Abstract
Diabetes Mellitus (DM) is the most common metabolic disorder and the most common cause of death in eastern populations, with prevalence estimated to be at the level of epidemic illness. Despite medical attention, psychological factors remain a significant contributor to DM, requiring effective psychological interventions. This study evaluated the effects of Mindfulness-integrated Cognitive Behavior Therapy (MiCBT) on depression, treatment adherence, and control of blood glucose of 25 Iranian patients (11 males and 14 females, mean age = 45.6) with type 2 DM, randomly assigned to either an 8-session MiCBT (n = 12) or treatment-as-usual (TAU) (n = 13). We present a theoretical conceptualization and detailed step-by-step implementation of MiCBT, and an assessment of its effectiveness in this sample. While no between-group differences were found at pre-treatment on any of the measures, the MiCBT group showed a significantly greater reduction in depression and greater treatment adherence than the TAU group at post-treatment. The MiCBT group also showed a significantly greater blood sugar reduction than the TAU group at 6-week follow-up. Within-group analysis found no significant change on any of the measures for TAU, whereas the MiCBT group reported a significant decrease in depression and increase in treatment adherence from pre- to post-treatment and maintained at 6-week follow-up. Blood sugar reduction also only occurred in the MiCBT group from pre- to post-treatment. Replication studies with larger samples are necessary to confirm these findings and validate the transdiagnostic efficacy and transcultural applicability of MiCBT in type 2 DM.
Similar content being viewed by others
1 Introduction
Type 2 Diabetes Mellitus (DM) is a metabolic disorder caused by pancreatic deficiency in insulin secretion or defects in its function, or both [1, 2], principally resulting from being overweight and lacking physical activity. In the past two decades, DM has drawn much attention in the research literature and is recognized as a major threat to global development [3, 4]. It is the most common metabolic disorder and the most common cause of death in eastern populations [5]. Two decades ago, its prevalence had already increased to the level of epidemic illness [6, 7], decreasing longevity by five to 10 years [8]. With an estimated 1.6 million deaths directly caused by diabetes in 2016, WHO estimates that diabetes was the seventh leading cause of death in 2016.
A considerable number of people with diabetes experience emotional difficulties which have been associated with treatment complications, including depressed mood, reduced quality of life, poor self-care behavior, negative appraisals of insulin therapy, reduced glycemic control and subsequent adverse cardiovascular outcomes, including mortality [9, 10]. There is evidence of a bidirectional association between depressive symptoms and DM, where depressive symptoms are associated with an increased risk of developing DM over time and DM levels are associated with an increased risk of developing depression over time [11,12,13]. In Iran, the prevalence of depressive symptoms among patients with diabetes is between 71 and 78 percent [14, 15], compared to between 28 and 34 percent in the general population [16].
A recent study suggests that insulin resistance has a shared pathogenic mechanism between depression and type 2 DM [17]. This could be relevant to the observation that depression often precedes diabetic symptoms in type 2 DM, and patients with higher levels of depression have been found to experience more complications with diabetes, reduced adherence to medical treatment and health behavior, such as maintaining a healthy diet, and depression seems to correlate with severe deteriorations and eventually death in patients with DM [18]. Naicker et al.’s longitudinal study examined mortality risk associated with type 2 DM and the presence of comorbid affective symptoms in a large Norwegian sample over 18 years [19]. Their study showed that mortality risk (1) increased in the presence of depression, anxiety, or both, (2) was higher with comorbid depression only, and (3) the highest risk of death occurred in men with type 2 DM and symptoms of depression only.
Depressive symptoms in people with diabetes appear to complicate medical intervention and correlate with therapeutic failure [20]. Given the relevance of comorbid psychological conditions in DM, it has been proposed that psychological interventions are important to maximize self-management and improve both glycemic and psychosocial outcomes in patients with DM [21]. Among various methods, mindfulness training has been used as an adjunct skillset to cognitive behavior therapy (CBT) or used as an alternative or complementary intervention [22]. Mindfulness originates from Buddhist teachings, and involves “moment-by-moment awareness that is cultivated by purposefully paying attention to things we ordinarily don't think of” ([23], p. 2). More specifically, mindfulness requires attentiveness to an immediate experience that is free from self-referential evaluation, value-based association or emotional reactivity [24, 25].
Since its inception in Western therapy [26], mindfulness training has been used effectively in numerous therapeutic programs to assist in attention and emotion regulation [27]. Mindfulness-based interventions (MBIs) are increasingly used to address a wide range of psychological and medical disorders [28] and have been shown to be efficacious in the clinical treatment of anxiety and mood dysfunctions [29,30,31]. There is also some evidence that MBIs may improve psychological and biological diabetes-care parameters. For instance, randomized controlled trials of MBIs have shown improvement in emotional well-being and decreased symptoms of depression and anxiety, as well as general psychological distress at 1-month follow-up [32], 1- and 2-month follow-up [33] and 3- to 9-month follow-up [34]. Other RCTs show that MBIs have resulted in reduced diabetes-related stress from pre- to post-treatment [35], and improvement in quality of life and use of coping strategies to improve diabetes-related self-care maintained at 3-month follow-up [22], although variations in the magnitude of their effects can occur across methods and patient groups (e.g., [36, 37]). In addition, these benefits were equally observed when patients attended individual sessions [38].
Mindfulness-integrated Cognitive Behavior Therapy (MiCBT) [39] is one of the evidence-based manualised MBIs, developed between 2001 and 2004 [40] to systematically integrate mindfulness meditation, in the Burmese Vipassana/Insight tradition, with core elements of cognitive-behavior therapy. MiCBT is usually delivered through a four-stage program across eight to 12 sessions, but it can be further adjusted according to the type and severity of symptoms. Participants learn first to internalize attention and develop experiential awareness and equanimity to improve attention and emotion regulation, and then use various types of exposure methods to externalize these skills in the contexts in which their impairment is triggered or maintained (see Method section for details).
The increasing use of MiCBT in clinical settings is partly due to its transdiagnostic applicability and to its emphasis on interoceptive desensitization and equanimity, both during mindfulness training and across all integrated behavioral tasks included in this approach [41]. The theoretical foundation of MiCBT is the co-emergence model of reinforcement [39, 42], which extends the traditional understanding of operant conditioning. This theoretical conceptualization is summarized in Appendix 1. There is mounting multidisciplinary evidence for the advantage of increasing interoceptive awareness and acceptance in mental health conditions [43]. These studies show clear indications of impaired interoceptive capacity in mental health disorders, which may explain why gains in interoceptive awareness and acceptance through mindfulness training tend to have transtherapeutic benefits [42, 44]. Accordingly, the transdiagnostic approach of MiCBT is of particular interest in conditions such as Diabetes because it enables clinicians to address active clinical symptoms and complex comorbidity across a wide range of conditions [45]. A quasi-experimental study also suggested that MiCBT is equally effective when implemented with individuals and groups (Unpublished), which provides flexibility in clinical settings where facilitating groups is impractical.
Several randomized controlled trials (RCTs) demonstrated the effectiveness of MiCBT across a range of contexts and conditions. For example, MiCBT was shown to be effective in treating anxiety and depression in pregnant women [46] and in women with multiple sclerosis [47] from pre- to post-treatment, reducing symptoms of obsessive–compulsive disorder with maintained gains at 1-month follow-up [48], reducing perceived pain and increasing pain self-efficacy in patients with breast cancer with gains maintained at 1-month follow-up [49], reducing anxiety, depression and fatigue while improving sleep quality and hope in patients with Multiple Sclerosis with gains maintained at 2-month follow-up [50, 51], changing gene expression in women with perinatal depression [52], and reducing sports-anxiety and pessimism, and increasing flow in competitive athletes from pre- to post-intervention [53]. Other studies demonstrated the efficacy of the interoceptive desensitization method used in MiCBT in both chronic pain with gains further increased at 2-month follow-up [54] and induced pain in student samples [55].
