Abstract
Neonatal Encephalopathy (NE) is a major cause of lifelong disability and neurological complications in affected infants. Identifying novel diagnostic biomarkers in this population may assist in predicting MRI injury and differentiate neonates with NE from those with low-cord pH or healthy neonates and may help clinicians make real-time decisions. To compare the microRNA (miRNA) profiles between neonates with NE, healthy controls, and neonates with low cord pH. Moreover, miRNA concentrations were compared to brain injury severity in neonates with NE. This is a retrospective analysis of miRNA profiles from select samples in the biorepository and data registry at the University of Florida Health Gainesville. The Firefly miRNA assay was used to screen a total of 65 neurological miRNA targets in neonates with NE (n = 36), low cord pH (n = 18) and healthy controls (n = 37). Multivariate statistical techniques, including principal component analysis and orthogonal partial least squares discriminant analysis, and miRNA Enrichment Analysis and Annotation were used to identify miRNA markers and their pathobiological relevance. A set of 10 highly influential miRNAs were identified, which were significantly upregulated in the NE group compared to healthy controls. Of these, miR-323a-3p and mir-30e-5p displayed the highest fold change in expression levels. Moreover, miR-34c-5p, miR-491-5p, and miR-346 were significantly higher in the NE group compared to the low cord pH group. Furthermore, several miRNAs were identified that can differentiate between no/mild and moderate/severe injury in the NE group as measured by MRI. MiRNAs represent promising diagnostic and prognostic tools for improving the management of NE.
Similar content being viewed by others
Introduction
MicroRNAs (miRNAs) are small endogenous RNA molecules that regulate translation in eukaryotic cells at the post-transcriptional level. They bind to their target mRNAs to induce translational repression or degradation1,2,3. MiRNAs are small, released into the extracellular space, resistant to degradation, and easily detected3,4. These attributes highlight their suitability as biomarker candidates for neonatal encephalopathy (NE). Unlike neuroproteins, miRNAs are detectable at very small concentrations. Since several miRNAs are involved in normal brain development, alterations in their expression may be implicated in conditions like NE.
NE is a major cause of lifelong disability in affected infants, causing profound distress for families and driving huge costs for healthcare systems5. The clinical management of neonates with NE is complex. Biomarkers capable to inform treatment, monitor injury progression, and predict outcomes are urgently needed. Currently, there is an active effort to develop neuroprotein-based biomarkers to assist the bedside clinician with real-time decision making such as treatment initiation6,7,8,9,10,11,12. MiRNAs may provide complementary information enabling clinicians to characterize and stratify risk among neonates with NE13,14,15,16,17.
This study aims to assess the miRNA profiles in neonates with NE undergoing therapeutic hypothermia and compare them to healthy controls and neonates with a low cord pH. We hypothesized that miRNA expression levels would differentiate between neonates with moderate to severe NE compared to the control and low cord pH populations. Moreover, we aimed to assess miRNA expression in NE neonates who underwent hypothermia according to brain injury severity.
Materials and methods
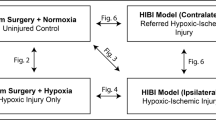
Study design and setting
This is a retrospective observational cohort study of miRNA profiles from select specimens collected between December 2013 and May 2019 and obtained from the Florida Neonatal Neurologic Network registry and biorepository as previously reported18,19. The University of Florida Institutional Review Board approved the study (IRB#201501109, IRB201802816).
Participants
Neonatal encephalopathy (NE) group
To identify subjects with NE, data were extracted from the electronic medical records and recorded in the REDCap electronic data capture tools20. From each patient in the NE group, two samples were retrieved from the biorepository and analyzed. The first sample was collected 0–6 h after birth, and the second sample was collected 48 h after birth. These timepoints coincided with the time before hypothermia (0–6 h) or at the initiation of hypothermia and during hypothermia (48 h).
Specimens were selected by NE outcome based on magnetic resonance imaging (MRI) results and categorized into no/mild brain injury (n = 18) and moderate/severe injury (n = 18) groups.
Low umbilical cord pH with or without evidence of mild NE
The alteration in umbilical cord pH, namely acidosis, reflects hypoxic stress in the fetus. Low cord pH, as an isolated finding, is not a predictor of hypoxic ischemic injury. However, low cord pH combined with other abnormal clinical findings is associated with adverse neonatal outcomes. Hence, we included a sample of 18 neonates with low umbilical cord pH to determine whether their miRNA expression profile differed compared with neonates with NE. The low umbilical cord pH group included neonates with a cord pH ≤ 7.1 who did not develop moderate to severe NE. They were transitioned to the NICU for closer monitoring, collection of clinical labs, and amplitude-integrated electroencephalography (aEEG) monitoring.
Neonates with a normal neurologic exam, normal labs, and/or an aEEG with no evidence of hypoxic-ischemic injury for the six-hour monitoring period were transferred back to the mothers, regardless of the pH. One blood sample was collected at 0–6 h of life from scavenged blood and stored in the biorepository.
