Poor diet, high blood pressure (BP) and low levels of physical fitness in childhood have been associated with multiple health problems including overweight and obesity, CVD, cancer and type 2 diabetes mellitus(1, Reference Weiss, Dziura and Burgert2). Furthermore, overweight and obesity are now the most common childhood disorders in Europe(3), causing social, psychological and physiological health problems in childhood and poor health outcomes as an adult(Reference Waters, de Silva-Sanigorski and Burford4). Environmental and lifestyle factors are recognised as the primary drivers of obesity, with poor diet and sedentary behaviours playing a role(Reference Perry, Garside and Morones5). Both national(Reference Bel-Serrat, Heinen and Murrin6) and international statistics(7) show that obese children are more likely to become obese adults, indicating that surveillance and the promotion of healthy behaviours early in life are warranted(Reference Craigie, Lake and Kelly8).
The school environment has the potential to make important differences in children’s health and presents a number of opportunities for intervention(Reference Vasques, Magalhaes and Cortinhas9–Reference Ward, Saunders and Pate12). In fact, school-based interventions show consistent improvements in children’s knowledge and attitudes, behaviour and, when tested, physical and clinical outcomes(1). Primary schools are particularly favourable, as children of primary school age can be highly influenced by health promotion initiatives, which can then promote positive behavioural changes that can continue into adulthood(13). Children also spend considerable amounts of time at school and this setting enables large numbers of children to be targeted at one time(Reference Garrow14).
Research from a systematic review of thirty-two studies with over 52 000 participants(Reference Sobol-Goldberg, Rabinowitz and Gross15) reported that recent school-based interventions demonstrate more convincing evidence for improvements in BMI by enhancing dietary intake (DI) and increasing physical activity (PA) than earlier initiatives. Another systematic review(Reference Waters, de Silva-Sanigorski and Burford4) also found strong evidence to support the beneficial effects of school-based programmes targeted to children aged 6–12 years. Such programmes include increased PA, improvements in nutritional quality of school food and providing environments and cultural practices to support healthy eating and activity throughout each day(Reference Waters, de Silva-Sanigorski and Burford4). Parental support is also important, which includes encouraging children to be more active, eat more nutritious foods and spend less time in screen-based activities in the home(Reference Horne, Hardman and Lowe16). Although some studies involving either a PA or a healthy eating component have shown positive effects on adiposity outcomes, combined nutrition and PA interventions seem to be more successful in improving multiple health behaviours (not just adiposity reduction) in primary-school children(Reference Amini, Djazayery and Majdzadeh17, Reference Wang, Cai and Wu18). A combined approach may also help to prevent the co-morbidities associated with obesity(Reference Bryan, Nilsson and Tompkins19), encouraging children to establish long-lasting healthy lifestyle habits. In addition, long-term interventions (>12 months) appear to be more effective in achieving healthier BMI(Reference Mei, Xiong and Xie20, Reference Sobol-Goldberg, Rabinowitz and Gross15) and improving diet and PA(Reference Wan Putri, Hamid Jan and Hafzan21), compared with short-term interventions (<12 months).
To date, there are no health promotion programmes targeting both nutrition and PA in Irish primary schools that have been evaluated and proven effective. Definite conclusions as to the effectiveness of such programmes at improving health behaviours and preventing overweight and/or obesity are therefore not available. Without such interventions, unhealthy behaviours are at risk of continuing, which could have both immediate and long-term health implications. To address this, Project Spraoi (http://www.cit.ie/projectspraoi), a primary-school health promotion intervention that aims to promote PA, improve DI and increase nutritional knowledge (NK) of Irish schoolchildren, was created. ‘Spraoi’ is a Gaelic Irish word, which means ‘fun’. Project Spraoi is based on Project Energize (www.projectenergize.org.nz/); a combined PA and nutrition intervention that is effective at improving cardiorespiratory fitness (CRF), body composition, BP and nutrition for children(Reference Rush, McLennan and Obolonkin22). The project, which has been running in New Zealand for 10 years, has proven to be both sustainable and cost-effective(Reference Rush, Cairncross and Williams23). With only minor changes to the Project Energize resources to make them suitable to an Irish setting (minor changes to some of the foods/drinks used in the resources and adaptation of games), Project Spraoi aims to achieve similar health improvements in schoolchildren in Cork.