The effects of MiCBT on type 2 DM and co-morbid symptoms were initially explored in a quasi-experimental study in a New-Zealander population, where type 2 DM is also of epidemic proportion (Unpublished). Participants reported an overall improvement of self-efficacy in managing unhelpful behaviors and unpleasant thoughts, body sensations, emotions and relationship with others from pre- to post-treatment. They also reported an increased ability to manage clinical symptoms, greater self-compassion and improvement in diabetes self-care. We are aware of one study which investigated the effectiveness of MiCBT in type 2 DM in Iran [56]. The results showed that MiCBT led to significant decrease in emotional distress and improved treatment adherence and quality of life in people with DM.
The aim of the present study was to provide an evaluation of the effectiveness of MiCBT in an Iranian population with type 2 DM attending the Kurdistan Clinic of Diabetes, using an adaptive delivery of MiCBT that takes into account cultural and religious complexities in an Iranian population when implementing a methodology that partly originates from a Buddhist contemplative tradition. We provide a detailed clinical implementation of both stages of MiCBT implemented in this experiment beyond what other studies have presented thus far, including verbatim task instructions and clinical dialogues in Appendix 2. We were particularly interested in exploring the possible effects of MiCBT on comorbid depression, poor adherence to medical treatment and diabetes self-care, including blood glucose control.
Based on previous findings (e.g., [32, 37]), we predicted that depressive symptoms on the Beck Depression Inventory would decrease significantly more in the MiCBT group than in the treatment-as-usual (TAU) group. It was also hypothesized that participants in the MiCBT group would be more able to adhere to diabetes treatment and related self-care on the Adherence to Therapy Scale than those in the TAU group. We also expected that decreased depression, greater treatment adherence and related self-care following treatment would result in a greater blood sugar reduction in the MiCBT group than in the control group.
2 Method
2.1 Participants
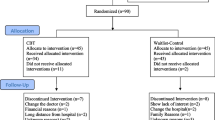
All potential participants consisted of Kurdish-speaking patients with type 2 DM attending the Kurdistan Clinic of Diabetes for their medical treatment, most of whom had a long-term DM diagnosis. Ninety-five patients met the criterion for literacy: having at least the ability for reading and writing that equals elementary school education. From these, 36 met the remaining criteria and were invited to participate. The clinical criteria for inclusion were: (1) scoring at least 15 on the Beck Depression Inventory (BDI) as per Viinamäki et al.’s [57] recommendations, (2) having no other psychological intervention implemented concurrently, and (3) having no suicidal thoughts or intent, and no psychotic states or manic symptoms. Exclusion Criteria were (1) the necessity for, or existing prescription of, antidepressants or other psychiatric medication, (2) change of drugs for diabetes control, and (3) emerging suicidal ideation in the period of the intervention. A recurring reason for exclusion was logistical. Some participants could not attend due to living too far from the center. Another was that many were overly suspicious and unwilling to give informed consent. These reduced the potential sample down to 36. Consent issues, despite our strict application of standard Helsinki ethical guidelines, may be a reflection of population suspiciousness, sense of oppression, and inflated need for caution.
Of 36 possible participants, 25 (11 males and 14 females, mean age = 45.6) volunteered and provided consent to participate. Participants were randomly assigned to either the MiCBT group (n = 12) or the TAU (control) group (n = 13). All participants had been diagnosed with type 2 DM between 2 and 10 years prior to enrolling in the study. However, randomization did not specifically take illness duration into account. The study was explained to participants during their first contact with the experimenter. Participants then completed an initial demographics questionnaire, which included baseline data for levels of depression and medical treatment adherence. There were no significant between-group differences on demographic and baseline data (see Table 1).
In both MiCBT and TAU groups, four participants failed to complete the forms and their data were excluded from the study. Their missing data were not obtainable. Intent-to-treat analysis (ITT) was not performed on the basis that ITT can only be performed where there is complete outcome data for all randomized participants [58] and the sample was too small to perform Maximum Likelihood Estimation or multiple imputation. Accordingly, only the data from eight participants in the MiCBT group and nine in the TAU group were retained. A comparison of baseline characteristics of participants who dropped out and those who did not is presented in Table 2. There were no significant differences in age and in all measures between included and excluded participants.
2.2 Materials
For their home practice of mindfulness meditation, participants in the MiCBT group received either a 60-90 min individual session with audiotapes or a printed script format of the same instructions if they could not use the audio instructions due to not having means of playing audio instructions. Some participants had no smart phones or audio player, some had hearing problems. The original audio instructions [59] were first transcribed and translated in Farsi with the author’s permission.
Measures. The Beck Depression Inventory (BDI) [60] is a widely used self-report depression rating scale with 21 items requiring answers scored on a 4-point scale, ranging from 0 to 3. It is administered across a wide range of psychological disorders for adults and adolescents. The BDI was found to have good internal consistency and good convergent validity; Cronbach’s alpha between 0.73–0.90. We used the translated version (BDI-I) in Farsi [61], which shows good convergent validity and internal consistency; Cronbach alpha between 0.78–0.92. Despite the cross-cultural sample for this study, translated items of the BDI accurately captures the expression of depression in the Iranian population, in which it has been used extensively.
The Adherence to Therapy Scale [62, 63] is a 4-item self-report questionnaire used to measure the extent to which a person follows a therapy protocol, do an intended activity or prevent counterproductive behavior. In the current study, participants were asked to include DM-specific medical regimens, such as taking medication, exercising, following a diet, and keeping regular medical appointments. It is scored on a 6-point Likert scale, ranging from very poor (1) to excellent adherence (6). Its Farsi version [63] showed good convergent validity and acceptable internal consistency; Cronbach’s alpha = 0.71. The Glycosylated Hemoglobin Test (HbA1c) measures a person’s average levels of blood glucose over the past 2 to 3 months.
2.3 Procedure
After a first consideration of sufficient literacy and diagnosis (especially type of DM), the participants were invited by telephone for a pre-enrollment interview, during which the inclusion criteria were assessed, and the baseline measures implemented. Those who met inclusion criteria were invited to take part in the study and attend eight weekly sessions. These participants were randomly assigned to two groups: a MiCBT group and a TAU group through a simple randomized lottery. The intervention group received eight 60 to 90-min individual sessions of MiCBT, while the TAU group did not receive any psychological intervention during this period, but continued to receive their usual medical treatment, which included as frequent (medical) consultations as required by their medical practitioner, although these were shorter than MiCBT sessions. Equally, participants in the MiCBT group received medical consultations as required by their medical practitioner.
A postgraduate student of clinical psychology and practitioner of mindfulness meditation implemented MiCBT following Cayoun’s implementation manual [39], while supervised by an experienced clinical psychologist. The student had a personal regular practice of mindfulness meditation for about 12 months prior to the commencement of the study. The supervising clinical psychologist had a personal regular practice of mindfulness meditation for over five years, but neither was particularly experienced in MiCBT. Therapy was delivered in individual sessions, rather than in group, because it was thought to be a more suitable approach for an Iranian population. The first session included a DM-specific goal-setting activity as part of ‘therapy contracting’, and baseline data were collected. All participants were given their routine diabetic drugs and only the intervention group undertook Stage 1 (intrapersonal regulation) and Stage 2 (behavioral regulation) of the MiCBT program, summarized in Table 3.
Participants in Stage 1 were taught to develop various mindfulness skillsets to improve attention and emotion regulation [27, 39], with an emphasis on body-scanning methods for the development of equanimity, as per the traditional teaching of Vipassana meditation in the Burmese tradition of Ledi Sayadaw, U Ba Khin, and Goenka [64]. Equanimity is an attitude toward personal experience which combines the inhibition of learned reactivity and the unconditional acceptance of the present experience [65]. Equanimity has been defined as “an even-minded mental state or dispositional tendency toward all experiences or objects, regardless of their affective valence (pleasant, unpleasant or neutral) or source” ([66], p. 357). Participants developed a degree of equanimity by surveying the body part by part, continuously and systematically, while learning to experience body sensations “just as body sensations” and preventing automatic reactions (see Appendix 2 for detailed implementation).
