Human odontoblasts express transient receptor protein and acid-sensing ion channel mechanosensor proteins. Microsc Res Tech 2011; 74: 457–63.
Wemmie JA, Price MP, Welsh MJ . Acid-sensing ion channels: advances, questions and therapeutic opportunities. Trends Neurosci 2006; 29: 578–86.
Page AJ, Brierley SM, Martin CM, Price MP, Symonds E, Butler R, et al. Different contributions of ASIC channels 1a, 2, and 3 in gastrointestinal mechanosensory function. Gut 2005; 54: 1408–15.
Yu Y, Chen Z, Li WG, Cao H, Feng EG, Yu F, et al. A nonproton ligand sensor in the acid-sensing ion channel. Neuron 2010; 68: 61–72.
Chu XP, Xiong ZG . Physiological and pathological functions of acid-sensing ion channels in the central nervous system. Curr Drug Targets 2012; 13: 263–71.
Gao J, Duan B, Wang DG, Deng XH, Zhang GY, Xu L, et al. Coupling between NMDA receptor and acid-sensing ion channel contributes to ischemic neuronal death. Neuron 2005; 48: 635–46.
Pignataro G, Cuomo O, Esposito E, Sirabella R, Di Renzo G, Annunziato L . ASIC1a contributes to neuroprotection elicited by ischemic preconditioning and postconditioning. Int J Physiol Pathophysiol Pharmacol 2011; 3: 1–8.
Yermolaieva O, Leonard AS, Schnizler MK, Abboud FM, Welsh MJ . Extracellular acidosis increases neuronal cell calcium by activating acid-sensing ion channel 1a. Proc Natl Acad Sci U S A 2004; 101: 6752–7.
Pignataro G, Simon RP, Xiong ZG . Prolonged activation of ASIC1a and the time window for neuroprotection in cerebral ischaemia. Brain 2007; 130: 151–8.
Simon RP . Acidotoxicity trumps excitotoxicity in ischemic brain. Arch Neurol 2006; 63: 1368–71.
MacDonald JF, Xiong ZG, Jackson MF . Paradox of Ca2+ signaling, cell death and stroke. Trends Neurosci 2006; 29: 75–81.
Moskowitz MA, Lo EH, Iadecola C . The science of stroke: mechanisms in search of treatments. Neuron 2010; 67: 181–98.
Escoubas P, de Weille JR, Lecoq A, Diochot S, Waldmann R, Champigny G, et al. Isolation of a tarantula toxin specific for a class of proton-gated Na+ channels. J Biol Chem 2000; 275: 25116–21.
Chen X, Kalbacher H, Grunder S . The tarantula toxin psalmotoxin 1 inhibits acid-sensing ion channel (ASIC) 1a by increasing its apparent H+ affinity. J Gen Physiol 2005; 126: 71–9.
Diochot S, Baron A, Rash LD, Deval E, Escoubas P, Scarzello S, et al. A new sea anemone peptide, APETx2, inhibits ASIC3, a major acid-sensitive channel in sensory neurons. EMBO J 2004; 23: 1516–25.
Xiong ZG, Pignataro G, Li M, Chang SY, Simon RP . Acid-sensing ion channels (ASICs) as pharmacological targets for neurodegenerative diseases. Curr Opin Pharmacol 2008; 8: 25–32.
Canessa CM, Schild L, Buell G, Thorens B, Gautschi I, Horisberger JD, et al. Amiloride-sensitive epithelial Na+ channel is made of three homologous subunits. Nature 1994; 367: 463–7.
Kleyman TR, Cragoe EJ Jr . Amiloride and its analogs as tools in the study of ion transport. J Membr Biol 1988; 105: 1–21.
Chen CC, Zimmer A, Sun WH, Hall J, Brownstein MJ, Zimmer A . A role for ASIC3 in the modulation of high-intensity pain stimuli. Proc Natl Acad Sci U S A 2002; 99: 8992–7.
Bassilana F, Champigny G, Waldmann R, de Weille JR, Heurteaux C, Lazdunski M . The acid-sensitive ionic channel subunit ASIC and the mammalian degenerin MDEG form a heteromultimeric H+-gated Na+ channel with novel properties. J Biol Chem 1997; 272: 28819–22.
Benson CJ, Eckert SP, McCleskey EW . Acid-evoked currents in cardiac sensory neurons: A possible mediator of myocardial ischemic sensation. Circ Res 1999; 84: 921–8.
Yagi J, Wenk HN, Naves LA, McCleskey EW . Sustained currents through ASIC3 ion channels at the modest pH changes that occur during myocardial ischemia. Circ Res 2006; 99: 501–9.
