Burden of disease by major depressive disorder
Depressive disorders generally consist of major depressive disorder, dysthymia and minor depression, but not other conditions that include depressive features, such as bipolar disorder. Major depressive disorder is the most serious clinical entity in the depressive spectrum and it is one of the most commonly diagnosed psychiatric illnesses. Major depressive disorder represents a priority for potential preventive interventions, because it is highly prevalent and it represents a serious recurrent condition associated with lower quality of life, elevated costs of medical treatments, a huge burden of personal and familial suffering, frequent co-morbidities, increased risk of suicide and elevated overall mortality. The yearly prevalence of major depression in adults is at least 5 %. The lifetime prevalence is 13 % with higher rates among females than males( Reference Kessler, Chiu and Demler 1 , Reference Hasin, Goodwin and Stinson 2 ). Symptoms of depression include low mood, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, feelings of tiredness, poor concentration and suicidality ideation. According to the Diagnostic and Statistic Manual of Mental Disorders, 5th edition (DSM-5), released in May 2013, the diagnostic criteria for major depressive disorder are those shown in Table 1. According to Matters and Loncar, unipolar depressive disorders were ranked the fourth global cause of disability-adjusted life years lost in 2002 and they were projected to become the second leading cause of disability-adjusted life years lost in 2030 in the world, and its first cause in high-income countries( Reference Mathers and Loncar 3 ). Consequently, depressive disorders pose heavy health and economic burdens and thus their prevention is a global public health priority.
Table 1. Diagnostic criteria for depression
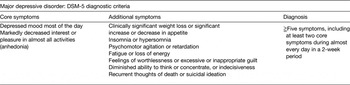
DSM-5, Diagnostic and Statistic Manual of Mental Disorders, 5th edition.
Age-adjusted rates of depression and suicide are known to be lower in Southern Europe (Spain, Italy and Greece) than in Northern or Central European countries( Reference Chishti, Stone and Corcoran 4 ). This South-to-North gradient has been hypothetically related to the diversity of food patterns between Mediterranean and non-Mediterranean countries. This difference also indirectly suggests that some aspects of the traditional Mediterranean diet (MeDiet) might have contributed to lower the risk of depression.
Aetiological hypothesis of depression
Major depressive disorder is considered to be a multifactorial disease. Therefore, a wide array of potential causes including biological, psychological and environmental factors are likely to be involved in the aetiology of depression. The interaction among these elements needs also to be taken into account( Reference Belmaker and Agam 5 ). Alterations in multiple neurobiological pathways, and not a single mechanism, are probably responsible for clinical cases of depression. Recent advances in neuroimaging procedures, including functional neuroimaging studies, have allowed a better understanding of some of these mechanisms.
Well-defined clinical and laboratory evidence supports a hormonal role in depression. This hypothesis holds that repeated or maintained stress-induced hypercortisolaemia will eventually lead to down-regulation of glucocorticoid receptors in the central nervous system. The normal negative feedback on cortisol consisting of inhibition of corticotropin-releasing hormone and adrenocorticotrophic hormone as a response to high cortisol levels will be eventually reversed in depression. As a consequence, an alteration of the hypothalamic–pituitary–adrenal axis is frequently seen in depressed patients with positive instead of negative feedback. This creates a vicious cycle with cortisol levels permanently elevated. The consequence of this vicious circle is that the levels of cortisol, adrenocorticotrophic hormone and corticotropin-releasing hormone are often simultaneously elevated in the depressed patients. This vicious circle has also been supposedly implicated in reduced volume of the hippocampus, reduced rates of neurogenesis, accumulation of visceral fat, abdominal obesity and a higher propensity to insulin resistance. This mechanism is compatible with the coexistence of major depression and a higher cardiovascular risk related to abdominal obesity, low-grade inflammatory status and insulin resistance. In this context it seems logical to think that depression and cardiovascular risk are very likely to share similar risk factors and aetiological mechanisms.