Methodology
Participation
Two schools were selected via convenience sampling for the purpose of a larger study, Project Spraoi, as described in detail elsewhere(Reference Coppinger, Lacey and ONeill24). Inclusion criteria for schools included: mixed, middle/high socio-economic status, rural, medium sized(25), proximity of 20 km to the research institute, willingness to implement the Project Spraoi intervention and not currently participating in another PA and/or healthy eating intervention(Reference Coppinger, Lacey and ONeill24). The intervention and control schools were matched on the inclusion criteria listed above. Due to budgetary constraints of the project, there was one ‘energizer’/researcher assigned to delivering the intervention to all classes (n 10). Hence, due to the exploratory nature of the study and limited resources, two schools were screened prior to the intervention to ensure they were not undertaking any other PA or healthy eating programmes. With more resources the number of schools would have been increased. However, the impact of the intervention may have been compromised as energizing time would have been greatly reduced if more than two schools were included with the current resources.
All students from the intervention school (n 274) received the PA and nutrition intervention; children in the control school (n 567) did not receive any of the intervention components. While all children from the intervention school took part in the nutrition and PA classes, evaluation of DI, NK, BP, anthropometric and CRF measurements was carried out only on 6-year-old and 10-year-old children. A total of 101 children (forty-nine 6-year-olds, fifty-two 10-year-olds; 48·1 % boys, 51·9 % girls) participated. The mean age for 6-year-olds was 6·09 (sd 0·33) years and 9·9 (sd 0·37) years for 10-year-olds. These two age groups were chosen as these age ranges are important for forming and understanding health habits(Reference Coppinger, Lacey and ONeill24). Data were collected over four days (two weekdays and two weekend days) at two time points (baseline, October 2014 and post-intervention, June 2016) by trained postgraduate researchers and staff of Cork Institute of Technology (Cork, Ireland). The same children were assessed at baseline and post-intervention; non-response rate for completed food diaries increased from 25 % (n 25) at baseline to 32 % (n 32) post-intervention.
Informed assent and parental consent were required from all children before participation. Ethical approval was obtained from Cork Institute of Technology Research Ethics Review Board in September 2013. All data collected were kept strictly confidential and were accessible only to researchers involved in Project Spraoi at Cork Institute of Technology. All participants were assigned a random identification number at the beginning of the study by the lead researcher, who was the only person able to trace data back to any participant. This identification number was used for the duration of the study. Data were collected on paper and inputted on to a password-protected laptop that was accessible only by the lead researcher. Data were processed and will be stored in line with the General Data Protection Regulation (GDPR) (EU) 2016/679.
Project Spraoi intervention
The Project Spraoi intervention took place over two academic years from October 2014 to May 2016. Every class (n 10) in the school received one ‘energizer’ session per week and this continued over the entire two-year period. For the purpose of evaluation, measurements were taken from participants at baseline (prior to the intervention delivery) and post-intervention data were gathered two years later, directly after completion of the intervention. The relevant intervention material used in Project Energize was tailored for use in Project Spraoi, with minor adjustments applied, in order to make it relevant to the Irish setting. From the outset, an agreement was signed by the school and the ‘energizer’ (who provided hands-on support and assistance to schools and teachers), agreeing to the goals of Project Spraoi and to outline expectations, roles and responsibilities. The researcher also acted as the ‘energizer’ for the entire intervention. The ‘energizer’ and class teacher discussed plans for targeted nutrition and PA classes, which included providing specific material on healthier food choices, delivering simple healthy food demonstrations and modelling PA classes based on Kiwidex(26) and Project Energize(Reference Rush, Reed and McLennan27). Information was also provided on unhealthy foods and ways to encourage a reduction in the amount of high-energy/low-nutrient foods consumed. Parents were given the opportunity to attend information and demonstration sessions, delivered by the ‘energizer’. These included healthy lunchbox ideas, tasting sessions and education sessions on high-sugar beverages and takeaways. The PA classes included the delivery of 20 min of huff and puff games, circuit classes, dance routines, gymnastics and whole-school initiatives. The key objectives of the Project Spraoi nutrition and PA interventions are described in Table 1.
