Abstract
Striatal enlargement has been consistently reported in schizophrenics receiving chronic neuroleptic treatment although the results following atypical antipsychotic treatment have been equivocal. In order to disentangle patient illness from a possible drug effect on brain structure, young adult rats were administered either haloperidol, risperidone, clozapine, olanzapine, or vehicle daily for four or eight months via drinking water. Significant increases in caudate-putamen volumes were seen in animals receiving either haloperidol or clozapine when compared with control animals following eight months of drug administration. Conversely, olanzapine-treated animals showed significant decreases in caudate-putamen volumes when compared with control animals after eight months of drug. Thus, converging evidence indicates that the neuroplastic response of the striatum following neuroleptic exposure causes volumetric increases, whereas atypical antipsychotics affect the basal ganglia differentially. The current data suggests that such differential responses may be due to both the pharmacological properties and the relative doses of the atypical agents.
Similar content being viewed by others
Main
In the last three decades, there has been a notable elucidation concerning the structure, organization and function of the basal ganglia, as well as the clinical relevance of this subcortical structure. The basal ganglia are comprised of four major structures: the striatum (made up of the caudate nucleus, the putamen, and the ventral striatum), the globus pallidus, the substantia nigra, and the subthalamic nucleus. The striatum receives inputs from the neocortex and the substantia nigra and, via the globus pallidus and substantia nigra, modulates thalamic function that, in turn, affects the frontal cortex. Although the role of the basal ganglia in movement planning and execution has been recognized for many years, we now understand that the compartmentalization and diverse chemoarchitecture of the basal ganglia, combined with complex anatomical interrelationships with thalamus and cortex, establishes this structure as a prime component in influencing executive function, emotion, and cognitive behaviors including learning and memory (Alexander et al. 1990). These findings also help explain why lesions of the basal ganglia lead to devastating movement disorders such as Parkinson's and Huntington's disease. Furthermore, due to both the complexity and functional parameters of this structure, the basal ganglia may play an important role in a number of neuropsychiatric disorders such as schizophrenia (Albin et al. 1989).
Sensitive structural and functional brain imaging techniques have begun to unravel some of the complicated neuropathology present in schizophrenia. Several structural abnormalities appear to be integral to the disease process itself, including the enlargement of the lateral and third ventricles (Shenton et al. 1997; McCarley et al. 1999) as well as volumetric reductions in temporal cortex (Suddath et al. 1989; Rossi et al. 1990; DeLisi et al. 1991), hippocampus (Bogerts et al. 1985, 1990; Suddath et al. 1990), superior temporal gyrus (Barta et al. 1990; Shenton et al. 1992) and thalamus (Andreasen et al. 1994). Other anatomic abnormalities in schizophrenia, however, appear to develop secondarily to the disease process. Postmortem studies and early in vivo imaging studies have reported volumetric increases of the caudate-putamen complex in schizophrenic patients (Heckers et al. 1991; Jernigan et al. 1991). Although initially believed to be a result of a pathological neurodevelopmental process affecting the basal ganglia (Swayze et al. 1992), these structural abnormalities now appear to be probable treatment effects. In a study examining first-episode, treatment-naıuml;ve schizophrenia patients, Chakos et al. (1994) demonstrated that the volume of the caudate nucleus increased after an 18-month exposure to typical antipsychotic drugs in direct proportion to the extent of treatment, findings later confirmed by Keshavan et al. (1994). In addition, Doraiswamy et al. (1995) reported that volumetric increases of the striatum are also found in major depressive patients treated with typical antipsychotic agents. Taken together, these findings strongly suggest that structural volumetric increases of the striatum are a consequence of typical antipsychotic treatment, possibly as a result of long-term blockade of dopamine D2 receptor (Chakos et al. 1994; Keshavan et al. 1994).
Interestingly, recent studies have indicated that atypical antipsychotics may also have an effect on basal ganglia volumes, although the direction of the change is unclear. For instance, several studies have reported that caudate volumes in schizophrenic patients return to normal following replacement of typical neuroleptics with the atypical antipsychotic clozapine (Chakos et al. 1995; Frazier et al. 1996; Corson et al. 1999; Scheepers et al. 2000), although one study reported that clozapine administration increased caudate volume in patients (Staal et al. 2000). Examination of the effects of atypical agents in neuroleptic-naıuml;ve patients also have yielded inconsistent findings, with some studies reporting that clozapine either causes no change (Gur et al. 1998) or decreases caudate volume (Keshavan et al. 1998b).
Due to the complexity of disentangling patient illness from possible treatment effects, these issues are particularly amenable to study in animal models. The present set of experiments sought to determine whether long-term administration of typical or atypical antipsychotic drugs affects brain structure in rodents, as such data can shed light as to whether striatal volume changes in patients are a disease-specific manifestation of schizophrenia or a predictable consequence of drug actions. While many similarities exist between humans and the rat, there are also some differences, such as the fact that the striatum of the rat is composed of a single structure that encompasses both the caudate and putamen nuclei. Nonetheless, by using an animal model to study drugs that have different mechanisms of actions (i.e., having differing affinities for dopamine D2 receptors as well as different target receptors), insights can be gained about how such drugs affect brain structure and the adaptive mechanisms that may be involved.