Control subjects
A total of 37 healthy neonates were included in the study. The eligibility criteria for controls included an Apgar score of eight or higher at one and five minutes of life (i), no evidence of encephalopathy (ii), and admission to the newborn nursery (iii). One blood sample was collected at birth from each patient’s umbilical cord from scavenged blood and later obtained for analysis from the biorepository18,19. Umbilical arterial samples were targeted. Of the 37 control samples, 25 were labeled as mixed because the arterial samples may have been contaminated by some umbilical venous blood at the time of sampling, five samples were definitively umbilical arterial and six samples were definitively labeled as umbilical venous. A single sample was not labeled.
MicroRNA profiling
Blood samples (1 ml) were centrifuged at 1200 g for 15 min. The resulting sera were transferred into 2 ml cryovials and stored at − 80 °C until assay analysis. The Firefly miRNA particle assay system was used for miRNA measurement, coupled with a portable flow cytometer/reader (Guava® easyCyte™ 6HT, Millipore, Burlington, MA). RNA extraction was performed by incubating 20 µl serum with 40 µl Lysis Mix and 20 µl nuclease-free water for 45 min at 60 °C while shaking. Then, the extracted RNA was analyzed with the FirePlex™ miRNA neurology panel V2 (cat# ab218371, Abcam, Waltham, MA) as described previously (PMC9301366).
Magnetic resonance imaging (MRI) scoring
In neonates with NE, MRIs were performed at either 4–5 days of age following rewarming (n = 30) or at 7–12 days of age (n = 6) if the babies were not stable enough for transport to MRI at 4–5 days of age. Neonates were imaged on a 3 T scanner (Siemens, Malvern, PA). The analysis focused on the T1-weighted, T2-weighted, and diffusion-weighted imaging (DWI) abnormalities. Two blinded subspecialty board-certified neuroradiologists with over 10 years of experience interpreted the MRI images using the Barkovich scoring system21. Individual brain regions scored included the basal ganglia (0–4), the watershed cortex/white matter (0–5), and combined basal ganglia/watershed (0–4). Infants with scores of 0–2 in any region were categorized as no/mild injury on MRI. Scores ≥ 3 in any region were interpreted as moderate/severe injury. Examples of neonatal brain MRI images showing injury to the basal ganglia and diffuse injury to the cortex and subcortical white matters are presented in Figure S1.
Data management and statistical analysis
No formal calculation of the sample size was performed as analyses were done retrospectively and included all neonates with NE who fulfilled the inclusion criteria. Baseline characteristics were summarized using standard descriptive statistics. Continuous variables were described as mean and standard deviation (SD), and categorical data were summarized as absolute frequencies and percentages. We compared groups using Mann–Whitney tests (two groups) and Kruskal–Wallis tests with post-hoc Dunn’s test (three groups). The association between categorical variables was evaluated using the chi-square or Fisher’s exact test, as indicated. Multivariate analysis methods were used to identify relevant patient clusters and variables responsible for class discrimination22,23. We first used principal component analysis (PCA) to lower the dimensionality of the data and to identify distinct clusters and potential outliers within the data sets. Outliers were identified using score plots in combination with Hotelling’s T2 and distance to model in X-space (DModX)24,25. Subsequently, a supervised multivariate analysis was conducted using orthogonal partial least squared discriminant analysis (OPLS-DA). OPLS-DA was used to maximize the detection of miRNA (X-variables) associated with differentiation between the predefined groups. In a subsequent modeling step, the loadings associated with each model were screened for the top 10 relevant variables using the R2VXAdj metric (i.e., explained a fraction of the variation of X variables for the predictive component). Traditional statistical analysis was performed using R (http://www.r-project.org, version 3.5.1) in RStudio (http://www.rstudio.com, version 1.1.456), and SIMCA® 16 Software (Umetrics AB, Umeå, Sweden) was used for multivariate data analysis.
Sub-network enrichment pathway analysis
To identify the potential pathobiological relevance of the identified miRNA markers that characterize NE we performed miRNA Enrichment Analysis and Annotation (miEAA) using the PathwayStudio software (Elsevier Inc. https://www.elsevier.com/solutions/pathway-studio-biological-research). To determine significantly altered functional and biological pathways for each set of identified miRNAs, the Subnetwork Enrichment Analysis (SNEA) algorithm was utilized. This algorithm uses Fisher’s exact test for the detection of nonrandom associations between two categorical variables that are organized by a specific relationship. Furthermore, the distribution of the subnetwork was compared between the inside and outside of the pathway using the Mann–Whitney test. Pathways with a P-value less than 0.05 were considered significant.
Statement of financial support
Department Development Funding.
Consent statement
Informed consent was obtained within 72 h of birth from the parents of all neonates enrolled.