Table 1 Key aims of the Project Spraoi nutrition and physical activity intervention
Dietary analysis
A 4 d estimated food diary (two weekdays and two weekend days), adapted from the Cork Children’s Lifestyle Study (CCLaS)(Reference Keane, Kearney and Perry28), was used to examine DI. Written instructions were provided to participants and parents and the researcher also provided guidance in the classroom setting on completing the food diary (students only). Each day of the food diary was broken into six meal sections: breakfast, morning snack, lunch, afternoon snack, dinner and evening snack. Ten-year-old children were advised to seek help from parents and teachers when filling in their food diary, while parents of 6-year-old children were asked to complete the food diary with them. To improve dietary data completion, the researcher sat down with all 10-year-olds at the end of food diary collection to fill in any missing information. While the researcher did not meet individually with parents, contact details of the researcher were made available to parents should they have any questions about the food diaries or data collection. To encourage accurate recording of portion sizes, detailed images from the Young Person’s Food Atlas (primary)(Reference Foster, Hawkins and Adamson29) were included with the diary to encourage the accurate recording of portion sizes. The Irish Food Portion Sizes Database(Reference Lyons and Giltinan30) was used to assign an age-appropriate median portion size when no estimation was given. Number of unhealthy snacks (sweets, crisps, chocolate, ice cream, cakes, biscuits, bars and pastries) was estimated using the Irish Food Portion Sizes Database(Reference Lyons and Giltinan30).
All foods and beverages were entered into the Dietplan 7 (Forestfield Software Ltd, Horsham, UK, 2015) software package. The statistical software package IBM SPSS Statistics for Windows version 22 was used to analyse and examine fruit and vegetable intake (total number of servings per day); number of unhealthy snacks per day; fibre (g/d); macronutrient intake, i.e. protein (% total energy), fat (% total energy), saturated fat (% total energy), sugar (% total energy); and micronutrient intake, i.e. Na (mg/d), Ca (mg/d) and Fe (mg/d).
Identifying under-reporters
To estimate total daily energy requirements, each participant’s BMR (based on his/her age, sex and weight according to Schofield et al.(Reference Schofield, Schofield and James31)) was multiplied by an allocated physical activity level (PAL)(Reference Torun, Davies and Livingstone32). The minimum PAL cut-off values were applied (PAL = 1·28 males and females aged 1–5 years, PAL = 1·39 for males aged 6–18 years and PAL = 1·30 for females aged 6–18 years). Each child’s total energy intake was then compared with his/her estimated energy requirements and it was found that 54·5 % of children were classified as under-reporters. To consider the likelihood of misreporting, all macronutrients in the present study were expressed as a proportion of energy consumed(25).
Nutrition knowledge questionnaire
The validated ‘Fit Kids ‘r’ Healthy Kids’(Reference Gower, Laurie and Moyer-Mileur33) questionnaire was used to assess participants’ knowledge of healthy eating. To ensure its age appropriateness and relevance in an Irish setting, it was first piloted in a primary school in Cork (among twenty-three students). Minor changes were made to the pictures and the Irish Food Pyramid (2012)(34) replaced the US Department of Agriculture food pyramid(35) used in the original questionnaire(Reference Gower, Laurie and Moyer-Mileur33). A total of fifteen multiple-choice questions measured knowledge of food groups, healthful foods and food functions.
Anthropometric and blood pressure measurements
All anthropometric measurements were carried out by trained researchers in a private room, in small groups (six children). The same researcher, where possible, undertook the same physical measurement with each child pre- and post-intervention to minimise intra-reliability error(Reference Coppinger, Lacey and ONeill24). Height (cm), body mass (kg) and waist circumference (cm) measurements were taken prior to (October 2014) and at the end of (June 2016) intervention delivery. Height and body mass were measured to calculate BMI and BMI Z-scores(Reference Cole, Freeman and Preece36, Reference Cole and Lobstein37). The International Obesity Task Force(Reference Cole and Lobstein37) age- and gender -adjusted cut-off points were applied to the data in order to assign BMI classifications (thin, normal, overweight, obese) and to make international comparisons. Waist-to-height-ratio (WHtR) was also calculated by dividing waist circumference by height and the universal cut-off value for children of 0·5 indicated risk of obesity and cardiometabolic syndrome(Reference Ashwell38). WHtR has been shown to be a better predictor for the presence of CVD risk factors than BMI in children(Reference Ribeiro, Coutinho and Bramorski39, Reference Savva, Tornaritis and Savva40). Waist circumference was measured in duplicate using a non-stretch Seca 200 measuring tape, height was measured using Leicester portable height scales and weight was measured using Tanita WB100MZ portable electronic scales. BP (mmHg) was measured on the right arm in a seated position, with the cuff positioned 2 cm above the elbow. Children were required to sit quietly prior to measurement to ensure an accurate reading. A third measurement was taken if the difference was >10 mmHg. Children were classified into BP categories (normal and high-normal/high) according to gender- and age-specific BP cut-off points(Reference Jackson, Thalange and Cole41).