MATERIALS AND METHODS
Animal Treatments
Young adult male Sprague-Dawley rats (Charles River, PQ), approximately 3.5 months old and weighing 225–250 g at the start of the study, were individually housed and maintained on a controlled 12h:12h light:dark cycle throughout the study. All animals in Experiments 1 and 2 (described below) were age-matched (± 1 week), and were randomly assigned to each drug treatment groups. Animals were allowed free access to water and Purina Laboratory Rat Chow (Purina Mills, St. Louis, MO) prior to initiation of the study. Once drug dosing began, all rats were placed on moderate caloric restriction in order to offset possible weight changes across the experimental groups that may have ultimately influenced brain volumes. The animals maintained body weights at 75% of their free-feeding weights and were allowed to gain an additional 5 g per week to account for normal growth. The dietary restriction was continued throughout the duration of the study and body weights in all drug-treatment groups did not significantly differ from the control group (data not shown). Weights were recorded weekly, with experimental drug dosage adjusted accordingly. Animal care was in accordance with guidelines set by the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
In experiment 1, there were four treatment groups: haloperidol (1.0 mg/kg/day), clozapine (20.0 mg/kg/day), risperidone (1.0 mg/kg/day), and a vehicle control. In experiment 2, initiated at a later date than experiment 1, olanzapine (3.0 mg/kg/day) was compared with vehicle. Clozapine (Novartis Pharmaceuticals, Basel, Switzerland) and olanzapine (Eli Lilly, Inc., Indianapolis, IN) were first dissolved in 1 N HCL and then titrated to pH 5.7 with 1 N NaOH. Additional 0.9% saline was added to achieve a final drug concentration of 1.4%. Haloperidol (McNeil Pharmaceuticals, Spring House, PA) and risperidone (Janssen Pharmaceutica, Inc., Beerse, Belgium), supplied in concentrate form at 5 and 10 mg/ml, respectively, were diluted in normal saline and the pH adjusted to 5.7. To enhance the taste of all drug solutions, 0.5% sucrose was added. The drugs were given orally to the animals in their drinking water on a daily basis. Water + drug intake, recorded daily, did not significantly differ between the groups (data not shown).
Animals (n = 112) were treated for a period of four or eight months and at each endpoint, the animals were anesthetized via an intraperitoneal injection of phenobarbital (40 mg/kg) and ketamine (50 mg/kg). Prior to perfusion, the tip of the tail was clipped and 3 mL of blood was collected in sodium heparin. The blood was centrifuged for 15 min at 2500 × g at 8°C and the resulting plasma frozen. Plasma levels for all drugs were assayed by the Analytical Psychopharmacology Laboratories of the Nathan Kline Institute (Orangeburg, NY). Plasma levels of haloperidol were determined using a modified gas-liquid chromatographic method that quantifies haloperidol and a major metabolite, reduced haloperidol (Bianchetti and Morselli 1978). Plasma risperidone and its major metabolite, 9-hydroxyrisperidone, (LeMoing et al. 1993) and plasma levels of clozapine and its inactive metabolite, norclozapine (Simpson and Cooper 1978), were measured using high-performance gas chromatography with electrochemical detection. Plasma olanzapine was assayed using a high performance liquid chromotography approach as reported by Catlow et al. (1995).
Immediately following the blood collection, the animals were perfused through the left ventricle of the heart with 0.9% saline, followed by fixative containing 2% paraformaldehyde in 0.1 M phosphate buffer (pH 7.4). Each brain was dissected from the cranium and stored overnight in fresh fixative at 4°C. Following postfixation, the brains were cryoprotected first in 15% and then 30% sucrose in PBS. The brains were stored in 30% sucrose for a maximum of three days for all animals, with the exception of both the 8-month groups in Experiment 2, which were stored in 30% sucrose for six weeks. Following cryoprotection, the brains were frozen in Tissue-Tek and stored at −70°C. Serial coronal sections (20 μM) were collected from the rostral to caudal poles of the striatum and stored at −70°C. The mounted sections were air-dried, briefly post-fixed with alcoholic formalin, stained with solochrome, dehydrated in graded alcohol solutions, stained with eosin, once again dehydrated in graded alcohol solutions, cleared in xylene and cover-slipped in Permount.
Although all treatment groups initially had n = 12 animals (the exception being the vehicle control groups in Experiment 2; n = 5), unequal n values occurred across the groups. This was due to animal deaths that veterinary examination suggested were unrelated to drug treatment and the occasional loss of tissue due to unavoidable perfusion and sectioning artifacts. Final n values are indicated in Table 1.