Another widely accepted aetiological theory is the monoamine hypothesis of depression. It suggests that depression is related to a dysfunction in serotoninergic or noradrenergic systems in the central nervous system. The crucial step is reduced availability of these monoamines in the synapse. The ability of some antidepressants to increase monoamine availability in the synapse by blocking their catabolism (for example, monoamine oxidase inhibitors) of by inhibiting their reuptake by the presynaptic neuron (for example, serotonin-reuptake inhibitors) are strong bases for this hypothesis( Reference Belmaker and Agam 5 ). Also, a test of oral tryptophan depletion (the subject is given a drink containing all amino acids except tryptophan, and therefore body stores of tryptophan are depleted) will not cause depression in healthy subjects, but will cause a relapse of some previously depressed subjects because tryptophan is the rate-limiting substrate for serotonin synthesis in the brain. In this context, an adequate intake of vitamin B6, folate, and vitamin B12 can be speculated to be associated with lower depression risk, because they are involved in the metabolism of S-adenosyl methionine and methionine (an essential amino acid). These latter two compounds are critical to the production of monoamines (serotonin and noradrenaline) and methylation in the brain. An interesting hypothesis of depression suggests that deficiencies in vitamin B6, folate and vitamin B12 can lead to reduced synthesis of these monoamines and decreased availability of them in the synapse. The repeatedly reported association between elevated levels of homocysteine and depression seems to corroborate this hypothesis because suboptimal levels of folate and B vitamins are associated with higher homocysteine levels and higher homocysteine levels have been associated with depression( Reference Almeida, McCaul and Hankey 6 ). A food pattern that ensures an optimal nutritional adequacy of these micronutrients (B vitamins and folate) would be likely to exert a preventive action on depression.
Food patterns as a component cause of sufficient causal pathways leading to depression
According to the classical model of causation in epidemiology proposed by Kenneth Rothman( Reference Rothman, Greenland and Lash 7 ), the occurrence of a specific disease will always have several contributing determinants that may act together in conjunction to produce the disease outcome of interest. There are several sufficient causes or causal pathways, each of them composed of several elements. The Rothman's model defined sufficient causes as complete causal mechanisms that will inevitably produce the disease. These complete causal mechanisms or ‘sufficient’ causes will never be isolated or single factors. On the contrary, each of them needs to include a set of different elements and circumstances that, once all of them are present, will unavoidably determine the production of the disease. This is the reason why the Rothman's model is sometimes called a modified deterministic causal model.
In contrast to sufficient causes, Rothman defined a component cause as each of the many elements that are included in at least one of the sufficient causal mechanisms or pathways. Usually, epidemiologists consider component causes as actual and proper causes of disease because the disease will not occur by that sufficient causal mechanism or pathway unless all the component causes of that pathway are present. Speaking in positive terms, if only one of its component causes is removed, that causal pathway will not produce the disease. This is a powerful approach for preventive medicine because, under the assumptions of this model, it is not necessary to tackle all of the component causes which are included in a sufficient cause or pathway in order to prevent the disease. Only with the elimination of one of them, the disease will be prevented.
In the context of the Rothman's model of causation in epidemiology, there is a growing body of evidence to support that some unhealthy food patterns can be considered as component causes of depression. Indeed, this assertion does not imply that unhealthy food patterns will be always a cause of depression (they are not a sufficient cause) neither that in all cases of depression an unhealthy food pattern was involved in the causal pathway (they are not a necessary cause of depression). Food patterns merely represent one of several component causes present in at least one of the multiple sufficient causes (causal pathways) of depression. Nevertheless, they can be appropriately referred to as causes of depression.
Biological plausibility for the link between cardioprotective diets and reduced risk of depression
One important criterion for causality in epidemiology is biological plausibility. There are many reasons to support the biological plausibility that cardioprotective food patterns are also protective against major depression( Reference Sanchez-Villegas and Martínez-González 8 ). Reasons to support this biological plausibility include the following mechanisms exerted by a cardioprotective diet: Anti-inflammatory effects; A high content of antioxidants, which can produce neuroprotection; Improved insulin sensitivity and reduced risk of metabolic syndrome; Improved endothelial function being the endothelium responsible for neurotrophins synthesis, including brain-derived neurotrophic factor; Potential for enhanced synaptogenesis and neurogenesis as a consequence of better availability and function of neurotrophins; Better nutritional adequacy and availability of B vitamins and folate related to the synthesis of monoamines; Improvement of lipid subtypes (n-3 fatty acids and other unsaturated fatty acids instead of trans fatty acids or SFA) in cell membranes, and consequently increased fluidity and permeability of cell membranes, where receptors for neurotransmitters are located; Counteracting of the adverse metabolic effects and increased visceral fat due to the abnormal regulation of the hypothalamic–pituitary–adrenocortical axis that occurs in depression.