Cardiorespiratory fitness
CRF was measured using a validated 550 m walk/run test(Reference Albon, Hamlin and Ross42, Reference Hamlin, Fraser and Lizamore43). An oval loop using a 110 m rope was set up on a level grassed area outside. The run/walk test was first explained before all children participated in a warm-up lap. Participants, in groups of up to five, were asked to complete five laps as quickly as possible. Time taken to complete the 550 m for each participant was recorded, in minutes and seconds, using calibrated XLR8 stopwatches. Run scores were classified into fast (≤50th centile) or slow (>50th centile) categories, based on the Waikato 2011 centile charts for time to complete 550 m(Reference Rush and Obolonkin44).
Data analysis
Data were analysed using IBM SPSS Statistics for Windows version 22.0. Mean and sd were used to summarise the data for all continuous variables. Children absent from school on the day of testing were recorded as missing values. Children were divided into four subgroups according to age and gender: 6-year-old boys, 6-year-old girls, 10-year-old boys and 10-year-old girls. Shapiro Wilk test and Levene’s test were used as criteria for satisfying the assumptions of measurements being normally distributed and homogeneity of variance, respectively. A repeated-measures ANOVA was undertaken to investigate statistically significant differences in DI, NK, height, weight, BMI, WHtR, BP and CRF between the intervention and control groups. All statistical testing was performed using a 5 % level of significance. The effect size (ES), η², was calculated to determine the strength of any statistically significant findings (small: 0·01 ≤ η² < 0·06; medium: 0·06 ≤ η² < 0·14; large: η² ≥ 0·14).
Results
Repeated-measures ANOVA was implemented to compare results of anthropometric measurements, BP, run time, NK (shown in Tables 2 and 3) and DI (shown in Tables 4 and 5) at baseline and post-intervention. Statistically significant interaction effects for the intervention were found. There were statistically insignificant differences between genders for anthropometric measurements, BP, run time and NK. Hence, results are reported for the total sample in Tables 2 and 3. There was no significant difference in energy intake for 6-year-olds and 10-year-olds from baseline to post-intervention.
Table 2 Effects of the Project Spraoi two-year nutrition and physical activity intervention for 6-year-old Irish schoolchildren: anthropometric, blood pressure (BP) measurements, run time and nutritional knowledge (repeated-measures ANOVA; n 49)
Table 3 Effects of the Project Spraoi two-year nutrition and physical activity intervention for 10-year-old Irish schoolchildren: anthropometric, blood pressure (BP) measurements, run time and nutritional knowledge (repeated-measures ANOVA; n 52)

* A large effect size.
† A medium effect size.
Table 4 Effects of the Project Spraoi two-year nutrition and physical activity intervention for 6-year-old Irish schoolchildren: macro- and micronutrient intakes, fruit and vegetable intake, and number of unhealthy snacks (repeated-measures ANOVA; n 49)
* A large effect size.
Table 5 Effects of the Project Spraoi two-year nutrition and physical activity intervention for 10-year-old Irish schoolchildren: macro- and micronutrient intakes, fruit and vegetable intake, and number of unhealthy snacks (repeated-measures ANOVA; n 52)
* A large effect size.