Volumetric and Morphometric Analyses
All volumetric quantifications were performed with an Olympus BH2 photomicroscope equipped with a high-resolution Sony video-camera, a motorized XYZ axis computer-controlled stage, and StereoInvestigator, a morphometry and stereology software package (MicroBrightField, Inc., Colchester, Vermont). When calculating the volume of caudate-putamen, the boundaries were defined and the volume was determined with the StereoInvestigator software according to the Cavalieri principle (Regeur and Pakkenberg 1989). Strict morphological criteria were used consistently in all animals to determine the boundaries of the caudate-putamen, with the region of interest corresponding to Plate 10 through Plate 23 of the Paxinos Rat Brain Atlas (Paxinos and Watson 1998). Briefly, the superior boundary of the striatum was defined by the corpus callosum, the lateral boundary by the external capsule, and the medial boundary by the lateral ventricle and the corpus callosum. The inferior boundary of the striatum lies between gray matter structures, and was delineated by a line drawn from the corpus callosum at the level of the rhinal fissure, extending to the lower boundary of the lateral ventricle, excluding the nucleus accumbens (Figure 1). Starting with one of the four most anterior sections, selected on a random basis across brains, every twelfth section through the rostrocaudal extent of the caudate-putamen was analyzed. By using this sampling strategy, approximately ten histological sections per brain were analyzed. The Gundersen estimated coefficient of error ranged from 0.03–0.05. All morphometric quantification was conducted blind by a trained technician unaware of treatment group, and we obtained good test-retest reliability (R2 = 0.92), calculated at the end of a lengthy set of training sessions.
Light microscope photographs of representative 20-μm coronal sections of the rat brain, stained with solochrome and eosin. The boundaries of the caudate-putamen nucleus used for the volumetric measurements are outlined in blue. A, the most anterior section, corresponds to approximately to Plate 10 of the Paxinos Atlas, while B corresponds to plate 14, and C, the most posterior section, corresponds to plate 23 (Paxinos and Watson 1998).
Statistical Analysis
As noted earlier, Experiments 1 and 2 were performed separately, indicating likely cohort differences. Thus, we felt it was inappropriate to use a 5 (vehicle, haloperidol, risperidone, clozapine, olanzapine) × 2 (four and eight months) fixed effects factorial ANOVA. Conversely, to analyze the experiments separately would reduce the error degrees of freedom, thus leading to less statistical power. Therefore, we chose to fit the twelve cells (eight from Experiment 1 and four from Experiment 2) into a one-cell means model. In order to satisfy the assumptions of this model, the observations in each cell had to be independent of one another and the cell variances had to be approximately equal. Using contrasts, we tested the main effects for drug, time, and interaction separately for Experiment 1 and Experiment 2. These tests, in the context of the larger cell, allowed for a more precise estimate of the mean square error, with a greater number of degrees of freedom, thus leading to more powerful tests. All effects were fixed effects. An experiment effect was also tested in order to assess whether it might have been possible to simply combine the data into one experiment. All statistical analyses were performed using the SAS system (SAS Inc., Cary, NC).
RESULTS
Table 2 lists the mean plasma levels for all drugs administered in the study and their corresponding therapeutic levels in humans. All animals, with the exception of those treated with clozapine, had drug blood plasma levels that were comparable to the therapeutic concentrations for the treatment of schizophrenia in humans. Mean plasma levels for norclozapine, a major inactive metabolite of clozapine, were 37.8 ng/ml at the eight month time point (data not shown), possibly indicating a high level of metabolic turnover for clozapine in the rat.
The treatment effects of vehicle, haloperidol, risperidone, and clozapine in Experiment 1 for both time points are shown in Table 1. The R2 for the model was 0.68, indicating that the model accounted for nearly 70% of the variation in caudate-putamen volume, suggesting a substantial effect of drug and time. The overall model F11,100 of 19.49 (p < .0001) indicated that experiment, treatment, and time influenced caudate-putamen volume. The experiment effect was smaller, but still highly significant (F1,100 = 8.44, p < .0045). Although the partial R2 was 0.0269, demonstrating that time of experiment initiation accounted for less than 3% of the variation in caudate-putamen volume; the most conservative approach is to discuss the main effects and interactions separately for Experiments 1 and 2.
In Experiment 1, the drug effect (F3,100 = 5.73, p < .0012) and time effect (F1,100 = 139.13, p < .0001) were highly significant, showing that both drug and duration of administration affected volumes. The interaction between the two was non-significant, allowing interpretation of the main effects and contrasts within the main effects. We tested three one-degree of freedom contrasts within the drug effect: Haloperidol X vehicle, clozapine X vehicle and risperidone X vehicle. At four months, we demonstrated a significant difference only between haloperidol and vehicle (F1,100 = 4.35, p < .039), with significantly larger caudate-putamen volumes in the haloperidol-treated animals (Table 1). At eight months, we found significant differences between haloperidol and vehicle (F1,100 = 6.50, p < .0123) and between clozapine and vehicle (F1,100 = 6.03, p < .0158), but not between risperidone and vehicle (F1,100 = 0.40, p < .5309). Figure 2 illustrates that striatal volumes in animals treated with haloperidol or clozapine are significantly larger than striatal volumes in vehicle-treated animals at eight months. The two contrasts remained significant at the 0.05 α level following a Bonferroni correction that was applied because three non-orthogonal hypotheses had been tested.