In this context, a wide body of clinical and epidemiological evidence supports a strong mutual link between depression and CVD. Sometimes the occurrence of depression precedes a cardiovascular event; in other instances a cardiovascular event is associated with a future higher risk of depression. It is very likely that depression and CVD may share common pathophysiological factors. For example, the seven health cardiovascular metrics proposed by the American Heart Association in 2010( Reference Lloyd-Jones, Hong and Labarthe 9 ) were predictive of a substantially lower risk of depression in 5110 participants of the Aerobics Study cohort followed-up for 6·1 years( Reference España-Romero, Artero and Lee 10 ). Also in the Seguimiento Universidad de Navarra (SUN) cohort, after following-up more than 16 000 participants initially free of depression and CVD during an average of 9 years, several predictive equations for cardiovascular risk built with baseline values of cardiovascular risk factors were strongly associated with the future risk of developing depression during the follow-up period (P Molero, unpublished results).
Advantages of food patterns in nutritional epidemiology
Several nutrients or foods have been associated with the risk of depression in longitudinal epidemiologic studies. They include a reduced risk of depression associated with an increased intake of folate( Reference Gilbody, Lightfoot and Sheldon 11 , Reference Astorg, Couthouis and de Courcy 12 ), n-3 fatty acids and n-3:n-6 fatty acids ratio( Reference Beydoun, Fanelli Kuczmarski and Beydoun 13 – Reference Sanchez-Villegas, Henríquez and Figueiras 15 ), olive oil( Reference Kyrozis, Psaltopoulou and Stathopoulos 16 , Reference Sánchez-Villegas, Verberne and De Irala 17 ) or moderate alcohol intake( Reference Gea, Martinez-Gonzalez and Toledo 18 , Reference Gea, Beunza and Estruch 19 ), whereas an increased risk of depression has been associated with higher intake of trans fatty acids( Reference Sánchez-Villegas, Verberne and De Irala 17 ), fast food and commercial bakery( Reference Sánchez-Villegas, Toledo and de Irala 20 ).
However, in nutritional epidemiology, two different situations need to be differentiated. Sometimes, the disease of interest is likely to be caused by a single nutrient or food. In contrast, and much more frequently, the disease will be probably associated with several dietary factors. For the first (and rare) situation the focus on a single nutrient or food may be adequate. However, for the most common situations of multifactorial dietary causes of a disease, the focus on a single nutrient or food will be wrong. In these very common situations, the food pattern approach represents the best-fitted methodology according to the current state of the art in nutrition research. The reason is that to assess the overall food pattern may be more useful because it goes beyond nutrients or foods and examines the effects of the overall diet. The focus on isolated nutrients or single foods is usually inappropriate because it would be unrealistic to assume that a single food or nutrient will have an important effect. In addition, the assessment of isolated food components makes it difficult to take into account any interaction between them. Food patterns allow capturing a wide range of potential interactions between different nutrients and foods. Moreover, the assessment of isolated foods or nutrients will be frequently confounded by other dietary factors.
The analysis of food patterns instead of isolated foods or nutrients overcomes most of the earlier-mentioned problems. Conversely, from an epidemiologic point of view, the sociological reality that many foods are usually consumed together provides an interesting approach per se. Therefore, in the study of the relationships between nutritional factors and the risk of depression, to change the focus to overall food patterns is more useful than the reductionist view of attributing all the effect to a single food or nutrient( Reference Hu 21 ). The advantages and limitations of the use of food patterns in nutritional epidemiology are presented in Table 2.
Table 2. Strengths and limitations of the food pattern approach

Food patterns cannot be directly measurable. However, they have been defined as the quantities, proportions, variety or combinations of different foods and beverages in diets, and the frequency with which they are habitually consumed( Reference Martínez-González and Martín-Calvo 22 , 23 ).
The methodology to ascertain food patterns can follow four different general approaches: (i) Selective diets: The procedure involves classifying subjects according to whether or not they meet several criteria (e.g. avoidance of meat or meat products to classify them as vegetarians); (ii) Indexes or scores: They are built according to individuals’ scores on quality of the food pattern and its components. They are sometimes referred to as a priori food patterns (e.g. the Mediterranean Dietary Score (MDS) proposed by Trichopoulou et al.)( Reference Trichopoulou, Martínez-González and Tong 24 ); (iii) Cluster Analysis: Statistical analysis conducted to build groups of similar individuals according to their food patterns. These are examples of a posteriori or empirically derived food patterns; (iv) Factor Analysis: Statistical identification of factors explaining variation in individuals’ scores (e.g. the Western Food Pattern originally proposed by Hu et al.)( Reference Hu, Rimm and Stampfer 25 ). As the previous analysis, this approach identifies a posteriori or empirically derived food patterns.