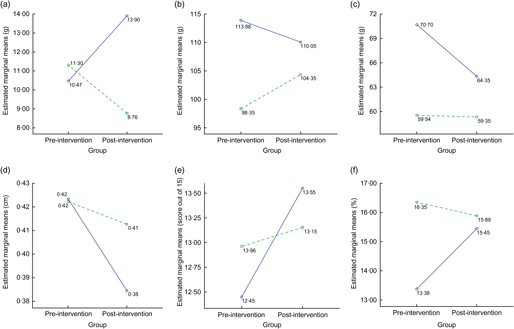
Intervention effects: 6-year-olds
There was only one significant finding for the 6-year-olds: a large statistically significant difference of 5·97 g between the change in fibre intake in 6-year-old males in the intervention and control groups (P = 0·024, ES = 0·315; Table 4). Fibre intake increased by 3·43 g within the intervention group and decreased by 2·54 g in the control group, see Fig. 1(a). Analysis of baseline data revealed that 69·4 % of 6-year-old children had normal BP, 18·4 % had high-normal and 12·2 % had high BP.
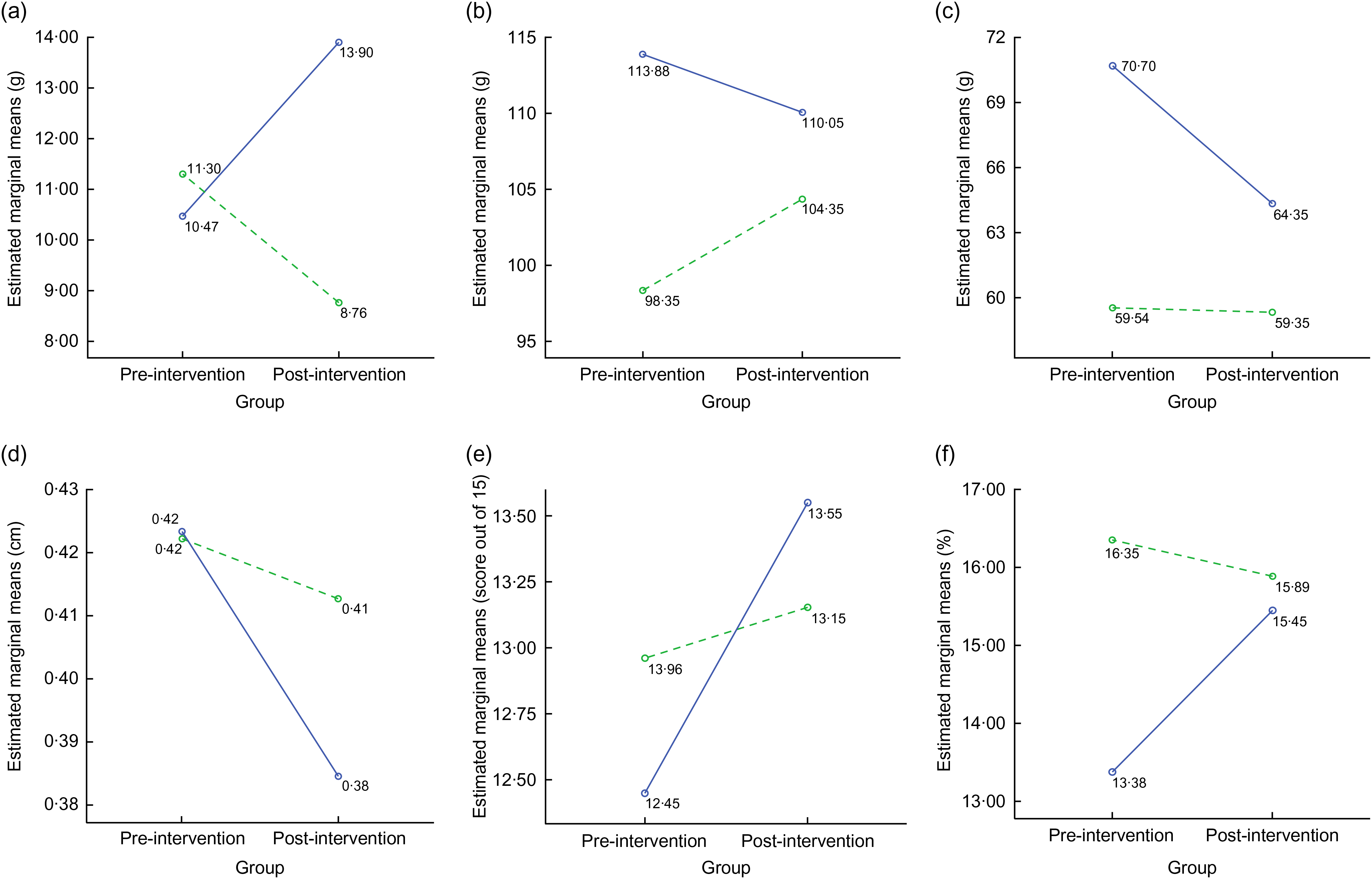
Fig. 1 Statistically significant effects of the Project Spraoi two-year nutrition and physical activity intervention for Irish schoolchildren: (a) fibre intake, 6-year-old males; (b) systolic blood pressure, 10-year-olds; (c) diastolic blood pressure, 10-year-olds; (d) waist-to-height ratio, 10-year-olds; (e) nutritional knowledge, 10-year-olds; (f) protein intake as a percentage of energy, 10-year-old females. ![]() , intervention group;
, intervention group; ![]() , control group
, control group
Intervention effects: 10-year-olds
For 10-year-olds, there was a large statistically significant difference of 9·83 mmHg between the change in systolic BP in the intervention and control groups (P = 0·005, ES = 0·165). Analysis of baseline data revealed that 56·9 % of 10-year-olds had normal BP, 27·5 % had high-normal and 15·7 % had high BP. The systolic BP decreased by 3·83 mmHg within the intervention group and increased by 6·0 mmHg in the control group, see Fig. 1(b). There was a moderate significant difference of 6·16 mmHg between the change in diastolic BP in the intervention and control groups (P = 0·023, ES = 0·116). The diastolic BP decreased by 6·35 mmHg for 10-year-olds in the intervention group and decreased by 0·19 mmHg in the control group, see Fig. 1(c).
There was a large statistically significant difference of 0·01 between the change in WHtR in the intervention and control groups (P = 0·0005, ES = 0·386). WHtR decreased by 0·02 in the intervention group compared with the control group, which decreased by 0·01, see Fig. 1(d). There was a moderate statistically significant difference of 0·91 (6·07 %) between the change in NK in the intervention and control groups (P = 0·027, ES = 0·107). NK of the intervention group improved by 1·1, while the control group only increased their NK by 0·19, see Fig. 1(e).