Once participants learned to apply and further develop equanimity with common stressors during the first three weeks of Stage 1 MiCBT, they undertook Stage 2 of MiCBT, as per the manualized instructions. However, more time was provided to participants who needed it and Stage 2 was delayed. The individual implementation facilitated these occasional adjustments. Stage 2 consists of two integrated exposure methods (imaginal and in vivo) that capitalize on the levels of equanimity developed during Stage 1 to decrease both experiential (interoceptive) and situational avoidance. Although the manualised structure of these MiCBT stages was purposefully unchanged to preserve and verify its transdiagnostic applicability, both interoceptive and exteroceptive exposure methods were set to reduce DM symptoms proliferation (see Appendix 2 for detailed implementation). It is recommended that the delivery schedule remains flexible enough to be delivered in an 8- to 12-week period, so that patients who struggle to acquire the expected skills have more time to do so before transitioning to subsequent behavioral and meditative stages [39].
Stage 3 provides training in interpersonal communication, and Stage 4 provides compassion training and explicit ethics (see [45], for detailed procedure of these stages). In this study, only stages 1 and 2 from the standard protocol were implemented within the eight sessions. This was primarily because these stages seemed to include the skillsets that were most congruent with the participants’ condition, and most culturally relatable to participants. The efficacy of the intervention with the truncation of stages was also a measurement of interest.
At the start and completion of the program, and at 6-week follow-up, all participants completed the BDI and Adherence to Therapy Scale and took the HbA1c test. Along with the other measures, the HbA1C test was taken at pre-treatment, post-treatment and follow-up. Each HbA1C test was sent to a medical laboratory for analysis. TAU involved the usual medical treatment, including medical visits, medication under the control of their physician and suggested diet, but excluded treatments of depression, such as antidepressants and psychological therapy. After the follow-up data and HbA1c test were collected on-site after meeting with the experimenter, participants in the TAU group received two sessions of counselling, relaxation training and mindfulness meditation.
2.4 Design
A 2 × 3 mixed factorial design was used, with Group (MiCBT, TAU) and Time (Pre-treatment, Post-Treatment, and 6-week follow-up) as independent variables. The dependent variables were the scores on each measure described above. Analyses of Variance (ANOVAs) were used to detect main effects and interactions between Group and Time, and pairwise comparisons and t-tests with Bonferroni adjustment were used for post-hoc analyses. Mauschly’s Test of Sphericity indicated that the assumption of sphericity was not violated for all ANOVAs. Raw data analysis found no outliers and Shapiro-Wilks and Kolmogorov–Smirnov tests showed a normal distribution. Incomplete data sets had to be excluded as the sample size was too small to use intent-to-treat analysis. Alpha levels were held at 0.05 and partial eta squared (ηp2) was used to estimate effect sizes. As per Cohen [67], norms for partial eta-squared were: small effect = 0.01; medium effect = 0.06; and large effect = 0.14.
3 Results
Baseline characteristics of participants with complete dataset (included in the study) and those with incomplete dataset (excluded from the study) were calculated for each group and for the entire sample using independent-samples t-tests. Table 4 shows means, standard deviations (SDs) and range for the three dependent measures.
4 Depression
A 2 × 3 ANOVA shows a significant Group by Time interaction, F(2,30) = 41.05, p < 0.001, ηp2 = 0.78, indicating a significantly greater decrease in depression in the MiCBT group than in the TAU group. A 2 × 2 ANOVA was used to assess the effect of MiCBT on Depression from pre- to post-treatment across groups. There was a significant Group by Time interaction, F(1,16) = 73.35, p < 0.001, ηp2 = 0.82, showing a larger decrease in depression from pre- to post-treatment in the MiCBT group, than in the TAU group. The pre-treatment to follow-up analysis also showed a significant interaction F(1,16) = 18.138, p < 0.001, ηp2 = 0.681, but no significant difference was found from post-treatment to follow-up F(1,16) = 0.084, p < 0.775, ηp2 = 0.617. Table 5 displays t-tests used for post-hoc analysis of group differences on the BDI, and within-subject differences and CIs for each group at each measurement time are shown in Table 6. Overall, the data show no group difference in depression at pre-treatment, and a large and statistically significant decrease in depression from pre- to post-treatment in the MiCBT group only. This difference was maintained at 6-week follow-up and the difference between groups remained. No differences were found in the TAU at any of the measurement times.
4.1 Adherence
To examine the effect of MiCBT on Adherence, a 2 × 3 (Group by Time, respectively) ANOVA was used. Means and SDs are shown in Table 4. There was a significant interaction of Adherence by Time F(2,30) = 111.58; p < 0.001; ηp2 = 0.920, showing a significantly greater increase in levels of adherence to medical treatment in the MiCBT group than in the TAU group. A 2 × 2 ANOVA found a significant interaction of Time by Group, F(1,16) = 155.68, p < 0.001, ηp2 = 0.931, showing that adherence to medical treatment improved significantly more in the MiCBT group than in the TAU group from pre- to post-treatment. There was also a significant between-group difference in the same direction from pre-treatment to follow-up with large effect size F(1,16) = 7.733, p = 0.013, ηp2 = 0.66. Neither group showed a significant difference between post and follow-up measures F(1,16) = 0.084, p < 0.229, ηp2 = 0.84. Table 5 displays t-tests used for post-hoc analysis of group differences on adherence, and within-subject differences and CIs for each group at each measurement time are shown in Table 6. Overall, the data show no group difference in Adherence at pre-treatment, and a large and statistically significant increase in Adherence from pre- to post-treatment in the MiCBT group only. This difference was maintained at 6-week follow-up and the difference between groups remained. No differences were found in the TAU at any of the measurement times.
4.2 Blood sugar levels (HbA1c)
A 2 (Group) × 3 (Time) repeated measures ANOVA was used to examine the effect of MiCBT on HbA1C. Means and SDs for HbA1c are shown in Table 2. There was a significant Group by Time interaction F(2,30) = 2.213, p = 0.012; ηp2 = 0.186. As shown in Table 5, post-hoc analysis shows a significant between-group difference in blood sugar at 6-week follow-up. As shown by the within-subject analysis displayed in Table 6, pairwise comparisons indicate a significant and large decrease in blood sugar levels from pre- to post-treatment in the MiCBT group, but not in the TAU group. There was also a trend toward significance (p = 0.067) in blood sugar reduction with a large effect size from pre-treatment to follow-up, and no difference between post-treatment and follow-up.
5 Discussion
The aim of this pilot study was to evaluate the effects of adding Mindfulness-integrated Cognitive Behavior Therapy (MiCBT) to TAU compared to TAU alone in an Iranian sample of patients with type 2 DM. Our results support the results of previous studies of the efficacy of MBIs in improving the wellbeing of people with DM [10, 32, 33]. They also support our first hypothesis. Participants who undertook the MiCBT program experienced a significant reduction in depression from pre- to post-treatment, which was maintained at 6-week follow-up. No depression reduction was found in the TAU group and there was no between-group difference in depression at pre-treatment. Also, in agreement with our second hypothesis, there was a significant increase in medical treatment adherence in the MiCBT group from pre- to post-treatment, which was also maintained at 6-week follow-up. This did not occur in the TAU group. Our third prediction was also supported by the data, showing a significant blood sugar reduction from pre- to post-treatment in the MiCBT group, maintained at 6-week follow-up, and a significant between-group difference at 6-week follow-up. While these early results need to be replicated, they support the increasing observation that MBIs may be useful alternative ways of alleviating the burden of depression and reduced self-care behavior in people with DM.
None of the participants reported aversive effects from practicing mindfulness. This may be due to using a trauma-sensitive methodology which includes individual implementation, rather than group delivery. The small sample size may have also reduced the probability of undesired effects. It is not clear whether this is generalizable to large samples.
The comorbidity of depression with DM is well established, and more so in socially disadvantaged populations such as that of Iran in general. Renn et al.’s [68] cross-sectional study of depressive symptomatology in 424 patients with prediabetes or type 2 DM from disadvantaged populations in the US demonstrated that the majority (67.7%) of DM patients also showed depressive symptoms. This is close to the high prevalence of depression found in Iranian diabetic patients (71–78%), which seems proportionally related to the already high (37%) prevalence of depression in the general Iranian population [69]. Since depressive symptoms include dysregulated diet and low motivation for activity and exercise, it is possible that depression is driving the high rate of type 2 DM in Iran and other disadvantaged populations. If this were the case in the current study, it could be that the greater effect of MiCBT in the current study may have been on decreasing depressive symptoms, as measure by the BDI, which in turn may have had an effect on participants’ improved self-care, as measured here through treatment adherence and glycemic control. Accordingly, it is difficult to know whether this might impact the generalizability of the findings to other populations. To clarify this possible causal mechanism, future studies could examine the effects of MiCBT on participants with type 2 DM with and without depression and measure the effects that MiCBT (or other MBIs) may have on DM alone.