Data illustrating the effects of different classes of antipsychotic drugs on caudate-putamen volume in animals receiving vehicle (VEH), haloperidol (HAL), risperidone (RIS) or clozapine (CLZ) for eight months. Data are expressed as mean ± S.E.M. Significant increases in caudate-putamen volumes were seen in haloperidol- and clozapine-treated animals versus vehicle-control or risperidone-treated animals. (** p < .01; Bonferroni).
In Experiment 2, the drug effect (F1,100 = 5.91, p < .0168) and time effect (F1,100 = 116.79, p < .0001) were both statistically significant, showing that both drug and duration of olanzapine administration affected volumes (Table 1). The interaction effect was non-significant, enabling us to interpret both the main effects and the contrasts within. In a manner parallel to that of Experiment 1, we tested the difference between olanzapine and vehicle at four and eight months. Figure 3 indicates that there is a significant decrease in striatal volumes for animals receiving olanzapine compared with vehicle at eight months (F1,100 = 5.42, p < .0219).
Data illustrating the effects of the atypical antipsychotic agent olanzapine (OLZ) or vehicle (VEH) on caudate-putamen volumes in animals treated for eight months. Data are expressed as means ± S.E.M. Caudate-putamen volumes were significantly larger in the in the olanzapine-treated animals versus vehicle-control animals. (* p < .02; Bonferroni).
DISCUSSION
In the present study, we found that chronic administration of haloperidol significantly increases caudate-putamen volumes in rats, thereby replicating the hypertrophy seen in schizophrenic patients on neuroleptics (Heckers et al. 1991; Jernigan et al. 1991; Chakos et al. 1994; Keshavan et al. 1994; Hokama et al. 1995; DeLisi et al. 1995). Although methodological and anatomical considerations complicate direct comparisons between human and rat studies, the observed volume increases in the present study of 8% to 15% (at 4 and 8 months, respectively) approximate the 6% to 15% increases reported previously in schizophrenic patients undergoing treatment with typical antipsychotic drugs (Chakos et al. 1994; Keshavan et al. 1994). In addition, the results presented here roughly parallel those seen by Chakos et al. (1998), who examined the relationship between chronic haloperidol treatment (1.5 mg/kg/day), vacuous chewing movements and striatal volume in rats. Surprisingly, clozapine also significantly increased striatal volumes following eight months of administration, whereas olanzapine, an atypical antipsychotic agent that shares a number of similarities with clozapine, significantly decreased striatal volumes in rats when administered for a corresponding period of time. Long-term exposure to risperidone, generally considered to be an atypical agent at low doses, did not alter caudate-putamen volumes significantly at either four or eight months. Furthermore, it appears as though exposure to either clozapine or olanzapine in the rat must be fairly prolonged, as the observed volume changes seen with these drugs appeared to occur between four and eight months of administration, although it is important to note that adequate blood plasma levels were obtained with only olanzapine and risperidone, but not with clozapine. In general, studies in schizophrenic patients have also indicated that longer duration of treatment with typical antipsychotics, but not cumulative dose, is associated with greater enlargement of the caudate (Frazier et al. 1996; Keshavan et al. 1994; Lieberman et al. 2001).
It must be noted that studies that examine striatal volume changes in animals following long-term antipsychotic drug administration have not given completely consistent results, much like the human studies. Our data are in direct contrast to a rodent study by Lee et al. (1999) that reported a decrease in striatal volumes following clozapine administration, and no volume changes between animals treated with haloperidol or vehicle. Roberts (2001) recently observed no change in striatal volumes between rats treated with haloperidol or olanzapine for six months. The disparities between the animal studies may be due to a number of methodological differences, such as the use of stereological analysis, different estimations of the region of interest, and different drug dosages and duration. For example, our volumetric analysis was performed using an unbiased stereological method rather than using D1- and D2-ligand autoradiograms to determine striatal boundaries as was done by Chakos et al. (1998) and Lee et al. (1999). Likewise, aspects of the nucleus accumbens were included in the analysis by Roberts (2001) but were not included in our study.
We also found a significant effect of time in both Experiments 1 and 2, with all striatal volumes being significantly smaller at eight versus four months. This main effect of time affected all animals, including vehicle controls, indicating that caudate-putamen volumes decreased with age in this population of rats, regardless of drug treatment. This finding differs from reported human studies, in which caudate volumes in schizophrenic patients increase while those of control subjects decrease over time (Chakos et al. 1994, 1995; Keshavan et al. 1994; Corson et al. 1999) and may illustrate that the relative length of drug administration in the present animal study represents a much longer life-interval than has been studied in humans. It is unlikely that this striatal volume decrease is due to a disruption in brain maturation, as rat brain development is essentially complete by the end of the first postnatal month (Altman and Das 1966). However, the moderate dietary restriction implemented in this study cannot be ruled out as influencing the time-dependent decreases in striatal volumes. Although caloric restriction has been shown to extend life span and delay both aging and the onset of a number of life-shortening diseases in laboratory animals (Mattson et al. 2001), it is possible that caloric restriction may ultimately play a role in the striatal volume changes. For example, while Chakos et al. (1998) reported a similar increase in caudate-putamen volumes as a result of haloperidol administration, they did not see a corresponding decrease in striatal volumes over time in their rats, all of which were maintained on an ad libitum diet. Therefore, it may be advantageous to measure both caudate-putamen and total brain volumes at the initiation of future studies, and to also add an additional control arm consisting of rats fed an ad libitum diet.