There was only one statistically significant change in DI for 10-year-olds. There was a large statistically significant difference of 2·53 % between the change in percentage of energy from protein in 10-year-old females in the intervention and control groups (P = 0·021, ES = 0·276). The percentage energy from protein increased by 2·07 % within the intervention group and decreased by 0·46 % in the control group, see Fig. 1(f).
Discussion
Project Spraoi is the only PA and nutrition intervention to date that has been implemented and evaluated among primary-school children in Ireland.
Project Spraoi significantly reduced systolic and diastolic BP in 10-year-old children. Our findings are consistent with research that school-based nutrition and PA intervention programmes can reduce BP(Reference Rush, Reed and McLennan27, Reference Hollar, Messiah and Lopez-Mitnik45) and thereby improve children’s health in the long term. Previous studies have demonstrated that a combination of increased PA and improved DI has a positive effect on BP in children when intervention duration was greater than 12 months(Reference Hollar, Messiah and Lopez-Mitnik45) and the reduction in BP was more marked in those studies in which combined diet and PA interventions were used(Reference Cai, Wu and Wilson46). Early intervention is critical as high BP is also correlated with WHtR(Reference Chen, Choy and Chan47) and BP in childhood predicts hypertension and metabolic syndrome later in life(Reference Sun, Grave and Siervogel48). The significant decrease in BP following the intervention is a clinically significant outcome as it has previously been shown in adults that every mmHg decrease in BP decreases the risk of CVD(Reference Chen, Choy and Chan47). Our results demonstrate the value of implementing a health promotion programme such as Project Spraoi in primary schools to significantly reduce systolic and diastolic BP.
Although there was no change in BMI, WHtR has been shown to be a better predictor for the presence of CVD risk factors than BMI in children(Reference Ribeiro, Coutinho and Bramorski39, Reference Savva, Tornaritis and Savva40) and higher level of fat accumulation around the abdominal area is associated with less favourable cardiometabolic profiles in children(Reference Khoury, Manlhiot and McCrindle49). Therefore, the significant improvement in WHtR for 10-year-old males and females in the intervention group is an important finding and supports the effectiveness of Project Spraoi in preventing overweight and obesity and decreasing cardiometabolic risk in children.