6 Limitations
A limitation of this study is the small sample size, and therefore lowered statistical power. With such small groups, caution must be applied when interpreting the results, as the findings might not be generalizable to the diabetic population at large. RCTs of MiCBT tend to show large effect sizes (d) ranging from 0.8 to 1.6. In this study, effects sizes were overall very large as well and easy to detect, but small effects in the TAU group may have been missed. Randomization could have also been improved by taking the duration of illness into account. Since all participants had been diagnosed between 2 and 10 years prior to enrolling in the study, and illness duration influences the effectiveness of diabetes education on lifestyle behavior modification and glycemic control [70], some variance may have been introduced. Ko et al. [70] recommend employing more intense, regular, and sustained reinforcement for people with longstanding type 2 diabetes (≥ 3 years). Accordingly, it is not clear whether illness-duration effects are more related to diabetes education than a comprehensive behavioral intervention such as MiCBT. Our results must therefore be interpreted with caution. Future studies with larger samples and controlling for illness duration are needed to assist in a more reliable examination of MiCBT effects in DM.
It was initially intended to measure participants’ adherence to meditation practice protocol. However, the participants’ home practice records were not consistently used or provided to the researchers and tracking daily practice could not be done effectively. Consequently, this measurement was not included in the analysis, which limits the ability to verify whether or not the amount of home practice of mindfulness impacted the outcomes. Future studies will need to adopt a more reliable protocol for measuring home practice. For example, where possible, a smart phone app could be used to guide and monitor practice (e.g., [71]).
Another limitation was the differential delivery of practice instructions in the MiCBT group. Whereas the standard means of learning to meditate in the MiCBT protocol is the intermittent use of audio instructions and silent practice, some participants in this study used a printed script format of the same instructions if they could not use audios (mostly due to logistics). Even though both audio and printed instructions contained the same information, the use of different learning modalities may have impacted practice accuracy or behavior, and potentially the outcome. Although participants in the MiCBT group improved significantly from pre to post treatment and maintained their gains at follow-up, there may have been within-group differences. All meditating participants learned each new method auditorily each week with the experimenter, but using home practice written instructions for the rest of the week would have required memory resources that were not necessary for those using audio instructions. Given the small sample per group, we were not able to do a meaningful statistical analysis for possible subgroup differences caused by these different learning modalities. Future studies would prevent potential confounds by providing home practice materials via the same delivery method. For participants who are unable to use a smart phone, when possible, researchers could provide a basic MP3 (audio) player or upload audio files on a website for participants to access online.
The altered implementation of the manualised MiCBT protocol from four to two stages was a potential limitation, especially in preventing relapse, which is the specific purpose of Stage 4 (the ‘empathic stage’). Our 6-week follow-up period was too short to elucidate this possibility. However, the simplified protocol in this study was also an opportunity to observe the beneficial effects of using only Stages 1 and 2 in type 2 DM. Developing attention- and emotion-regulation skills in Stage 1 and integrating these within exposure techniques in Stage 2 provided substantial benefits to participants. However, this small-scale study does not permit any reliable assertion that the effects of a simplified MiCBT program equates those of a full version. While the MiCBT approach is flexible enough to be adapted to client needs in clinical settings, time constraints in this study did not allow for any adaptation where it was needed. While this would have been a routine adjustment of the program in clinical settings, with a longer delivery for severe symptoms and personality disorders (Cayoun et al. [24]), the academic context of this study did not allow for adopting the developer’s recommendation of a flexible 8 to 12-session delivery. For instance, the daily practice of loving kindness and explicit ethics during Stage 4 teaches people to prevent harming themselves and others out of compassion. It teaches them to value themselves and care for themselves, which also means caring for their body and general well-being, including caring about what they eat. A self-implementation protocol of MiCBT suggests that the program can be further lengthened on a need basis. Hence, it is recommended that future studies allow more flexible time for implementation and approximate real-life delivery of the program (8–12 sessions), as it is possible that people with DM may make further progress, especially with decreasing blood sugar levels, if they are given more time. Nonetheless, the present study also shows that a simplified implementation remained efficacious in reducing the target symptoms in this sample.
Finally, mindfulness skills were not assessed. It is therefore difficult to know whether all or only some skillsets implemented in the first two stages of MiCBT were most beneficial. Including a mindfulness measure validated for the Iranian population would be advantageous in future studies. In addition, given the central role of equanimity in the cultivation and maintenance of mindfulness, future MBI studies with type 2 DM will benefit from using a measure of equanimity which includes items related to craving and avoidance, such as “I can pay attention to what is happening in my body without disliking or wanting more of the feeling or sensation” [64].
7 Future directions
The scope and sample size of this study did not allow for an examination of the possible contribution of gender and personality factors. Nyklíček et al. [36] found that women with diabetes and outpatients low in extraversion benefited most from Mindfulness-based Cognitive Therapy [31]. It is not clear whether these factors would also affect MiCBT outcomes, and future study may investigate this possibility. It may be that some MBIs are more suited to various patient groups with DM, such as individuals with high or low comorbidity, with or without personality disorders. In addition, assessing the possible inter-relatedness of psychological factors in DM would clarify the psychological profiles of DM and assist in selecting therapeutic goals more effectively.
MiCBT was shown to yield similar transdiagnostic benefits whether implemented in group or individual clinical settings. However, it is not clear whether such clinical settings would yield the same results for people with DM. Tovote et al. [37] used an individual delivery of MBCT and CBT, which produced significant reductions in depressive and anxiety symptoms, improved well-being, and diabetes-related distress, but no blood sugar reduction. It is not clear whether group dynamics, such as peer pressure, could have motivated participants to adhere to self-care and medical treatment, resulting in blood sugar reduction. It would be beneficial for future studies to investigate the possible differential effects of group versus individual delivery of MBIs in patients with DM.
Moreover, future studies may include mediation analysis, as it is not clear in this study whether improved emotion-regulation, as reflected through improved mood, mediated the effects on other variables (adherence and blood sugar); Alternatively, it is also possible that preventing avoidance through exposure (in Stage 2) may have improved adherence and assisted participants in feeling empowered and hopeful, thereby decreasing symptoms of depression. We also suggest that a longer follow-up period is necessary to show the fuller extent of the effect over time, since more time is necessary to address complex variables, such as personality factors. Future studies may show better outcome reliability by including a 6-month follow-up measure. Future studies may also include a way of rating the sessions for adherence and leader competence. Although the program in the current study was followed with integrity, such measure was not included. It would also be useful to compare the effects of the truncated version of MiCBT implemented in this study (stages 1 and 2) with the full version comprising the four stages. It is possible that a difference may emerge in the transdiagnostic efficacy. Since stages 1 and 2 focus on integrating mindfulness and CBT to assist in self-regulation and reducing avoidance, and 3 and 4 address impairments in interpersonal contexts and poor self-compassion, it may be that people with DM and comorbid interpersonal dysfunctions may benefit more from the full program.
8 Conclusion
In this study, adding MiCBT to TAU was markedly more effective than TAU alone in reducing depressive symptoms, increasing adherence to therapy and reducing blood sugar levels in people with type 2 DM. This is in support of the extant literature, which shows that MBIs are useful adjunctive treatments of DM, as they can help address common comorbid psychological symptoms. However, this study was limited by a small sample size and used a simplified implementation than the standard four-stage MiCBT protocol. To establish the effectiveness of MiCBT in this population, studies with larger sample sizes are needed to compare group with individual implementation, investigate gender and personality variables, and use longer follow-up periods to increase outcome reliability.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon request.
References
World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications: Report of a WHO consultation. Part 1, Diagnosis and classification of diabetes mellitus; 1999. https://apps.who.int/iris/handle/10665/66040
Committee CDACPGE. Clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2008;32(Suppl 1):10–3.
World Health Organization. Diabetes: Key facts; 2018. https://www.who.int/news-room/fact-sheets/detail/diabetes
Alwan A. Raising the priority accorded to diabetes in global health and development. Int J Diabetes Mellitus. 2010;2(3):139–40. https://doi.org/10.1016/j.ijdm.2010.10.001.