Statement on study methodology
The University of Florida Institutional Review Board approved the study (IRB#201501109, IRB201802816). Informed consent was obtained for sample and data collection for all subjects enrolled in the biorepository. Blood collection from neonates was conducted in conformity with common practice as well as state and federal regulations.
Results
Description of the patient population
We studied 36 neonates with moderate to severe NE who underwent hypothermia. The mean gestational age was 38.2 weeks (SD ± 1.9), the mean birth weight was 3383 g (SD ± 867), and the cohort consisted primarily of males (61%). Neonates characteristics at enrollment were analyzed by no/mild and moderate/severe brain injury as assessed by MRI (Table 1). The Apgar scores at 5 and 10 min of life, the Sarnat scores, and the history of seizures were different between both groups (P < 0.05). The Apgar scores were lower in the moderate/severe brain injury group, which also included more infants with a stage III initial Sarnat exam and a history of seizures. Additional characteristics and details are shown in Table 1.
Moreover, a total of 37 age-matched healthy controls and 18 neonates with a low cord pH were included in this study. In the low cord pH group, all neonates had Sarnat serial exams performed between 0 and 6 h after birth. Of the 18 neonates, eight had a Sarnat exam consistent with mild NE.
When comparing the low cord pH group (n = 18) to the NE group (n = 36), there were no significant differences in gestational age, birth weight, sex, and Cesarian section (Table S2). However, the Apgar scores at 1 and 5 min of life were higher in the low cord pH group (3.8 ± 3.1 and 7.2 ± 1.8) compared to the NE group (1.80 ± 1.6 and 3.94 ± 2.4) (Table S2, P < 0.05).
Comparison of NE neonates with healthy controls and with low cord pH neonates
MiRNA profiles of neonates with moderate to severe NE who underwent hypothermia were compared to those from healthy controls using PCA (R2X = 0.67, Q2 = 0.60). A degree of natural separation was observed (Figure S2). Supervised OPLS-DA modeling maximized the variations between the two groups (R2Y = 0.91, Q2 = 0.83, p < 0.0001) (Figure S2a), with an area under the curve (AUC) of 0.99 (Figure S2b). The loadings plot indicated that different miRNAs characterized the two groups (Figure S2c).
A set of highly influential miRNAs that can differentiate between the NE group and controls was identified (Fig. 1). All were significantly upregulated in the NE group compared to the control group. Interestingly, the same significant trend was observed when comparing the low cord pH group to healthy controls. The highest fold change in miRNA levels was obtained for miR-323a-3p and mir-30e-5p.
Box-and-whisker plots of highly influential miRNA in healthy, low pH and NE neonates. The group differences are presented for 10 selected miRNAs. The black horizontal line in each box represents the median, with the boxes representing the interquartile range. Each dot represents a patient. Significant differences are indicated with *(p < 0.05), **(p < 0.01), or ***(p < 0.001) (Kruskal–Wallis test).
MiRNA profiles of neonates with NE were additionally compared to those from neonates with a low cord pH. An OPLS-DA model could be constructed (R2Y = 0.47, Q2Y = 0.28, p = 0.003) (Figure S3a), with the ability to separate the two groups with an area under the ROC curve of 0.91 (Figure S3b). The loadings plot associated with the model was screened for relevant variables (Figure S3c).
In total, three miRNAs were significantly different between low cord pH and moderate to severe NE neonates. The levels of miR-34c-5p, miR-491-5p, and miR-346 were significantly lower in the low cord pH group compared to the moderate to severe NE group and the healthy controls (Fig. 2).
Group differences for identified miRNA discriminating low cord pH and NE groups. Box-and-whisker plots of highly influential miRNA in healthy, low pH and severe HIE neonates. The black horizontal line in each box represents the median, with the boxes representing the interquartile range. Each dot represents a patient. Significant differences are indicated with *(p < 0.05), **(p < 0.01), or *** (p < 0.001) (Kruskal–Wallis test).
Comparison of brain injury as assessed by MRI
MiRNA profiles of the neonates with NE were compared according to the severity of brain injury on MRI using multivariate models. The analysis was conducted twice for samples taken before and after hypothermia. OPLS-DA models (Figure S4) could be constructed using baseline characteristics and miRNA profiles obtained before and after hypothermia (R2Y = 0.69, Q2Y = 0.41, p = 0.002 and R2Y = 0.58, Q2Y = 0.41, p = 0.003, respectively), with ability to separate the two groups with an area under the ROC curve of 0.97 and 0.996, respectively.
The loading plots revealed that the moderate/severe injury group is characterized by a higher occurrence of seizures (p < 0.0001), increased AST and ALT levels (p = 0.007), and a lower APGAR score at 5 min (p = 0.02) compared to the no/mild injury group. Hsa-mir-16-5p (p = 0.006), hsa-mir-20a-5p (p = 0.02), hsa-mir-15b-5p (p = 0.01), and hsa-mir-17-5p (p = 0.01) were significantly higherin the no/mild brain injury group compared to the moderate/severe injury group and the control groupacutely before or at the time of initiation of hypothermia (Fig. 3).