The significant increase in the NK of 10-year-olds is similar to previously published data in the USA(Reference Gower, Laurie and Moyer-Mileur33). Increased NK has the potential to enhance children’s DI(Reference Rosário, Araújo and Oliveira50). Research by Worsley(Reference Worsley51) asserts that NK may play a small but pivotal role in the adoption of healthier food habits. The increase in NK was evaluated using a validated questionnaire(Reference Gower, Laurie and Moyer-Mileur33) and similar to other studies(Reference De Villiers, Steyn and Draper52), despite an increase in NK, positive changes were not seen in DI. There was only one significant dietary change among these same 10-year-olds (increase in percentage of energy from protein). These results are disappointing and may be attributed to the fact that, despite their NK, primary-school children have little control over what they eat. Research conducted with children in Northern Ireland indicated that parents were major influencers in their children’s diets(Reference Walsh and Nelson53). Parents are responsible for what children eat at this age and therefore despite the efforts of the intervention, DI is dependent on food provided by parents. Parents play a critical role in developing an environment that fosters healthy eating and providing nutritious foods(Reference Lindsay, Sussner and Kim54). Birch et al. report that in order to improve primary-school children’s healthy food preferences, there must be increased exposure, availability and accessibility to healthy foods from parents(Reference Birch, Savage and Ventura55). Although Project Spraoi involved parents in some aspects of the programme (healthy lunchbox demonstrations, sugary drinks and takeaway information sessions, recipes), this involvement was limited and therefore increasing the amount of parental participation in Project Spraoi may help to further improve DI. Despite the increase in NK, it is parents who control what their children eat. Therefore, despite the efforts of the intervention, DI is dependent on foods/drinks provided by parents/guardians. It is expected that as these children age, the NK gained as part of the intervention will be called upon as they move towards nutritional independence.
Children’s NK is important and nutrition education should continue to form part of a multicomponent intervention to improve dietary behaviours(Reference Lakshman, Sharp and Ong56).
Although there was no significant increase in fruit and vegetable intake, there was a significant increase in fibre intake of 6-year-old males. Children with diets high in fibre see many health benefits, including normal gastrointestinal function, prevention and treatment of childhood obesity, lower BP and lower risk for CVD in adulthood(Reference Andersen, Øverby and Lillegaard57, Reference Threapleton, Greenwood and Evans58). Fibre comes from a variety of sources and while there was no increase in total percentage of energy from carbohydrate or fruit and vegetable intake from baseline to post-intervention, there may have been an increase in the intake of whole grains. Whole grains tend to have a high fibre content, which may help to explain the increase in fibre(Reference Kranz, Brauchla and Slavin59). However, this is only a hypothesis as whole grains were not measured as an individual component. The increase in protein intake in 10-year-old females is consistent with findings of the Nutrition Pathfinders programme for 4th grade students (aged approximately 10 years) which found that girls in the intervention group significantly increased their protein intake compared with girls in the control group; an effect not seen in boys(Reference Threapleton, Greenwood and Evans58). The specific foods responsible for the increase in fibre and protein are not known. Additional information on dietary data has been reported elsewhere(Reference Merrotsy, McCarthy, Flack, Lacey and Coppinger60); however, baseline data highlighted suboptimal intakes of fruit and vegetables, fibre, Ca and Fe, while unhealthy snacks and saturated fat intakes were higher than recommended. As the family food environment still has an important influence on a 6-year-old’s DI(Reference Campbell, Crawford and Ball61), it may be that a longer implementation of the intervention may be needed before changes are seen in the younger age children involved in this intervention.
Strengths and limitations
A key strength of this research is the public health implications of the findings. Project Spraoi supports primary schools to implement nutrition and PA policies which promote healthy eating and encourage children to be active, which is line with the Obesity Policy and Action Plan(62) which focuses on a ‘whole-school’ approach to tackling obesity. As dietary habits can track into adulthood, promoting healthy eating patterns in childhood may be a useful preventive strategy. The 4 d estimated food diary provides detailed data on dietary intake and is a key strength of the research. Furthermore, the present study is the first of its kind in primary schools in Ireland; although the intervention was only in one school, the positive findings emerging highlight the importance of creating a healthy school environment.