Jones NG, Slater R, Cadiou H, McNaughton P, McMahon SB . Acid-induced pain and its modulation in humans. J Neurosci 2004; 24: 10974–9.
Sluka KA, Price MP, Breese NM, Stucky CL, Wemmie JA, Welsh MJ . Chronic hyperalgesia induced by repeated acid injections in muscle is abolished by the loss of ASIC3, but not ASIC1. Pain 2003; 106: 229–39.
Dube GR, Lehto SG, Breese NM, Baker SJ, Wang X, Matulenko MA, et al. Electrophysiological and in vivo characterization of A-317567, a novel blocker of acid sensing ion channels. Pain 2005; 117: 88–96.
van der Worp HB, van Gijn J . Clinical practice. Acute ischemic stroke. N Engl J Med 2007; 357: 572–9.
Ballou LR, Botting RM, Goorha S, Zhang J, Vane JR . Nociception in cyclooxygenase isozyme-deficient mice. Proc Natl Acad Sci U S A 2000; 97: 10272–6.
Brune K, Beck WS, Geisslinger G, Menzel-Soglowek S, Peskar BM, Peskar BA . Aspirin-like drugs may block pain independently of prostaglandin synthesis inhibition. Experientia 1991; 47: 257–61.
Voilley N, de Weille J, Mamet J, Lazdunski M . Nonsteroid anti-inflammatory drugs inhibit both the activity and the inflammation-induced expression of acid-sensing ion channels in nociceptors. J Neurosci 2001; 21: 8026–33.
Deval E, Noel J, Lay N, Alloui A, Diochot S, Friend V, et al. ASIC3, a sensor of acidic and primary inflammatory pain. EMBO J 2008; 27: 3047–55.
Wang W, Ye SD, Zhou KQ, Wu LM, Huang YN . High doses of salicylate and aspirin are inhibitory on acid-sensing ion channels and protective against acidosis-induced neuronal injury in the rat cortical neuron. J Neurosci Res 2012; 90: 267–77.
Neidle S . DNA minor-groove recognition by small molecules. Nat Prod Rep 2001; 18: 291–309.
Chen X, Orser BA, MacDonald JF . Design and screening of ASIC inhibitors based on aromatic diamidines for combating neurological disorders. Eur J Pharmacol 2010; 648: 15–23.
Chen X, Qiu L, Li M, Durrnagel S, Orser BA, Xiong ZG, et al. Diarylamidines: high potency inhibitors of acid-sensing ion channels. Neuropharmacology 2010; 58: 1045–53.
Baron A, Waldmann R, Lazdunski M . ASIC-like, proton-activated currents in rat hippocampal neurons. J Physiol 2002; 539: 485–94.
Wu LJ, Duan B, Mei YD, Gao J, Chen JG, Zhuo M, et al. Characterization of acid-sensing ion channels in dorsal horn neurons of rat spinal cord. J Biol Chem 2004; 279: 43716–24.
Lin J, Chu X, Maysami S, Li M, Si H, Cottrell JE, et al. Inhibition of acid sensing ion channel currents by lidocaine in cultured mouse cortical neurons. Anesth Analg 2011; 112: 977–81.
Butterworth JF, Strichartz GR . Molecular mechanisms of local anesthesia: a review. Anesthesiology 1990; 72: 711–34.
Mozhayeva GN, Naumov AP, Nosyreva ED . A study on the potential-dependence of proton block of sodium channels. Biochim Biophys Acta 1990; 775: 435–40.
Jones DK, Peters CH, Tolhurst SA, Claydon TW, Ruben PC . Extracellular proton modulation of the cardiac voltage-gated sodium channel, Nav1.5. Biophys J 2011; 101: 2147–56.
Leng TD, Lin J, Weiss A, Cottrell JE, Xiong ZG . Acid sensing ion channel are modulated by local anesthetics. Society for neuroscience, Abstract 2011; 139: 10.
Acknowledgements
The work in Dr Zhi-gang XIONG's laboratory was partially supported by NIH R01NS047506, R01NS066027, NIMHD S21MD000101, U54 RR026137, AHA 0840132N, and ALZ IIRG-10-173350.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leng, Td., Xiong, Zg. The pharmacology and therapeutic potential of small molecule inhibitors of acid-sensing ion channels in stroke intervention. Acta Pharmacol Sin 34, 33–38 (2013). https://doi.org/10.1038/aps.2012.81
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2012.81
Keywords
This article is cited by
-
Regulating Factors in Acid-Sensing Ion Channel 1a Function
Neurochemical Research (2016)
-
Down-Regulated Expression of Acid-Sensing Ion Channel 1a in Cortical Lesions of Patients with Focal Cortical Dysplasia
Journal of Molecular Neuroscience (2014)