Delavari A, Hazaveh AM, Noroozi-nezhad A, Yar-ahmadi S. Diabetes and physician, The national program for control and prevention of diabetes. Nashereseda publication; 2004. (in Persian)
Munir SA. Global epidemic of diabetes. Nishtar Med J. 2010;2(2):56–60.
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14. https://doi.org/10.1016/j.diabres.2009.10.007.
Day C. The rising tide of type 2 diabetes. Br J Diabetes Vasc Dis. 2001;1(1):37–43. https://doi.org/10.1177/14746514010010010601.
Bener A, Al-Hamaq A, Dafeeah EE. High prevalence of depression, anxiety and stress symptom among diabetes mellitus patients. Open Psychiatry J. 2011;5(1):5–12. https://doi.org/10.2174/1874354401105010005.
Son JV, Nyklíček I, Pop VJ, Pouwer F. Testing the effectiveness of a mindfulness-based intervention to reduce emotional distress in outpatients with diabetes (DiaMind): design of a randomized controlled trial. BioMedCentral Public Health. 2011;11:131. https://doi.org/10.1186/1471-2458-11-131.
Beran M, Muzambi R, Geraets A, Albertorio-Diaz JR, Adriaanse MC, Iversen MM, Kokoszka A, Nefs G, Nouwen A, Pouwer F, Huber JW, Andreas Schmitt A, Schram MT, for the European Depression in Diabetes (EDID) Research Consortium. The bidirectional longitudinal association between depressive symptoms and HbA1c: a systematic review and meta-analysis. Diabetic Med. 2021;39(2):e14671. https://doi.org/10.1111/dme.14671.
Escobar Florez OE, Aquilera G, De la Roca-Chiapas JM, Macías Cervantes MH, Garay-Sevilla ME. The relationship between psychosocial factors and adherence to treatment in men, premenopausal and menopausal women with Type 2 Diabetes Mellitus. Psychol Res Behav Manag. 2021;2021(14):1993–2000. https://doi.org/10.2147/PRBM.S342155.
Rajender A, Kanawal K, Chaudhary D, Chaudhri RS, Rajender G, Choudhary P. Study of depression in type 2 diabetes mellitus patients. Int J Med Sci Public Health. 2016;5(9):1874–7. https://doi.org/10.5455/ijmsph.2016.17012016367.
Mousavi SA, Aghayan S, Razavian-Zadeh N, Nourozi N, Khosravi A. Studying depression and general health of type 2 diabetic patients. Health Knowl J. 2009;3:44–8.
Ranjbar K, Sharif F, Dejbakhsh T. Comparing the prevalence and severity of depression among medicated diabetic adults. Hormozgan Phys J. 2007;10:363–9.
Zhuang Q, Shen L, Ji H. Quantitative assessment of the bidirectional relationships between diabetes and depression. Oncotarget. 2017;8:23389–400. https://doi.org/10.18632/oncotarget.15051.
Lyra e Silva NM, Lam MP, Soares CN, Munoz DP, Milev R, De Felice FG. Insulin resistance as a shared pathogenic mechanism between depression and type 2 Diabetes. Front Psychiatry. 2019;10:57. https://doi.org/10.3389/fpsyt.2019.00057.
Sargin H, Cakin I, Sargin M. Diabetes and depression. Turkish J Endocrinol Metab. 2002;6:95–100.
Naicker K, Johnson JA, Skogen JC, Manuel D, Øverland S, Sivertsen B, Colman I. Type 2 Diabetes and comorbid symptoms of depression and anxiety: longitudinal associations with mortality risk. Diabetes Care. 2017;40(3):352–8. https://doi.org/10.2337/dc16-2018.
Clarke DM, Currie KC. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Aust. 2009;190(7):54–60. https://doi.org/10.5694/j.1326-5377.2009.tb02471.x.
Harvey JN, Lawson VL. The importance of health belief models in determining self-care behavior in diabetes. Diabetes Med. 2009;26(1):5–13. https://doi.org/10.1111/j.1464-5491.2008.02628.x.
Gregg JA, Callaghan GM, Hayes SC, Glenn-lawson JL. Improving diabetes self-management through acceptance, mindfulness, and values: a randomized controlled trial. J Consult Clin Psychol. 2007;75(2):336–43. https://doi.org/10.1037/0022-006x.75.2.336.
Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain and illness. Delacorte; 1990.
Cayoun BA. Mindfulness-integrated CBT for well-being and personal growth. Chichester: Wiley; 2015.
Grossman P. Mindfulness for psychologists: paying kind attention to perceptible. Mindfulness. 2010;1:87–97. https://doi.org/10.1007/s12671-010-0012-7.
Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4(1):33–47. https://doi.org/10.1016/0163-8343(82)90026-3.
Bishop RS, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Segal Z, Abbey S, Speca M, Velting D, Devins G. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract. 2006;11(3):125–43. https://doi.org/10.1093/clipsy/bph077.
Didonna F. Clinical handbook of mindfulness. Berlin: Springer; 2009.
Feldman G, Lavallee J, Gildaweie K, Greeson JM. Dispositional mindfulness uncouples physiological and emotional reactivity to a laboratory stressor and emotional reactivity to executive functioning lapses in daily life. Mindfulness. 2016;7:527–41. https://doi.org/10.1007/s12671-015-0487-3.
Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol. 2010;78(2):169–83. https://doi.org/10.1037/a0018555.
Segal ZV, Williams JMG, Teasdale JD. Mindfulness–based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford Press; 2002.
Rosenzweig S, Reibel D, Greeson J, Edman J, Jasser S, McMearty K, Goldstien BJ. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a Pilot Study. Altern Ther Health Med. 2007;13:36–8.
Son JV, Nyklíček I, Pop VJ, Blonk MC, Erdtieck RJ, Spooren PF, Toorians AW, Pouwer F. The effects of a mindfulness-based intervention on emotional distress, quality of life, and HbA1c in outpatients with diabetes (DiaMind): a randomized controlled trial. Diabetes Care. 2013;36(4):823–30. https://doi.org/10.2337/dc12-1477.
Tovote KA, Fleer J, Snippe E, Bas IV, Links TP, Emmelkamp PM, Sanderman R, Schroevers M. Cognitive behavioral therapy and mindfulness-based cognitive therapy for depressive symptoms in patients with diabetes: design of a randomized controlled trial. BioMedCentral Psychology. 2013;1:17.
Sheibani KA, Alipor A, Poursharifi H, Zare. The impact of mindfulness based cognitive therapy (MBCT) on mental and physical well-being indicators in patients with type 2 diabetes. Zahedan J Res Med Sci. 2013;16(10):19–23.
Nyklíček I, van Son J, Pop VJ, Denollet J, Pouwer F. Does Mindfulness-Based Cognitive Therapy benefit all people with diabetes and comorbid emotional complaints equally? Moderators in the DiaMind trial. J Psychosom Res. 2016;91:40–7. https://doi.org/10.1016/j.jpsychores.2016.10.009.
Tovote KA, Fleer J, Snippe E, Peeters ACTM, Emmel-kamp PM, Robbert Sanderman R, Schroevers M. Individual mindfulness-based cognitive therapy and cognitive behavior therapy for treating depressive symptoms in patients with diabetes: results of a randomized controlled trial. Diabetes Care. 2014;37(9):2427–34. https://doi.org/10.2337/dc13-2918.
Schroevers MJ, Tovote KA, Keers JC, Links TP, Sanderman R, Fleer J. Individual mindfulness-based cognitive therapy for people with diabetes: a pilot randomized controlled trial. Mindfulness. 2015;6:99–110. https://doi.org/10.1007/s12671-013-0235-5.
Cayoun BA. Mindfulness-integrated CBT principles and practice. Chichester: Wiley; 2011.
Cayoun BA, Sauvage V, Van Impe M. A non-diagnosis-specific application of mindfulness-based cognitive-behaviour therapy: a pilot study. Annual report to The Hobart Clinic, Rokeby, TAS, Australia; 2004.