Although both our present findings and those from human studies appear to demonstrate that administration of various classes of antipsychotic agents influences basal ganglial volumes in divergent ways, a number of methodological concerns (e.g., the use of thick sections with interslice gaps, the use of area measures, or varying definitions of specific regions of interest) have been suggested as contributing to the equivocal data for striatal volume changes in schizophrenic patients treated with atypical antipsychotics (Keshavan et al. 1998a). An additional factor that should be underscored is that “atypical” antipsychotic agents comprise a class of drugs that are quite different from one another with regard to both pharmacological mechanisms and behavioral effects. Customarily, antipsychotics have been classified as “atypical” because they produce significantly fewer extrapyramidal symptoms than do typical neuroleptics at clinically equivalent doses (Ichikawa and Meltzer 1999). Yet, atypical antipsychotics differ from each other, as well as from typical antipsychotics, by their occupancy of dopamine D2 or 5-HT2A receptors at therapeutic doses (Kinon and Lieberman 1996; Kasper et al. 1999; Miyamoto et al. 2000). Moreover, there are different patterns in the occupancy of other receptors and significant differences among the various atypical agents with regard to behavioral outcome measures, such as negative symptoms, cognitive dysfunction, and mood stabilization (for review, see Ichikawa and Meltzer 1999). Due to these differences, atypicality may be better viewed as a continuum, rather than categorically (Waddington and O'Callaghan 1997; Remington and Kapur 2000). This perspective suggests the importance of considering the drug (rather than the class) as a separate dependent variable in neuroimaging studies. For instance, Gur et al. (1998) examined caudate volumes of both neuroleptic-naıuml;ve and previously treated schizophrenics, half of whom were treated with risperidone, the other half with clozapine. Their conclusion that atypical antipsychotics were not associated with a change in caudate volumes may be due to opposing drug effects, since clozapine has been shown to decrease caudate volumes (Keshavan et al. 1998b) and the present study suggests that risperidone is not involved with striatal volume change.
Another important dependent variable to consider in such studies may be dose, with higher doses of atypical antipsychotics decreasing basal ganglia volumes and lower dosages increasing volumes. Studies which have shown decreases in caudate volumes following atypical antipsychotic administration include Frazier et al. (1996) and Scheepers et al. (2000) where the mean dose of clozapine was 400 and 346 mg/day, respectively, and Corson et al. (1999), who reported that the largest decrements in caudate nucleus volume occurred in four of ten patients who had received low doses of typical neuroleptics at intake and were then switched to “large doses” of clozapine (unfortunately, their medication history was reported in “dose-years”, thus making it difficult to deconvolute the data). Conversely, significantly larger caudate volumes have been observed in patients administered a mean clozapine dose of 228 mg/day (Staal et al. 2000). Differences in drug dosages may also explain the results seen in the present rat study, as the (presumably) low dosages of clozapine resulted in increased caudate volumes, while higher doses of olanzapine caused decreased caudate volumes.
It has been hypothesized that sustained blockade of neurotransmitter receptors following chronic antipsychotic treatment causes a disruption of normal homeostatic mechanisms within target neurons which may, in turn, lead to substantial and long-lasting alterations in the overall anatomic structure, as demonstrated by striatal hypertrophy. This disruption is believed to produce a number of compensatory changes, including increased striatal blood flow as well as activation, regeneration, hypertrophy and change in the number of striatal synapses (Muller and Seeman 1977; Benes et al. 1983, 1985; Meshul and Casey 1989; Meshul et al. 1994; Roberts et al. 1995). An overriding question, however, is how striatal volume changes may affect either the course of schizophrenia or the efficacy of the different antipsychotic agents. While no correlation has been established between structural abnormalities in the basal ganglia and either tardive dyskinesia or extrapyramidal symptoms (Elkashef et al. 1994; Scheepers et al. 2000), larger caudate volumes have been associated with poorer neuropsychological test performances (Hokama et al. 1995), deficit syndrome (Buchanan et al. 1993) and more severe symptomology (Gur et al. 1998), suggesting that caudate enlargement may adversely modulate the effects of the medication. Furthermore, a recent study by Scheepers et al. (2001) found that the degree of (left) caudate volume decrease was significantly correlated with improvement in positive and general symptoms, but not negitive symptoms. Conceivably, the volume decrease seen in schizophrenic patients following administration of relatively high dosages of clozapine, and perhaps olanzapine, may be indicative of a mechanism by which a critical correction occurs in the overall cortical-subcortical-thalamic circuitry, and as such, would be partially responsible for the superior efficacy of this class of antipsychotic agents with regard to cognition and possibly, negative symptoms.