The second approach represented by a dietary index tries to assess overall diet quality. The use of a dietary index is considered as an a priori approach because the scoring systems for such indexes or scores are based on previous knowledge of what constitutes a healthy diet or what represents a traditional or geographical model for a typical combination of food habits (e.g. a Mediterranean-type diet). Sometimes, the dietary index/score approach might be limited by the gaps in current knowledge and current understanding of the food–disease relationship. Further examples, beyond the MeDiet, of some a priori-defined food patterns using indices or scores are the Healthy Eating Index (HEI), a single summary measure of the degree of conformity between an individual's diet and the recommendations of the US Department of Agriculture Food Guide Pyramid for five major food groups and to specific recommendations in the US Dietary Guidelines for Americans, the Healthy Diet Score, the Recommended Food Score or the Alternative HEI.
Available longitudinal evidence on food patterns and the risk of depression
Some studies have pointed out that several food patterns could be associated with the risk of depression among adults. This association seems to be consistent across countries, cultures and populations according to several systematic reviews and meta-analyses( Reference Quirk, Williams and O'Neil 26 – Reference Rahe, Unrath and Berger 28 ). These systematic reviews included not only adults but also other populations, included retrospective or cross-sectional studies without longitudinal data and finally, occasionally included studies that really did not assess the effect of an overall food pattern, but only of food items or food groups. Table 3 provides a summary of available longitudinal prospective studies assessing the risk of adult depression associated with overall food patterns.
Table 3. Available longitudinal studies assessing the risk of depression associated with overall food patterns
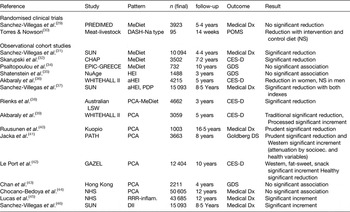
PREDIMED, PREvención con DIeta MEDiterránea (prevention with Mediterranean diet); MeDiet, Mediterranean diet; Dx, diagnosis; DASH, dietary approaches to stop hypertension; POMS, Profile of Mood States; SUN, Seguimiento Universidad de Navarra; CHAP, Chicago Health and Aging Project; EPIC, European Prospective Investigation into Cancer and Nutrition; GDS, Geriatric Depression Scale; NuAge, Québec Longitudinal Study on Nutrition and Aging; HEI, healthy eating index; aHEI, alternative healthy eating index; CES-D, Center for Epidemiologic Studies Depression Scale; PDP, pro-vegetarian dietary pattern; Australian LSW, Australian Longitudinal Study on Women's Health; PCA, principal component analysis; PATH, personality and total health; Goldberg DS, Goldberg Depression Scale; GAZEL, GAZ and ELectricité; NHS, Nurses’ Health Study; RRR-Inflam, reduced rank regression to ascertain a pro-inflammatory dietary pattern; DII, Dietary Inflammatory Index.
Only one large randomised trial (the PREDIMED study) has tested the effects on the risk of incident cases of clinical depression during 5·4-years follow-up of two MeDiet in comparison with a control group receiving advice to follow a low-fat diet in an elderly population at high cardiovascular risk( Reference Sánchez-Villegas, Martínez-González and Estruch 29 ). The point estimates for the relative risks (RR) associated with the intervention using a MeDiet supplemented with extra-virgin olive oil (RR = 0·91) or a MeDiet supplemented with mixed tree nuts (RR = 0·78) in the PREDIMED trial suggested an inverse association. However, the CI for both estimates were wide and they showed that the results were compatible with a null result. Even when both MeDiet were merged together and analysed as a single group, the multivariable-adjusted RR was 0·85 (95 % CI 0·64, 1·13). Only when the analysis was limited to participants with type 2 diabetes (approximately 50 % of the sample), a significantly reduced risk of depression was observed and only for participants assigned to the MeDiet + nuts (RR = 0·59; 95 % CI 0·36, 0·98; P = 0·04) but not for participants randomly allocated to MeDiet + extra-virgin olive oil. A second available trial of a small sample size and short duration tested a diet in line with the model of the Dietary Approaches to Stop Hypertension trial and moderately reduced in sodium( Reference Torres and Nowson 30 ). The outcome was the amelioration of symptoms of postmenopausal depression. A beneficial effect was observed for both the active intervention and the control group, without significant differences between them.