Francis S, Shawyer F, Cayoun B, Enticott J, Meadows G. Study protocol for a randomized control trial to investigate the effectiveness of an 8-week mindfulness-integrated cognitive behavior therapy (MiCBT) transdiagnostic group intervention for primary care patients. BMC Psychiatry. 2020;20:7. https://doi.org/10.1186/s12888-019-2411-1.
Cayoun BA, Shires AG. Co-emergence reinforcement and its relevance to interoceptive desensitization in mindfulness and therapies aiming at transdiagnostic efficacy. Front Psychol. 2020;11: 545945. https://doi.org/10.3389/fpsyg.2020.545945.
Khalsa SS, Adolphs R, Cameron OG, the Interoception Summit 2016 participants. Interoception and mental health: a roadmap. Biol Psychiatry Cognit Neurosci Neuroimaging. 2018;3(6):501–13. https://doi.org/10.1016/j.bpsc.2017.12.004.
Greeson J, Garland EL, Black D. Mindfulness: a transtherapeutic approach for transdiagnostic mental processes. In: Ie A, Ngnoumen CT, Langer EJ, editors. The Wiley-Blackwell handbook of mindfulness. 1st ed. Hoboken: Wiley; 2014. p. 533–62.
Cayoun BA, Francis SE, Shires AG. The clinical handbook of mindfulness-integrated cognitive behavior therapy: a step-by-step guide for therapists. Hoboken: Wiley; 2019.
Yazdanimehr R, Omidi A, Sadat Z, Akbari H. The effect of mindfulness-integrated cognitive behavior therapy on depression and anxiety among pregnant women: a randomized clinical trial. J Caring Sci. 2016;5(3):195–204. https://doi.org/10.15171/jcs.2016.021.
Bahrani S, Zargar F, Yousefipour G, Akbari H. The effectiveness of mindfulness-integrated cognitive behavior therapy on depression, anxiety, and stress in females with multiple sclerosis: a single blind randomized controlled trial. Iran Red Crescent Med J. 2017;19(4):e44566. https://doi.org/10.5812/ircmj.44566.
Derakhtkar A, Khezrimoghadam N, Fazilat-Pour M, Cayoun BA. The Effectiveness of Mindfulness-integrated Cognitive Behavioral Therapy (MiCBT), meta-cognitive therapy, acceptance and commitment therapy, and cognitive behavioral therapy on obsessive-compulsive disorder. Int J Health Stud. 2021. https://doi.org/10.22100/ijhs.v8i2.876.
Mozafari-Motlagh MR, Nejat H, Tozandehjani H, Samari AA. Effect of cognitive behavior therapy integrated with mindfulness on perceived pain and pain self-efficacy in patients with breast cancer. J Nurs Midwifery Sci. 2019;6(2):51–6. https://doi.org/10.4103/JNMS.JNMS_60_18.
Pouyanfard S, Mohammadpour M, Parvizifard A, Foroughi A. The effectiveness of mindfulness-integrated cognitive-behavioral therapy on sleep quality, anxiety, and fatigue in patients with multiple sclerosis: a randomized clinical trial. J Sleep Sci 2019;4(1–2):1–8. https://jss.tums.ac.ir/index.php/jss/article/view/140
Pouyanfard S, Parvizifard A, Mohammadpour M, Sadeghi K. Effectiveness of mindfulness-integrated cognitive behavior therapy on anxiety, depression and hope in multiple sclerosis patients: a randomized clinical trial. Trends Psychiatry Psychother. 2020;42(1):55–63. https://doi.org/10.1590/2237-6089-2018-0105.
Wang L, Zhang M, Zhu H, Sun L, Yu B, Cui X. Combined identification of lncRNA NONHSAG004550 and NONHSAT125420 as a potential diagnostic biomarker of perinatal depression. J Clin Lab Anal. 2021;35(8): e23890. https://doi.org/10.1002/jcla.23890.
Scott-Hamilton J, Schutte NS, Brown RF. Effects of a mindfulness intervention on sports-anxiety, pessimism, and flow in competitive cyclists. Appl Psychol Health Well Being. 2016;8(1):85–103. https://doi.org/10.1111/aphw.12063.
Cayoun BA, Simmons A, Shires A. Immediate and lasting chronic pain reduction following a brief self-implemented mindfulness-based interoceptive exposure task: a pilot study. Mindfulness. 2020;11(1):112–24. https://doi.org/10.1007/s12671-017-0823-x.
Shires A, Sharpe L, Newton-John TRO. The relative efficacy of mindfulness versus distraction: the moderating role of attentional bias. Eur J Pain. 2018;23(4):1–12. https://doi.org/10.1002/ejp.1340.
Ayoubi J, Bigdeli I, Mashhadi A. The effect of Mindfulness-integrated Cognitive Behavior Therapy on quality of life, psychological distress and adherence in patients with type 2 Diabetes Mellitus. Q J Health Psychol. 2020;9(34):75–94. https://doi.org/10.30473/HPJ.2020.48322.4533.
Viinamäki H, Tanskanen A, Honkalampi K, Koivumaa-Honkanen H, Haatainen K, Kaustio O, Hintikka J. Is the Beck Depression Inventory suitable for screening major depression in different phases of the disease? Nord J Psychiatry. 2004;58(1):49–53. https://doi.org/10.1080/08039480310000798.
Lachin JM. Statistical considerations in the intent-to-treat principle. Control Clin Trials. 2000;21(3):167–89. https://doi.org/10.1016/S0197-2456(00)00046-5.
Cayoun BA. Mindfulness training: a complete step-by-step training in mindfulness meditation. [Audio recording of practice instructions] MiCBT Institute; 2004/2015. https://www.mindfulness.net.au
Beck AT, Steer RN, Garbing MG. Psychometric properties of the beck depression inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8(1):77–100. https://doi.org/10.1016/0272-7358(88)90050-5.
Stefan-Dabson K, Mohammadkhani P, Massah-Choulabi O. Psychometrics characteristic of Beck Depression Inventory-II in patients with major depressive disorder. Arch Rehabil. 2007;8:82–80 (In Persian).
Safren SA, Gonzalez JS, Soroudi N. Coping with chronic illness: cognitive behavioral therapy for adherence and depression in individuals with chronic illness. Workbook: Oxford University Press; 2008.
Fakhraei S, Sohrabi A, Rezaie F. Effectiveness of cognitive behavior therapy for depression and adherence (CBT-AD) in HIV-infected individuals receiving ART and MMT. [Unpublished Master’s Thesis] The University of Kurdistan, Sanandaj, Iran; 2013.
Hart W. The art of living: Vipassana meditation as taught by S. N. Goenka. Harper Collins; 1987.
Rogers HT, Shires AG, Cayoun BA. Development and validation of the equanimity Scale-16. Mindfulness. 2020. https://doi.org/10.1007/s12671-020-01503-6.
Desbordes G, Gard T, Hoge EA, Hölzel BK, Kerr C, Lazar SW, Olendzki A, Vago DR. Moving beyond mindfulness: defining equanimity as an outcome measure in meditation and contemplative research. Mindfulness. 2015;6:356–72. https://doi.org/10.1007/s12671-013-0269-8.
Cohen J. Statistical power analysis for the behavioural sciences. 2nd ed. Mahwah: Lawrence Erlbaum; 1988.
Renn BN, Obetz V, Feliciano L. Comorbidity of depressive symptoms among primary care patients with diabetes in a federally qualified health center. J Health Psychol. 2020;25(9):1303–9. https://doi.org/10.1177/1359105318755260.
Mohamadi M, Mohaqeqi Kamal SH, Vameghi M, Rafiey H, Setareh Forouzan A, Sajjadi H. A meta-analysis of studies related prevalence of depression in Iran. J Res Health. 2017;7(1):581–93.
Ko SH, Park SA, Cho JH, Ko SH, Shin KM, Lee SH, Song KH, Park YM, Ahn YB. Influence of the duration of diabetes on the outcome of a diabetes self-management education program. Diabetes Metab J. 2012;36(3):222–9. https://doi.org/10.4093/dmj.2012.36.3.222.
Huberty J, Green J, Glissmann C, Larkey L, Puzia M, Lee C. Efficacy of the mindfulness meditation mobile app “Calm” to reduce stress among college students: Randomized controlled trial. JMIR Mhealth Uhealth. 2019;7(6): e14273. https://doi.org/10.2196/14273.