In summary, a convergence of evidence from neuropathological, neuroimaging, and animal studies indicates that basal ganglia volume changes seen in schizophrenic patients are due more to antipsychotic treatment rather than the disease process itself. While the neuroplastic response of the striatum following neuroleptic exposure appears to cause volumetric increases, atypical antipsychotics appear to affect the structures of the basal ganglia differentially. The current data suggest that this differential response may be due to both the subclass of the atypical antipsychotic agent as well as the relative dose of that agent.
References
Albin RL, Young AB, Penney JB . (1989): The functional anatomy of basal ganglia disorders. Trends Neurosci 12: 366–375
Alexander GE, Crutcher MD, DeLong MR . (1990): Basal ganglia-thalamocortical circuits: parallel substrates for motor, oculomotor, ‘prefrontal’ and ‘limbic’ functions. Prog Brain Res 85: 19–146
Altman J, Das GD . (1966): Autoradiographic and histological studies of postnatal neurogenesis. I. A longitudinal investigation of the kinetics, migration and transformation of cells incorporating tritiated thymidine in neonate rats, with special reference to postnatal neurogenesis in some brain regions. J Comp Neurol 126: 337–389
Andreasen NC, Arndt S, Swayze V, Cizadlo T, Flaum M, O'Leary D, Ehrhardt JC, Yuh WT . (1994): Thalamic abnormalities in schizophrenia visualized through magnetic resonance image averaging. Science 266: 294–298
Barta PE, Pearlson GD, Powers RE, Richards SS, Tune LE . (1990): Auditory hallucinations and smaller superior temporal gyral volume in schizophrenia. Am J Psychiatry 147: 1457–1462
Benes FM, Paskevich PA, Domesick VB . (1983): Haloperidol-induced plasticity of axon terminals in rat substantia nigra. Science 221: 969–971
Benes FM, Paskevich PA, Davidson J, Domesick VB . (1985): The effects of haloperidol on synaptic patterns in the rat striatum. Brain Res 329: 265–274
Bianchetti G, Morselli PL . (1978): Rapid and sensitive method for determination of haloperidol in human samples using nitrogen-phosphorus selective detection. J Chromatog 153: 203–210
Bogerts B, Ashtari M, Degreef G, Alvir JMJ, Bilder RM, Lieberman JA . (1990): Reduced temporal limbic structure volumes on magnetic resonance images in first episode schizophrenia. Psychiatry Res: Neuroimaging 35: 1–13
Buchanan R, Breier A, Kirkpatrick B, Elkashef A, Munson R, Gellad F, Carpenter W . (1993): Structural abnormalities in deficit and nondeficit schizophrenia. Am J Psychiatry 150: 59–65
Catlow JT, Barton RD, Clemens M, Gillespie TA, Goodwin M, Swanson SP . (1995): Analysis of olanzapine in human plasma utilizing reversed-phase high-performance liquid chromatology with electrochemical detection. J Chromatogr 668: 85–90
Chakos MH, Lieberman JA, Builder RM, Borenstein M, Lerner G, Bogerts B, Wu H, Kinon B, Ashtari M . (1994): Increase in caudate nuclei volumes of first-episode schizophrenic patients taking antipsychotic drugs. Am J Psychiatry 151: 1430–1436
Chakos MH, Lieberman JA, Alvir J, Bilder R, Ashtari M . (1995): Caudate nuclei volumes in schizophrenic patients treated with typical antipsychotics or clozapine. Lancet 345: 456–457
Chakos MH, Shirakawa O, Lieberman J, Lee H, Bilder R, Tamminga C . (1998): Striatal enlargement in rats chronically treated with neuroleptic. Biol Psychiatry 44: 675–684
Corson PW, Nopoulos P, Miller DD, Arndt S, Andreasen NC . (1999): Change in basal ganglia volume over 2 years in patients with schizophrenia: typical versus atypical neuroleptics. Am J Psychiatry 156: 1200–1204
DeLisi LE, Hoff AL, Schwartz JE, Shields GW, Haltonre SN, Gupta SM, Henn IA, Anand AK . (1991): Brain morphology in first-episode schizophrenia-like psychotic patients: A quantitative magnetic resonance imaging study. Biol Psychiatry 29: 159–175
DeLisi LE, Tew W, Xie S, Hoff AL, Sakuma M, Kushner M, Lee G, Shedlack K, Smith AM, Grimson R . (1995): A prospective follow-up study of brain morphology and cognition in first-episode schizophrenic patients: preliminary findings. Biol Psychiatry 38: 349–360
Doraiswamy PM, Tupler LA, Krishnan KR . (1995): Neuroleptic treatment and caudate plasticity. Lancet 345: 734–735