Among observational studies, an inverse association between a priori defined Mediterranean-type diets and the incidence of depression has been found in two large cohorts( Reference Sánchez-Villegas, Delgado-Rodríguez and Alonso 31 , Reference Skarupski, Tangney and Li 32 ). In the largest of them (the SUN study) a reduced risk of depression associated with closer conformity to the traditional MeDiet was found( Reference Sánchez-Villegas, Delgado-Rodríguez and Alonso 31 ). The conformity to the MeDiet was operationally defined using the MDS proposed by Trichopoulou et al.Reference Trichopoulou, Costacou and Bamia 33 The MDS assigned 1 point to subjects whose consumption was at or above the sex-specific median of six components in agreement with the traditional MeDiet (vegetables, fruits/nuts, legumes, fish/seafood, cereals and MUFA:SFA lipid ratio). The participant received also 1 point if her/his intake was below the median for the two components not in line with the traditional MeDiet (meat/meat products and dairy products). For ethanol, 1 point was assigned only for moderate amounts of intake (5–25 g/d for women or 10–50 g/d for men). Consequently, the MDS could theoretically range from the highest possible conformity to MeDiet (9 points) to the minimum possible conformity (0 points reflecting no adherence at all). Adherence to the MDS was categorised into five categories: low (score 0–2), low–moderate (score 3), moderate–high (score 4), high (score 5) and very high (6–9). The RR of incident clinical depression (480 new diagnoses during 4·4-years follow-up) were 0·74, 0·66, 0·49 and 0·58 for low-moderate, moderate-high, high and very high conformity v. low conformity, respectively, all of them statistically significant in fully adjusted models and with a significant linear trend (P = 0·002). To allay fears related to a potential reverse causality bias (i.e. depressed patients may have poorer dietary habits as a consequence of their depression), the authors repeated their analyses after excluding those cases of depression reported in the first 2 years of follow-up (n 243). Contrarily to the hypothesis of reverse causation that would predict an attenuation of the association after the exclusion of early cases, the inverse associations for the two upper categories of conformity to the MeDiet were not attenuated, but they even exhibited stronger inverse associations with RR = 0·42 (95% CI 0·27, 0·66) and R = 0·50 (95% CI 0·33, 0·74) for MDS = 5 and MDS ≧ 6, respectively.
Nevertheless, it should be pointed out that a smaller cohort study in Greece, did not find any significant advantage of the MeDiet( Reference Psaltopoulou, Kyrozis and Stathopoulos 34 ). However, it is necessary to highlight that the present study was based on a sample of only 732 elders. The point estimate for the RR associated with the MeDiet was protective although not significant probably due to a lack of statistical power.
The association between the adherence to other quality dietary indexes beyond the MeDiet and depression has also been analysed. Whereas no significant effect between the adherence to the HEI and changes in depressive symptoms was found after 3 years of follow-up in the NuAge study( Reference Shatenstein, Ferland and Belleville 35 ), Akbaraly et al. showed a significant association between a higher score in the alternative HEI and a lower risk of depression in women, but not in men, from the Whitehall-II cohort study( Reference Akbaraly, Sabia and Shipley 36 ). Also in the SUN cohort, several other quality dietary indexes, specifically the alternative HEI and the Pro-vegetarian Dietary Pattern showed an inverse association with the incidence of depression and suggested the potential existence of a nonlinear threshold effect( Reference Sánchez-Villegas, Henríquez-Sánchez and Ruíz-Canela 37 ). This last finding suggests that the risk of depression can be reduced when a subject moves from very low to moderate adherence to a diet quality index. However, there is not much extra benefit in terms of reduced risk of depression for further improvements in adherence when the subject moves from moderate to high or very high scores. This dose–response pattern is compatible with the hypothesis that suboptimal intake of some micronutrients (present in the lower levels of adherence to diet quality scores) is involved in the risk of developing depression.