Skinner BF. Science and human behavior. New York: The Free Press; 1953.
Tang Y, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. 2015;16:213–25. https://doi.org/10.1038/nrn3916.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
FS: executed the study, analyzed the data and co-wrote the paper. AS and NSA: co-designed the study and collaborated with the procedure and data acquisition. BC: Co-wrote the manuscript and collaborated with the editing of the manuscript. All authors approved the final version of the manuscript for submission. This study was a part of a Master of Science dissertation in clinical psychology at the University of Kurdistan, Iran. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The procedures used in this study adhere to the tenets of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was approved by the Human Research Ethics Committee of the Kurdistan University of Medical Sciences, Sanandaj, Iran (Ref. IR.UOK.REC.1398.044).
Consent to participate
Participants were fully informed of the procedure and aims of the study and gave their consent to participate.
Competing interests
The authors declare that they have no competing interest. The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: Summary of theoretical conceptualization of Mindfulness-integrated Cognitive Behavior Therapy (MiCBT)
Mindfulness-integrated Cognitive Behavior Therapy (MiCBT) is a transdiagnostic therapy approach that integrates mindfulness meditation with core elements of cognitive and behavioral methods for the purpose of teaching clients to cultivate experiential awareness and equanimity in order to regulate emotion and attention, and externalize these skills to the contexts in which their impairment is triggered or maintained [45]. The co-emergence model of reinforcement (CMR) [39, 42], is the main theoretical foundation of MiCBT. It also constitutes an important rationale for the mindfulness meditation (Vipassana) practices used in MiCBT, described in detail in Appendix 2. To preserve economy and facilitate accessibility of concepts, this appendix merely describes the CMR’s mechanisms in plain English and omits cumbersome scientific references. A comprehensive multidisciplinary review of empirical evidence can be found in the open access paper from Cayoun and Shires [42].
The CMR is a metatheory of behavior reinforcement. It emphasizes the neurophenomenology of experience by integrating central elements of cognitive and affective neuroscience, learning theory, schema theory and the “five aggregates of body and mind” known as the fundamental information processing components of human experience in Buddhist psychology. By providing a neurophenomenological account of the interaction between cognition and interoception, and its consequences on behavior, the CMR is better equipped than the traditional operant conditioning approach to explain behavior maintenance and change, including with psychopathology.
The traditional assumption of operant conditioning implies that learning takes place when the behavior ‘operates’ on the environment to generate consequences [72]. Behavior is either increased or decreased depending on the resulting consequence of the behavior on the stimulus. If the behavior leads to a desired outcome (rewarding consequence), the frequency of the behavior is likely to increase. If the behavior leads to an undesired outcome (non-rewarding or aversive consequence), the frequency of the behavior is likely to decrease. This conceptualization gives minimal, if any, consideration for the role that internal contexts, such as cognition and interoception, may have in guiding behavior.
In contrast, the CMR (Fig.
1) suggests that we react emotionally (response) because of the sensations we feel in the body (co-emergent interoception) that co-emerge with our conscious or subconscious evaluation (evaluation) of an external situation or internal experience (stimulus). We do not directly react to stimuli, which in the CMR are mere triggers that enter into contact through the senses to stimulate our memory of meaning or ‘category’ of experience. Once a potential trigger has been evaluated as agreeable/good or disagreeable/bad based on evaluative filters (including autobiographical memories, personality trait, needs, values, mood, beliefs/schemas, culture and expectations), sensations co-emerge in the body to drive a response. In short, we react in the way that we do because of what we feel, not because of the nature or state of the stimulus, and what we feel depends on our habitual judgement (evaluation). Importantly, greater self-referential processing in the brain’s medial prefrontal cortex activates stronger interoceptive signals in the brain’s insular cortex. In other words, the more we take a situation personally (i.e., the more activated is the “I”, “my”, “me”, “we”, “ours”), the more intense is the body sensation, which in turn increases the probability of a reaction.
It is also noteworthy that, unless specifically trained to process information differently (e.g., through mindfulness training), we ‘live in the past’ every time we become emotionally reactive, even indiscernibly. Once a reaction (response) takes place, the consequence is perceived through sensory pathways and fed forward for further evaluation. If the reaction produced the desired outcome, the memory of the response is reinforced. For example, negative reinforcement takes place when an unpleasant sensation decreases after avoiding the discomfort of exercising. Similarly, positive reinforcement takes place when pleasant sensations increase after eating pleasant food or feeling pleasantly intoxicated. This is obvious, for instance, when a person with social anxiety ‘forgets’ their fear after drinking alcohol, even though the avoidant response may have been reinforced for many years. Unless the person experiences fear-related unpleasant body sensation, the response is no longer driven by conditioned memory and they enjoy socializing or performing in public. In this particular example, alcohol prevents the memory re-consolidation mechanism of fear, similarly to the effect of a betablocker such as propranolol.
In the above description, both the structure and process of the mechanism are stable, in equilibrium state. This implies that all components and their brain corelates communicate more or less harmoniously between themselves. However, when situation is evaluated as being personally important and the event is distressing, the system is shifted to a momentary functional disequilibrium. Figure
2 shows a disequilibrium state occurring for a person with type 2 Diabetes Mellitus (DM) with poor adherence to self-care. Attention resources are depleted from sensory pathways (sensory perception and co-emergent interoception) and reallocated to the cognitive (evaluation) and behavioral (response) components of the information system. As a result, one becomes momentarily over-judgmental and over-reactive at the cost of sensitivity and objectivity (e.g., it is difficult to feel a mosquito bite while we are being chased by a grizzly bear). This is pictorially represented in Fig. 2 by larger boxes for inflated components and smaller ones for deflated components.
Sufficient systemic flexibility, subserved by executive functions, allows rapid return to a functional equilibrium between components after a reaction has occurred. However, if disequilibrium has been sufficiently sustained over time to produce brain reorganization, it becomes learned and is the stable state of the system. As a result of learned disequilibrium, one remains overly judgmental and reactive, leading to dysfunctional behavior. The CMR assigns chronic conditions and personality disorders to learned disequilibrium. Whatever modalities appear to reinforce a behavior (social/observational learning, operant or classical conditioning), all depend on the underlying interoceptive reinforcement described above. Since emotional events are encoded and retrieved from memory in a co-emergent manner, behavior which is not actively reinforced through exposure to a stimulus can still be maintained. This is the case for avoidant behavior. The sheer memory of being exposed to the avoided situation co-emerges with unpleasant body sensations, which in turn reconsolidates the aversive memory and reinforces avoidance. Unless some amount of interoceptive desensitization occurs, reactive habits are difficult to change. This is the primary reason for integrating mindfulness with CBT.
During mindfulness meditation, practitioners are taught to prevent self-referential evaluation and reaction (reducing processing in evaluation and response components) when experiencing pleasant and unpleasant experiences. Instead, they learn not to identify with the experience and accept it on the basis that it is an impermanent and therefore impersonal phenomenon. They are also asked to pay careful attention to the sensory aspects of the experience (increase processing in sensory perception and co-emergent interoception). Hence, mindfulness meditation is an ideal means of recreating equilibrium state in the nervous system and reestablishing a sense of agency over undesired behavior, irrespective of the condition for which one seeks psychological assistance. This is the main reason for which mindfulness training produces transdiagnostic benefits. In MiCBT, mindfulness practice is tightly integrating with CBT skillsets to combine interoceptive and exteroceptive exposure to targeted contexts. With poor self-care related to type 2 DM, targeted contexts may be avoidance of exercise and craving unhelpful food, among others. As explained in Appendix 2, interoceptive awareness and desensitization are first cultivated during mindfulness meditation Stage 1 of MiCBT, and then implemented in contexts of situational avoidance and interpersonal reactivity to improve the capacity to maintain an equilibrium state across contexts.