Box-and-whisker plots demonstrating MiRNA expression in blood samples taken before or at initiation of hypothermia (at 0–6 h post-birth) from NE neonates with moderate/severe injury and with no/mild injury on MRI, and in controls. The black horizontal line in each box represents the median, with the boxes representing the interquartile range. Significant differences are indicated with*(p < 0.05) or with **(P < 0.01) (Kruskal–Wallis test).
Subacutely at 48 h, during hypothermia, we demonstrated that the expression of hsa-mir-197-3p (p = 0.004), hsa-mir-342-3p (p = 0.003), hsa-mir-103a-3p (p = 0.01), hsa-mir-150-5p (p = 0.006), hsa-mir-328-3p (p = 0.0096) and hsa-mir-191-5p (p = 0.03) was significantly reduced in the moderate/severe injury group (Fig. 4).
Box-and-whisker plots demonstrating MiRNA expression in blood samples taken after hypothermia (at 48 h post-birth) from NE neonates with moderate/severe injury and with no/mild injury on MRI. The black horizontal line in each box represents the median, with the boxes representing the interquartile range. Significant differences are indicated with*(p < 0.05) with or **(P < 0.01) (Kruskal–Wallis test).
Discussion
MiRNA expression affects a plethora of biological pathways implicated in ischemic injury, including apoptosis and neuroinflammation. Investigating their role as selective biomarkers of NE is an impressive research field that has the potential to improve risk stratification in such a heterogeneous injury.
The first aim of this study was to determine miRNAs that are significantly altered within hours of life in neonates suffering from NE compared to healthy controls. The expression levels of 10 miRNAs were significantly upregulated in the NE group compared to healthy controls. The biological pathways in which these miRNAs are implicated are presented in Figure S5. Casey et al. utilized a porcine model of neonatal NE to demonstrate a significant increase in circulating miR-151a levels one-hour post-hypoxia–ischemia26. Interestingly, miR-151-a was shown to promote healing after spinal cord injury by targeting P53 to improve neuronal survival27. In response to injury, microglia release exosomes containing miR-151-a that can be taken up by neurons to attenuate cell death. This may explain the pronounced upregulation of miR-151-a-3p in NE neonates in this study. Similarly, the upregulation of miR-146a-5p in NE neonates may serve as a counteractive mechanism against neuroinflammation and oxidative stress. MiR-146a is a known negative regulator of inflammation that inhibits the interleukin-1 receptor-associated kinase 1 (IRAK1) and toll-like receptor 4 (TLR4) genes in immune cells28. Analysis utilizing the Pathway Studio software additionally predicts the role of miR-146a in the inhibition of ischemia and neuroinflammation (Figure S5). These data suggest that miR-151-a and MiR-146a may be upregulated as a defense mechanism to ameliorate portions of the pathophysiologic cascade following hypoxia–ischemia11.
Only a few studies exist comparing the miRNA concentrations between neonates with NE and those with low umbilical cord pH29. We found that in neonates with low cord pH, blood concentrations of miR34c-5p, miR491-5p, and miR346 were substantially lower than in moderate to severe NE and healthy controls. These results suggest distinct pathobiological processes underlying low cord pH and its consequences, but not NE. This is also supported by the lack of differences between low cord pH and control groups. Further studies are warranted to fully understand these findings.
Next, we investigated miRNA profile alterations in NE neonates requiring therapeutic hypothermia according to MRI brain injury severity. Analysis revealed a significant upregulation in the levels of miR-16-5p, miR-15b-5p, miR-17-5p, and miR-20a-5p in patients with no/mild injury at 0–6 h of age compared to moderate/severe injury group and controls. These miRNAs are implicated in the regulation of cell proliferation and apoptosis. Previous studies have reported that miR-16-5p and miR-15b-5p induce apoptosis by targeting the ani-apoptotic protein BCL-233,34,35. Pathway studio analyses predict that miR-15b-5p is involved in apoptosis regulation, while miR-16-5p positively regulates apoptosis (Figure S5). The overexpression of miR-15b-5p and miR-16b-5p induces cell cycle arrest in G1-G0, and their levels negatively correlate with those of cyclin D136. The dynamic injury landscape of neonatal NE and the various time points post-injury are two factors that influence the type of cell death implicated in the disease. Following acute neonatal HI injury, strikingly necrosis is the major cell death phenotype in the brain of mouse, rat, and piglet neonates37,38,39. Moreover, necrosis is associated with early neurodegeneration after HI, while apoptosis is associated with delayed neuronal death. This may explain the upregulation of apoptosis-associated miRNAs in the no/mild injury group compared to moderate/severe injury group, and the lack of difference between healthy controls and moderate/severe injury group. While, these findings should be interpreted with caution because the limited sample size and the inherent heterogeinity of NE, they provide initial evidence of the role of apoptosis as a major component of the pathophysiologic cascade in no/mild brain injury, and suggest that miR-16-5p and miR-15b-5p have potential to identify subjects most likely to respond to therapeutic hypothermia by ameloriating apoptosis40, and be used as predictive markers and for drug development in the moderate to severe injury group.