Elkashef AM, Buchanan RW, Gellad F, Munson RC, Breier A . (1994): Basal ganglia pathology in schizophrenia and tardive dyskinesia: An MRI quantitative study. Am J Psychiatry 151: 752–755
Frazier JA, Giedd JN, Kaysen D, Albus K, Hamburger S, Alaghband-Rad J, Lenane MC, McKenna K, Breier A, Rapoport JL . (1996): Childhood-onset schizophrenia: brain MRI rescan after 2 years of clozapine maintenance treatment. Am J Psychiatry 153: 564–566
Gur RE, Maany V, Mozley D, Swanson C, Bilker W, Fur RC . (1998): Subcortical MRI volumes in neuroleptic-naıuml;ve and treated patients with schizophrenia. Am J Psychiatry 155: 1711–1717
Heckers S, Heinsen H, Heinsen Y, Beckmann H . (1991): Cortex, white matter, and basal ganglia in schizophrenia: A volumetric postmortem study. Biol Psychiatry 29: 556–566
Hokama H, Shenton ME, Nestor PG, Kikinis R, Levitt JJ, Metcalf D, Wible CG, O'Donnell BF, Jolesz FA, McCarley RW . (1995): Caudate, putamen, and globus pallidus volume in schizophrenia: a quantitative MRI study. Psychiatry Res Neuroimaging 61: 209–229
Ichikawa J, Meltzer HY . (1999): Relationship between dopaminergic and serotonergic neuronal activity in the frontal cortex and the action of typical and atypical antipsychotic drugs. Eur Arch Psychiatry Clin Neurosci 249: 90–98
Kasper S, Tauscher J, Kufferle B, Barnas C, Pezawas L, Quiner S . (1999): Dopamine- and serotonin-receptors in schizophrenia: results of imaging-studies and implications for pharmacotherapy in schizophrenia. Eur Arch Psychiatry Clin Neurosci 249: 83–89
Keshavan MS, Bagwell WW, Haas GL, Sweeney JA, Schooler NR, Pettegrew JW . (1994): Changes in caudate volume with neuroleptic treatment. Lancet 344: 1434
Keshavan MS, Haas G, Kahn CE, Aguilar E, Dick EL, Schooler NR, Sweeney JA, Pettegrew JW . (1998): Superior temporal gyrus and the course of early schizophrenia: progressive, static, or reversible? J Psychiatr Res 32: 161–167a
Keshavan MS, Rosenberg D, Sweeney JA, Pettegrew JW . (1998): Decreased caudate volume in neuroleptic-naıuml;ve psychotic patients. Am J Psychiatry 155: 774–778b
Kinon BJ, Lieberman JA . (1996): Mechanisms of action of atypical antipsychotic drugs: a critical analysis. Psychopharmacology (Berl) 124: 2–34
Jernigan TL, Zisook S, Heaton RK, Moranville JT, Hesselink JR, Braff DL . (1991): Magnetic resonane imaging abnormalities in lenticular nuclei and cerebral cortex in schizophrenia. Arch Gen Psychiatry 48: 881–890
Lee H, Tarazi FI, Chakos M, Wu H, Redmond M, Alvir JM, Kinon BJ, Bilder R, Creese I, Lieberman JA . (1999): Effects of chronic treatment with typical and atypical antipsychotic drugs on the rat striatum. Life Sci 64: 1595–1602
LeMoing JP, Edouard S, Levron JC . (1993): Determination of risperidone and 9-hydroxyrisperidone in human plasma by high performance liquid chromatography with electrochemical detection. J Chromatogr 614: 333–339
Lieberman J, Chakos M, Wu H, Alvir J, Hoffman E, Robinson D, Bilder R . (2001): Longitudinal study of brain morphology in first episode schizophrenia. Biol Psychiatry 49: 487–499
Mattson MP, Duan W, Lee J, Guo Z . (2001): Suppression of brain aging and neurodegenerative disorders by dietary restriction and environmental enrichment Molecular Mechanisms. Mech Ageing Dev 122: 757–778
McCarley RW, Wible CG, Frumin M, Hirayasu Y, Levitt JJ, Fischer IA, Shenton M . (1999): MRI anatomy of schizophrenia. Biol Psychiatry 45: 1099–1119
Meshul CK, Casey DE . (1989): Regional, reversible ultrastructural changes in rat brain with chronic neuroleptic treatment. Brain Res 489: 338–346
Meshul CK, Stallbaumer RK, Taylor B, Janowsky A . (1994): Haloperidol-induced morphological changes in striatum are associated with glutamate synapses. Brain Res 648: 181–185
Miyamoto S, Duncan GE, Mailman RB, Lieberman JA . (2000): Developing Novel Antipsychotic Drugs: Strategies and Goals. Curr Opin Cen & Periph Nerv Syst Invest Drugs 2: 25–39
Muller P, Seeman P . (1977): Brain neurotransmitter receptors after long-term haloperidol: dopamine, acetylcholine, serotonin, alpha-noradrenergic and naloxone receptors. Life Sci 21: 1751–1758
Paxinos G, Watson C . (1998): The Rat Brain in Stereotaxic Coordinates 4th ed San Diego/London, Academic Press
Regeur L, Pakkenberg B . (1989): Optimizing sampling designs for volume measurements of components of human brain using a stereological method. J Microsc 155: 113–121