Principal component analysis (Factor Analysis approach) has also been developed in several cohort studies to identify post-hoc (empirically derived) food patterns( Reference Rienks, Dobson and Mishra 38 – Reference Chocano-Bedoya, O'Reilly and Lucas 44 ). Results obtained for MeDiet are consistent with those reported using a priori-defined food pattern( Reference Rienks, Dobson and Mishra 38 ). Other examples include the results reported by Akbaraly et al. within the Whitehall-II study( Reference Akbaraly, Brunner and Ferrie 39 ) that found that an empirically derived food pattern rich in sugary desserts, fried foods, processed meats, refined grains and high-fat dairy products was associated with a significantly increased risk of depression, whereas an empirically derived food pattern rich in vegetables, fruits and fish was associated with a significantly lower risk of depression. In contrast with the significant protection against depression found for a Prudent food pattern empirically identified in the Kuopio cohort( Reference Ruusunen, Lehto and Mursu 40 ) or in the Australian PATH cohort study( Reference Jacka, Cherbuin and Anstey 41 ) or the detrimental role of Western, snacking and fat-sweet food patterns obtained in the GAZEL cohort study( Reference Le Port, Gueguen and Kesse-Guyot 42 ), other studies have failed to report statistically significant results for the analysis of the association between a posteriori food patterns and depression( Reference Chan, Chan and Woo 43 ). In this sense, it is remarkable to highlight the results reported in the Nurses’ Health Study. In this large cohort, the Prudent (high in vegetables) or Western (high in meats) food patterns also identified by using principal component analysis did not show any significant association with the incidence of depression( Reference Chocano-Bedoya, O'Reilly and Lucas 44 ). However, another posterior assessment in the Nurses’ Health Study using reduced rank regression methods found that a pro-inflammatory food pattern was significantly associated with a higher risk of depression( Reference Lucas, Chocano-Bedoya and Schulze 45 ) supporting the hypothesis of the biological plausibility for the link between cardioprotective diets and reduced risk of depression mentioned earlier.
In line with these findings, the SUN cohort has also recently reported a similar magnitude of the increment in the risk of depression related to a pro-inflammatory food pattern assessed through the Dietary Inflammatory Index, a scoring algorithm based on an extensive review of the literature linking articles focusing on the effect of diet on inflammatory biomarkers( Reference Sánchez-Villegas, Ruíz-Canela and de la Fuente-Arrillaga 46 ).
Though further longitudinal studies and trials are needed to confirm several aspects such as the link between depression and cardiometabolic conditions or the shape of the dose–response curve between adherence to a diet quality index and the risk of depression, we can conclude stating that there is a growing body of sound epidemiological evidence to support that food patterns with a high content in fruit and vegetables, olive oil, tree nuts, fish and whole grains, but low in meats, meat products, commercial bakery, trans fats, sugary desserts and sugar-sweetened beverages are associated with a reduced risk of depression.
Acknowledgements
We are indebted to the participants of the SUN Project for their continued cooperation and participation. We thank the other members of the SUN Group: Alonso A, Barrio López MT, Basterra-Gortari FJ, Benito Corchón S, Bes-Rastrollo M, Beunza JJ, Carlos Chillerón S, Carmona L, Cervantes S, de Irala Estévez J, de la Fuente Arrillaga C, de la Rosa PA, Delgado Rodríguez M, Donat Vargas CL, Donázar M, Fernández Montero A, Galbete Ciáurriz C, García López M, Gea Sánchez A, Goñi Ochandorena E, Guillén Grima F, Hernández A, Lahortiga F, Llorca J, López del Burgo C, Marí Sanchís A, Martí del Moral A, Martín Calvo N, Martínez JA, Núñez-Córdoba JM, Pimenta AM, Ruíz-Canela M, Ruíz Zambrana A, Sánchez Adán D, Sayón Orea C, Toledo Atucha E, Toledo Atucha J, Vázquez Ruiz Z and Zazpe García I.
Financial Support
The SUN Project was supported by the official funding agency for biomedical research of the Spanish government, Instituto de Salud Carlos III (ISCIII), through grants provided to research networks (RTIC RD 06/0045, to M. A. M.-G.) and through Centro de Investigación Biomédica en Red de Fisiopatología de la Obesidad y Nutrición (CIBERobn) and by grants from Fondo de Investigación Sanitaria–Fondo Europeo de Desarrollo Regional (Proyecto de Investigación (PI) 10/02658, 10/02293 and 13/00615).
Conflicts of Interest
None.
Authorship
Both the authors contributed equally to the writing of this work.