MiR-17-5p and miR-20a-5p were shown to prevent cell cycle arrest during neuronal lineage differentiation of stem cells41. miEAA predicts that they are implicated in the regulation of cell proliferation and differentiation (Figure S5). Interestingly, the overexpression of the miR-17–92 cluster upregulates cell proliferation in ischemic animals42. Branyan et al. showed that stroke outcomes were improved when miR-20a-3p was administered by intravenous injections 4 h after middle cerebral artery occlusion (MCAo) in rats43. MiR-17-5p and miR-20a-5p were upregulated in the no/mild injury group compared to controls, probably as a an attempt to mitigate the pathological effects of hypoxia. This increase is not observed in the moderate/severe injury group. Clinically, this calls for the investigation of miR-17-5p and miR-20a-5p as attractive candidates for future NE treatment. Moreover, these markers may affect synaptic plasticity and long-term outcomes and merit further study.
In this study, we have also measured miRNAs at 48 h during hypothermia to identify potential markers of treatment response, and foud that miR-197-3p, miR-342-3p, miR-328-3p, miR-191-5p, miR-103a-3p, and miR-150-5p were significantly upregulated in patients with no/mild injury compared to the moderate/severe group and controls. It was previously established that miR-150-5p promotes cell survival to protect against ischemic injury in the heart44. Additionally, the neuroprotective role of miR-150-5p was revealed in the hypoxic-ischemic brain45. Scherrer et al. reported that lower log-miR-150-5p levels in the plasma were associated with mortality three months post-ischemic stroke46. Clinically, this finding reflects the potential of miR-150-5p as an attractive marker for monitoring the therapeutic response following hypothermia.
Of the neonates with seizures (36%) in our cohort, 85% had EEG-confirmed seizures and 15% had clinical seizures. Our study demonstrated that AST, ALT, and the presence of seizures were associated with moderate/severe brain injury on MRI. Seizures have been reported to correlate with worse outcomes in neonates with NE47. These observations are not novel, but they demonstrate that our cohort is consistent with others reported in the literature47,48. Our results highlight the association between miRNA levels and the potential mechanisms of liver injury, as well as seizure activity in the injured neonatal brain.
One of the strong points of this study is the inclusion of matched healthy controls and a considerable number of neonates with NE compared to previous studies15,49,50. Moreover, we assessed miRNA profile alterations in the low cord pH group. This allowed us to identify miRNAs that can differentiate between neonates with low cord pH and those with NE, suggesting that these two conditions are associated with distinct molecular mechanisms. Furthermore, we utilized sera to allow the assessment of only extracellular miRNA. We offered a practical approach for NE diagnosis by utilizing circulating markers which are convenient and efficient.
One limitation of neonatal biomarker studies is the lack of studying only neonates with sentinel events, which occur in 15–29% of NE cases51,52. These events include placental abruptions, uterine ruptures, and shoulder dystocia accompanied by the interruption of placental function or the disruption of fetal blood flow and leading to hypoxia–ischemia in the fetus. Unlike adults with traumatic brain injury or stroke, the exact timing of injury in NE may be unknown. Sentinel events allow for the exact timing of the hypoxic-ischemic insult. We performed a sub-group analysis of all neonates with sentinel events, but the sample size was small. Additionally, we analyzed MRI results by subjective reading. Ideally, objective readings with volumetric measurement of the injury should be used to correlate injury with the serum concentrations of biomarkers. Finally, control and low cord pH samples were obtained at birth and 1 h of age respectively. While these were ideal controls for the 0–6 h of age NE group, we were unable to obtain control and low cord pH samples at 48 h of age and therefore comparisons at this time point may not be ideal.