Remington G, Kapur S . (2000): Atypical antipsychotics: are some more atypical than others?. Psychopharmacology (Berl) 148: 3–15
Roberts RC . (2001): Effect of chronic olanzapine treatment on striatal synaptic organization. Synapse 39: 8–15
Roberts RC, Gaither LA, Gao XM, Kashyap SM, Taminga CA . (1995): Ultrastructural correlates on haloperidol-induced oral dyskinesias in rat striatum. Synapse 20: 234–243
Rossi A, Stratta P, D'Albenzio L, Tartaro A, Schiazza G, DiMichele V, Bolino F, Casacchia M . (1990): Reduced temporal lobe areas in schizophrenia: Preliminary evidences from a controlled multiplanar magnetic resonance imaging study. Biol Psychiatry 27: 61–68
Scheepers FE, Gispen de Wied CC, Hulshoff Pol HE, van de Flier W, van der Linden JA, Kahn RS . (2000): The effect of clozapine on caudate nuclei volume in schizophrenic patients previously treated with typical antipsychotics. Neuropsychopharmacology 24: 47–54
Scheepers FE, Gispen de Wied CC, Hulshoff Pol HE, Kahn RS . (2001): Effect of clozapine on caudate nucleus volume in relation to symptoms of shizophrenia. Am J Psychiatry 158: 644–646
Shenton ME, Kikinis R, Jolesz FA, Pollak SD, LeMay M, Wible CG, Hokama H, Martin J, Metcalf D, Coleman M . (1992): Abnormalities of the left temporal lobe and thought disorder in schizophrenia. A quantitative magnetic resonance imaging study. N Engl J Med 327: 604–612
Shenton ME, Wible CG, McCarley RW . (1997): A review of magnetic resonance imaging studies of brain abnormalities in schizophrenia. In Krishnan K.R.R. Doraiswamy P.M. Brain Imaging in Clinical Psychiatry New York, Marcel Dekker, Inc
Simpson GM, Cooper TB . (1978): Clozapine plasma levels and convulsions. Am J Psychiatry 135: 99–100
Staal WG, Hulshoff Pol HE, Schnack HG, Hoogendoorn MLC, Jelma K, Kahn RS . (2000): Structural brain abnormalities in patients with schizophrenia and their healthy siblings. Am J Psychiatry 157: 416–420
Suddath RL, Casanova MF, Goldberg TE, Daniel DG, Kelsoe JR, Weinberger DR . (1989): Temporal lobe pathology in shizophrenia: A quantitative magnetic reasonance imaging study. Am J Psychiatry 146: 464–472
Suddath RL, Christison GW, Torrey EF, Casanova MF, Weinberger DR . (1990): Anatomical abnormalities in the brains of monozygotic twins discordant for schizophrenia. N Eng J Med 332: 789–794
Swayze VW, Andreasen NC, Alliger RJ, Yuh WT, Ehrhardt JC . (1992): Subcortical and temporal structures in affective disorder and schizophrenia: a magnetic resonance imaging study. Biol Psychiatry 31: 221–240
Waddington JL, O'Callaghan E . (1997): What makes an antipsychotic “atypical”? Conserving the definition. CNS Drugs 7: 341–346
Acknowledgements
This research was supported by T32 ESO7126, and grants from the Foundation of Hope, the Theodore and Vada Stanley Foundation, and Eli Lilly and Company. The authors would like to thank MacNeil Pharmaceuticals for the gift of haloperidol, Novartis Pharmaceuticals for the gift of clozapine, Janssen Pharmaceutica for the gift of risperidone, and Eli Lilly, Inc., for the gift of olanzapine.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andersson, C., Hamer, R., Lawler, C. et al. Striatal Volume Changes in the Rat Following Long-term Administration of Typical and Atypical Antipsychotic Drugs. Neuropsychopharmacol 27, 143–151 (2002). https://doi.org/10.1016/S0893-133X(02)00287-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(02)00287-7
Keywords
This article is cited by
-
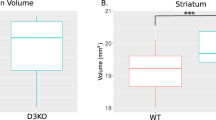
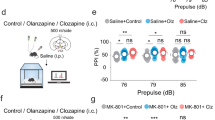
Role of D3 dopamine receptors in modulating neuroanatomical changes in response to antipsychotic administration
Scientific Reports (2019)
-
Neural Stem Cell Tumorigenicity and Biodistribution Assessment for Phase I Clinical Trial in Parkinson’s Disease
Scientific Reports (2016)
-
Genetic sex and the volumes of the caudate-putamen, nucleus accumbens core and shell: original data and a review
Brain Structure and Function (2016)
-
SELENBP1 expression in the prefrontal cortex of subjects with schizophrenia
Translational Psychiatry (2015)
-
Repetitive and self-injurious behaviors: associations with caudate volume in autism and fragile X syndrome
Journal of Neurodevelopmental Disorders (2013)