While the food diary has been shown to have high validity as a method of dietary assessment(Reference Ortega, Perez-Rodrigo and Lopez-Sobaler63), the method also has limitations, including error, reporting bias and being time-consuming for participants to complete. Our research relied on parents filling out the food diaries on behalf of the 6-year-olds, which may have decreased the response rate(Reference Shim, Oh and Kim64). In order to try and counteract this and increase response rate, all children with completed food diaries were entered into a draw to win a pair of sports shoes. The food dairies were self-reported, therefore some misreporting and non-reporting is likely to have occurred(Reference Poslusna, Ruprich and De Vries65). Debriefing with the researcher at the end of diary completion may have also introduced reporting bias of dietary intake(Reference Livingstone, Robson and Wallace66).
A total of 54·5 % of children were classified as under-reporters by comparing each child’s total energy intake with his/her estimated energy requirements using PAL cut-off values(Reference Torun, Davies and Livingstone32). To minimise the impact of misreporting all macronutrients in the present study were expressed as a proportion of energy consumed(Reference Coppinger, Lacey and ONeill24). The under-reporting of dietary intake is a considerable challenge in dietary assessment studies(Reference Livingstone, Robson and Wallace66). The percentage of participants who under-reported their energy intakes is high, but broad ranges from 10 to 50 % have been reported elsewhere(Reference Livingstone and Black67). Stallone et al.(Reference Stallone, Brunner and Bingham68) examined three approaches to dietary analysis and concluded that including all subjects and using energy adjustment was preferable to excluding under-reporters. While there may have been a difference in results between under- and over-reporters in the current study, it was beyond the scope of the study to assess these. However, to minimise the impact of misreporting, all macronutrients were expressed as a proportion of energy consumed. The Irish Universities Nutrition Alliance study(Reference Walton, McNulty and Nugent69) also reported energy-adjusted nutrient intakes to minimise the effects of under-reporting. Data must therefore be evaluated with caution(Reference Livingstone, Robson and Wallace66). The low sample size also made it more difficult to assess the impact of the intervention.
Another limitation of the present study was the minimal involvement of parents and this may have affected the results, as parents are responsible for providing their child with healthy food choices. Increased parental involvement in future research with Project Spraoi is crucial in changing the dietary habits of children, because research has shown significantly stronger effects in studies with a high level of parental involvement(Reference Charlebois, Gowrinathan and Waddell70). Regular communication with parents, special events, newsletters, information about lunchboxes and repeated opportunities for parents to be included are some of the ways to increase parental involvement(Reference Charlebois, Gowrinathan and Waddell70).
Potential confounding factors may include socio-economic status, seasonality and physical activity levels; however, we tried to limit the impact of these factors by matching the schools on socio-economic status and rural/urban. Seasonality may be an issue as baseline testing was carried out in October 2014 (autumn), while follow-up testing was undertaken in May/June (aummer). While it was beyond the scope of the study, investigating the effect of seasonality on DI, PA and CRF is recommended in future research. However, both the control and intervention data were collected at the same time so if seasonality is a factor, it is expected that it would affect both groups similarly.
Conclusion
Although only in one intervention school, the evaluation of the effectiveness of Project Spraoi has shown enhancements to WHtR, BP, NK, and healthier intakes of protein and fibre of participating children. This combined nutrition and PA intervention supports research that schools play a key role in implementing health promotion strategies to improve the overall health of children. Furthermore, it is in line with Ireland’s Obesity Policy and Action Plan(62) of supporting primary schools to implement health promotion initiatives that promote healthly eating and encourage children to be active. Improvements shown in the current study signify Project Spraoi’s potential for long-term benefits and indicate that the expansion of the intervention to other schools is both justified and warranted.
Acknowledgements
Acknowledgements: The authors would sincerely like to thank the schools and participants for their involvement in and contribution to this study. Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: None. Authorship: T.C., A.L.M., J.F. and A.M. designed the research project. A.M. conducted the research and T.C. and J.F. assisted with data collection. A.M. analysed the data and performed the statistical analysis under the guidance of S.L. A.M. was the lead author, however all authors contributed to the writing of the article. All authors then reviewed the final article for content. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Cork Institute of Technology Research Ethics Review Board. Written informed consent was obtained from all subjects.
Author ORCID
Tara Coppinger, 0000-0002-7251-4516.