In conclusion, this study provides pilot data that confirm the alteration of miRNA profiles of neonates with moderate to severe NE compared to healthy controls. There is limited research on miRNA in the context of NE. Our results can be utilized to focus the research efforts on each identified miRNA marker individually. Moreover, the identified miRNAs in this study have the potential for utilization as quantifiable noninvasive biomarkers for NE diagnosis and therapeutic response monitoring.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABG:
-
Arterial blood gas
- aEEG:
-
Amplitude-integrated electroencephalography
- AUC:
-
Area under the curve
- CK:
-
Creatine kinase
- CK-MB:
-
Creatine kinase-myoglobin binding
- DWI:
-
Diffusion-weighted imaging
- HIE:
-
Hypoxic-ischemic encephalopathy
- IRAK:
-
Interleukin-1 receptor-associated kinase 1
- LFT:
-
Liver function test
- MCAo:
-
Middle cerebral artery occlusion
- miEAA:
-
MiRNA Enrichment Analysis and Annotation
- miRNAs:
-
MicroRNAs
- MRI:
-
Magnetic resonance imaging
- NE:
-
Neonatal encephalopathy
- NICU:
-
Neonatal Intensive Care Unit
- OPLS-DA:
-
Orthogonal partial least squared discriminant analysis
- PCA:
-
Principal component analysis
- PTT:
-
Partial thromboplastin time
- SNEA:
-
Subnetwork Enrichment Analysis
- SST:
-
Serum separator tubes
- TBI:
-
Traumatic brain injury
- TLR4:
-
Toll-like receptor 4
References
Huntzinger, E. & Izaurralde, E. Gene silencing by microRNAs: Contributions of translational repression and mRNA decay. Nat Rev Genet. 12(2), 99–110. https://doi.org/10.1038/nrg2936 (2011).
Ipsaro, J. J. & Joshua-Tor, L. From guide to target: Molecular insights into eukaryotic RNA-interference machinery. Nat Struct Mol Biol. 22(1), 20–28. https://doi.org/10.1038/nsmb.2931 (2015).
O’Brien, J., Hayder, H., Zayed, Y. & Peng, C. Overview of MicroRNA biogenesis, mechanisms of actions, and circulation. Front Endocrinol (Lausanne). 9, 402. https://doi.org/10.3389/fendo.2018.00402 (2018).
Ponnusamy, V. & Yip, P. K. The role of microRNAs in newborn brain development and hypoxic ischaemic encephalopathy. Neuropharmacology. 149, 55–65. https://doi.org/10.1016/j.neuropharm.2018.11.041 (2019).
McIntyre, S. et al. Neonatal encephalopathy: Focus on epidemiology and underexplored aspects of etiology. Semin Fetal Neonatal Med. 26(4), 101265. https://doi.org/10.1016/j.siny.2021.101265 (2021).
Chalak, L. F. et al. Biomarkers for severity of neonatal hypoxic-ischemic encephalopathy and outcomes in newborns receiving hypothermia therapy. J Pediatr. 164(3), 468–474. https://doi.org/10.1016/j.jpeds.2013.10.067 (2014).
Graham, E. M., Everett, A. D., Delpech, J. C. & Northington, F. J. Blood biomarkers for evaluation of perinatal encephalopathy: State of the art. Curr Opin Pediatr. 30(2), 199–203. https://doi.org/10.1097/MOP.0000000000000591 (2018).
Massaro, A. N. et al. Serum biomarkers of MRI brain injury in neonatal hypoxic ischemic encephalopathy treated with whole-body hypothermia: A pilot study. Pediatr Crit Care Med. 14(3), 310–317. https://doi.org/10.1097/PCC.0b013e3182720642 (2013).
Massaro, A. N. et al. Plasma biomarkers of brain injury in neonatal hypoxic-ischemic encephalopathy. J Pediatr. 194, 67–75. https://doi.org/10.1016/j.jpeds.2017.10.060 (2018).
Murray, D. M. Biomarkers in neonatal hypoxic-ischemic encephalopathy: Review of the literature to date and future directions for research. Handb Clin Neurol. 162, 281–293. https://doi.org/10.1016/B978-0-444-64029-1.00013-8 (2019).
Douglas-Escobar, M. & Weiss, M. D. Hypoxic-ischemic encephalopathy: A review for the clinician. JAMA Pediatr. 169(4), 397–403. https://doi.org/10.1001/jamapediatrics.2014.3269 (2015).
Douglas-Escobar, M. V. et al. UCH-L1 and GFAP serum levels in neonates with hypoxic-ischemic encephalopathy: A single center pilot study. Front Neurol. 5, 273. https://doi.org/10.3389/fneur.2014.00273 (2014).
Looney, A. M. et al. Altered expression of umbilical cord blood levels of miR-181b and its downstream target mUCH-L1 in infants with moderate and severe neonatal hypoxic-ischaemic encephalopathy. Mol Neurobiol. https://doi.org/10.1007/s12035-018-1321-4 (2018).
Looney, A. M. et al. Downregulation of umbilical cord blood levels of miR-374a in neonatal hypoxic ischemic encephalopathy. J Pediatr. 167(2), 269–273. https://doi.org/10.1016/j.jpeds.2015.04.060 (2015).
O’Sullivan, M. P. et al. Validation of altered umbilical cord blood MicroRNA expression in neonatal hypoxic-ischemic encephalopathy. JAMA Neurol. 76(3), 333–341. https://doi.org/10.1001/jamaneurol.2018.4182 (2019).
Whitehead, C. L. et al. Circulating MicroRNAs in maternal blood as potential biomarkers for fetal hypoxia in-utero. PLoS One. 8(11), e78487. https://doi.org/10.1371/journal.pone.0078487 (2013).
Wang, Z., Liu, Y., Shao, M., Wang, D. & Zhang, Y. Combined prediction of miR-210 and miR-374a for severity and prognosis of hypoxic-ischemic encephalopathy. Brain Behav. 8(1), e00835. https://doi.org/10.1002/brb3.835 (2018).
Chang, L. L. et al. Enteral feeding as an adjunct to hypothermia in neonates with hypoxic-ischemic encephalopathy. Neonatology. 113(4), 347–352. https://doi.org/10.1159/000487848 (2018).
Shankaran, S. et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med. 353(15), 1574–1584 (2005).
Harris, P. A. et al. Research electronic data capture (REDCap): A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 42(2), 377–381. https://doi.org/10.1016/j.jbi.2008.08.010 (2009).
Barkovich, A. J. et al. Prediction of neuromotor outcome in perinatal asphyxia: evaluation of MR scoring systems. AJNR Am J Neuroradiol. 19(1), 143–149 (1998).
Backryd, E., Ghafouri, B., Carlsson, A. K., Olausson, P. & Gerdle, B. Multivariate proteomic analysis of the cerebrospinal fluid of patients with peripheral neuropathic pain and healthy controls: A hypothesis-generating pilot study. J Pain Res. 8, 321–333. https://doi.org/10.2147/JPR.S82970 (2015).
Olausson, P. et al. Protein alterations in women with chronic widespread pain: An explorative proteomic study of the trapezius muscle. Sci Rep. 5, 11894. https://doi.org/10.1038/srep11894 (2015).
Wheelock, A. M. & Wheelock, C. E. Trials and tribulations of ’omics data analysis: Assessing quality of SIMCA-based multivariate models using examples from pulmonary medicine. Mol Biosyst. 9(11), 2589–2596. https://doi.org/10.1039/c3mb70194h (2013).
Eriksson, L. B. T., Johansson, E., Trygg, J., VikstroÈm, C. Multi- and Megavariate Data Analysis: Basic Principles and Applications. 3rd ed. MKS Umetrics 2013.
Casey, S. et al. Temporally altered miRNA expression in a piglet model of hypoxic ischemic brain injury. Mol Neurobiol. 57(10), 4322–4344. https://doi.org/10.1007/s12035-020-02018-w (2020).
Li, C. et al. Microglia-derived exosomal microRNA-151-3p enhances functional healing after spinal cord injury by attenuating neuronal apoptosis via regulating the p53/p21/CDK1 signaling pathway. Front Cell Dev Biol. 9, 783017. https://doi.org/10.3389/fcell.2021.783017 (2021).
Taganov, K. D., Boldin, M. P., Chang, K. J. & Baltimore, D. NF-kappaB-dependent induction of microRNA miR-146, an inhibitor targeted to signaling proteins of innate immune responses. Proc Natl Acad Sci USA. 103(33), 12481–12486. https://doi.org/10.1073/pnas.0605298103 (2006).
Gaulee, P. et al. Concentration of serum biomarkers of brain injury in neonates with a low cord pH with or without mild hypoxic-ischemic encephalopathy. Front Neurol. 13, 934755. https://doi.org/10.3389/fneur.2022.934755 (2022).
Kao, Y. C., Wang, I. F. & Tsai, K. J. miRNA-34c Overexpression causes dendritic loss and memory decline. Int J Mol Sci. https://doi.org/10.3390/ijms19082323 (2018).
Hu, J., Hu, X. & Kan, T. MiR-34c participates in diabetic corneal neuropathy via regulation of autophagy. Invest Ophthalmol Vis Sci. 60(1), 16–25. https://doi.org/10.1167/iovs.18-24968 (2019).
Greco, S. et al. Deregulated microRNAs in myotonic dystrophy type 2. PLoS One. 7(6), e39732. https://doi.org/10.1371/journal.pone.0039732 (2012).
Cimmino, A. et al. miR-15 and miR-16 induce apoptosis by targeting BCL2. Proc Natl Acad Sci USA. 102(39), 13944–13949. https://doi.org/10.1073/pnas.0506654102 (2005).
Jiang, X. et al. Aloe-emodin induces breast tumor cell apoptosis through upregulation of miR-15a/miR-16-1 that suppresses BCL2. Evid Based Complement Alternat Med. 2020, 5108298. https://doi.org/10.1155/2020/5108298 (2020).
Chatterjee, A., Chattopadhyay, D. & Chakrabarti, G. MiR-16 targets Bcl-2 in paclitaxel-resistant lung cancer cells and overexpression of miR-16 along with miR-17 causes unprecedented sensitivity by simultaneously modulating autophagy and apoptosis. Cell Signal. 27(2), 189–203. https://doi.org/10.1016/j.cellsig.2014.11.023 (2015).
Bandi, N. et al. miR-15a and miR-16 are implicated in cell cycle regulation in a Rb-dependent manner and are frequently deleted or down-regulated in non-small cell lung cancer. Cancer Res. 69(13), 5553–5559. https://doi.org/10.1158/0008-5472.CAN-08-4277 (2009).
Northington, F. J. et al. Necrostatin decreases oxidative damage, inflammation, and injury after neonatal HI. J Cereb Blood Flow Metab. 31(1), 178–189. https://doi.org/10.1038/jcbfm.2010.72 (2011).
Northington, F. J., Ferriero, D. M., Graham, E. M., Traystman, R. J. & Martin, L. J. Early neurodegeneration after hypoxia-ischemia in neonatal rat is necrosis while delayed neuronal death is apoptosis. Neurobiol Dis. 8(2), 207–219 (2001).
Martin, L. J. et al. Neuronal death in newborn striatum after hypoxia-ischemia is necrosis and evolves with oxidative stress. Neurobiol Dis. 7(3), 169–191. https://doi.org/10.1006/nbdi.2000.0282 (2000).
Edwards, A. D. et al. Specific inhibition of apoptosis after cerebral hypoxia-ischaemia by moderate post-insult hypothermia. Biochem Biophys Res Commun. 217(3), 1193–1199. https://doi.org/10.1006/bbrc.1995.2895 (1995).
Trompeter, H. I. et al. MicroRNAs MiR-17, MiR-20a, and MiR-106b act in concert to modulate E2F activity on cell cycle arrest during neuronal lineage differentiation of USSC. PLoS One. 6(1), e16138. https://doi.org/10.1371/journal.pone.0016138 (2011).
Liu, X. S. et al. MicroRNA-17-92 cluster mediates the proliferation and survival of neural progenitor cells after stroke. J Biol Chem. 288(18), 12478–12488. https://doi.org/10.1074/jbc.M112.449025 (2013).
Branyan, T. E. et al. Functional assessment of stroke-induced regulation of miR-20a-3p and its role as a neuroprotectant. Transl Stroke Res. 13(3), 432–448. https://doi.org/10.1007/s12975-021-00945-x (2022).
Tang, Y. et al. MicroRNA-150 protects the mouse heart from ischaemic injury by regulating cell death. Cardiovasc Res. 106(3), 387–397. https://doi.org/10.1093/cvr/cvv121 (2015).
Luo, H. et al. miR-150-3p enhances neuroprotective effects of neural stem cell exosomes after hypoxic-ischemic brain injury by targeting CASP2. Neurosci Lett. 779, 136635. https://doi.org/10.1016/j.neulet.2022.136635 (2022).
Scherrer, N. et al. MicroRNA 150-5p improves risk classification for mortality within 90 days after acute ischemic stroke. J Stroke. 19(3), 323–332. https://doi.org/10.5853/jos.2017.00423 (2017).
Srinivasakumar, P. et al. Treating EEG seizures in hypoxic ischemic encephalopathy: A randomized controlled trial. Pediatrics. 136(5), e1302–e1309. https://doi.org/10.1542/peds.2014-3777 (2015).
Elsadek, A. E., FathyBarseem, N., Suliman, H. A., et al. Hepatic injury in neonates with perinatal asphyxia. Glob Pediatr Health. 2021;8:2333794X20987781. https://doi.org/10.1177/2333794X20987781
Winkler, I. et al. MicroRNA expression profiles as diagnostic and prognostic biomarkers of perinatal asphyxia and hypoxic-ischaemic encephalopathy. Neonatology. 119(2), 204–213. https://doi.org/10.1159/000521356 (2022).
Dong, X. et al. Expression profile of circular RNAs in the peripheral blood of neonates with hypoxic-ischemic encephalopathy. Mol Med Rep. 22(1), 87–96. https://doi.org/10.3892/mmr.2020.11091 (2020).
Badawi, N. et al. Intrapartum risk factors for newborn encephalopathy: The Western Australian case-control study. BMJ. 317(7172), 1554–1558. https://doi.org/10.1136/bmj.317.7172.1554 (1998).
Nelson, K. B. et al. Antecedents of neonatal encephalopathy in the Vermont Oxford Network Encephalopathy Registry. Pediatrics. 130(5), 878–886. https://doi.org/10.1542/peds.2012-0714 (2012).
Acknowledgements
We thank all families for participating in clinical research, which allows us to continue to improve care for neonates.
Author information
Authors and Affiliations
Contributions
Supervision: MW and KW; Study Design: MW and LS; Data Collection; ZY, HX, LS, CR, MA, DR; Data analysis, SM, FD, FK, SL, and MW; Experiments: ZY, HX and CR; Writing: FD, FK, SM, LS and MW, Reviewing and editing: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dakroub, F., Kobeissy, F., Mondello, S. et al. MicroRNAs as biomarkers of brain injury in neonatal encephalopathy: an observational cohort study. Sci Rep 14, 6645 (2024). https://doi.org/10.1038/s41598-024-57166-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-57166-z
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.