Appendix 2: Step-by-step delivery of stages 1 and 2 of MiCBT with verbatim instructions
MiCBT is composed of learning stages grouped into ‘internalizing’ and ‘externalizing’ phases that enable change across various life domains. The purpose of this hierarchical integration is first to teach clients to internalize attention in order to regulate attention and emotion, and then externalize these skills to the contexts in which their psychological condition is triggered or maintained. The descriptions below include sections explaining (1) the structure, (2) the related skillsets, (3) their rationale offered to patients, and (4) their related instructions using verbatim dialogue. As per CBT clinical interventions, we commence the teaching of each skillset by offering the patient a psychoeducational rationale to help promote an initial understanding of the task, commitment to doing it, and therapeutic alliance. The descriptions below also include instructional features that we believe are relevant to using MiCBT with type 2 DM. These would change according to the presenting condition for which the patient seeks assistance. In the verbatim dialogues below, ‘T’ = therapist and ‘P’ = patient. Also, ‘…’ means short silence, “… …” means longer silence, and italics are used to indicate words that are emphasized.
2.1 Stage 1: ‘Personal Stage’ (attention and emotion regulation)
2.1.1 Purpose
During the first stage of MiCBT, participants were taught to develop three mindfulness skillsets to improve their ability to regulate attention and emotions. These are also standard steps in the traditional teaching of Vipassana meditation in the Burmese tradition of Ledi Sayadaw, U Ba Khin, and Goenka [64]. Although beneficial in themselves, these self-regulation skills are integrated in subsequent stages to build exposure methods that are applicable across a wide range of diagnoses and symptoms.
2.1.2 Attention regulation
Regulation of attention through ‘mindfulness of breath’ (MOB) requires perceiving.
each thought only as ‘a thought’, a mental process, regardless of its content, in order to develop meta-cognitive awareness while preventing automatic identification with thoughts. This practice requires core cognitive mechanisms involved in sustained attention, response inhibition and attention shifting [27, 39]. In MiCBT, MOB is principally used to increase one’s capacity to remain attentive of a chosen object of concentration, partly as a prerequisite for developing emotion-regulation skills, which necessitate a sufficient degree of concentration. However, by practicing MOB and applying metacognitive awareness and acceptance in day-to-day experiences, patients also derive a sense of agency over the process of thinking and a sense of self-efficacy in preventing the proliferation of unhelpful thoughts in daily life.
2.1.2.1 Delivery of the rationale and practice instructions
The following is an actual interaction with a patient with major depression with anxious distress and type 2 DM. This is a typical introduction to MOB in therapy session, occasionally using Socratic dialoguing, taking into account that Persian expressions may differ from English ones, partly due to cultural differences. MiCBT practitioners use a method called ‘the finger task’ to deliver the rationale for MOB in an experiential way. This served both to educate the patient through direct experience, and to verify that they have understood the task before practicing it at home. The same instructions were given in Persian (with slight variance in expressions) to each participant during individual therapy sessions. Each participant was first explained how and why to sit comfortably on a chair or on the floor with their neck and back straight, without leaning against anything, unless they had a medical condition which required back or neck support:
T. If that’s ok with you, in a few minutes I will guide you through a short practice called ‘mindfulness of the breath’. It is a simple training of attention which helps people to accept their thoughts and let them pass more quickly. People also understand better the way their mind works, and they usually become more comfortable with their experiences of overthinking things or worrying. How does that sound?
P. This sounds good, but what if I can’t concentrate?
T. This will not be a problem. On the contrary, we can adjust the practice and use your experience to develop a better ability to accept your experience just as it is.
P. And will that help?
T. More often than not, yes it helps.
P. Sure, I’m happy to try.
T. Great. If you are ready to start, take a comfortable posture, sitting with your neck and back straight... For this particular exercise today, please place your hands face down on your thighs to practice what we call the finger task. It’s very simple and it will help me see if I have explained everything correctly. This is just for today and you won’t need to do this at home. In a minute, I will ask you to close your eyes and focus your attention on your breath for as long as you can. Of course, within seconds it is likely that a thought, a sound or an image will pop up in your mind. This is absolutely normal and expected. The first skill you will need to develop is simply to detect it, just recognize that thinking has taken place, and that this is just a thought that doesn’t define who you are.
P. What do your mean?
T. Let’s take the example of dreams. Do you have weird dreams sometimes?
P. Oh yeah, very often.
T. Right, and does it mean that because the thoughts of a dream are weird it makes you a weird person?
P. No, not at all.
T. So is it possible that we can have thoughts that don’t necessarily reflect who we are when we are awake?
P. Sure, I get what you mean now.
T. Ok, so that’s the first skill, just recognizing a thought for what it is, just a thought. Then, as soon as you noticed a thought, accept that it is there and resist the habit of thinking it. It’s a kind of “thanks but no thanks” attitude. This is where you exercise your free will; the choice to think or not to think, irrespective of the type of thought. Do you think a person that is not able to choose their thoughts can truly say that they have ‘free-will’, whoever they are?...
P. Not at all! I think they are more a prisoner of their mind, like me sometimes.
T. True, we are more often than not like a slave of our own thoughts, but we can free our mind with training. So, this is the second skill, you ‘inhibit’ the usual response of the mind to engage with a thought just because it arises in the mind. And the third skill is to literally abandon the thought, to put down and gently return to the breath without delay; without clinging to it and without impatience or frustration. We shift attention back to the task at hand, which during this practice is to pay attention to the breath. We only use the breath to anchor attention on the body, but the most important things about the practice are the skills we use once a thought comes in the mind. Basically, we develop three important skills called ‘executive functions’ with the front of our brain, first to stay aware of arising thoughts that we didn’t choose to have, then prevent the habit of thinking it further, and immediately refocus on the task that you chose to do in the first place, which is to monitor your breath. Are you ready to try?
P. Sure!
T. Ok, so please gently close your eyes, as this will prevent being too distracted by what is around you and gently re-place the palm of the hands on your thighs. Now you will indicate when you are using the three skills that I just mentioned using the index finger of your dominant hand. Can you show me the one I’m talking about?... Great! Every time you notice a thought arising in the mind, gently raise this finger and keep it raise to show me that you are in the process of disengaging from the thought, and then re-place you finger back on your thigh to show me that your full attention is now refocused on the breath. Is everything clear? Can you repeat what you are going to do just in case I need to clarify something?... Ok, now focus all your attention, all your attention on the breath at the entrance of the nostrils. You may feel a sensation of the breath touching the inner walls of the nostrils, the outer rings of the nostrils, or the area below the nostrils above the upper lip...It is important that you control your attention, but not the breath. It must be normal, natural, breath, just as you need to breathe from moment to moment...just remain aware of is happening right now at the entrance of your nostrils... Now I let you practice in silence for a minute, using your finger to show the three skills. Remember to accept thoughts when they arise and to return to the breath very patiently... ...
T. Excellent! In your own time, please open your eyes.
P. Wow! This was hard!
T. Yes, very hard to start with because parts of your frontal lobe are working hard in a way that they are not used to. It’s a bit like going to the gym for the first time. It can hurt a little for the first few days and then it becomes much easier. Does that make sense?
P. Yes totally.
T. Do you think that this practice could be helpful when you have unwanted or even destructive thoughts?
P. Yes, I can see how this could help me letting them go and be more productive.
T. Yes, because of the daily training, every day you become a little more able to apply the three executive functions I mentioned earlier into your daily activities. For example, you mentioned that you ruminate when you are not busy, so you drink alcohol or you eat bad food to avoid it. Do you think that catching these thoughts as soon as they pop up, not engaging with them, and refocusing on what you are doing could help?
P. Wow, it would be brilliant if I could do this!
T. Well, all you need to do is to commit to practicing it for 30 minutes twice daily, as we agreed last week when we did the therapy contract. When would you like to start?
Note that the entire explanation is free from cultural loading and unless a person asked about the origins of the practice no references to Buddhism were made to prevent potential fear or dilemmas related to religious matters. This applies to patients affiliated to other religions, who reported in the past being afraid of emptying their mind and letting in evil spirits. Accordingly, Buddhist terminology, such as ‘emptiness’ is not used, even though MiCBT adheres closely to the traditional practice of mindfulness skills.
2.1.3 Emotion regulation
The next skillset of Stage 1 practice serves to assist in regulating emotions, which is principally enhanced by improving interoceptive awareness and equanimity through ‘body-scanning’ (BS) techniques. Once the patient is able to focus on the breath without interruption for at least 30 s, they are ready for BS. The approximate 30-s cut-off is based on the requirement to focus for about 30 s on ‘blank spots’ (absence of conscious body sensations) in various body parts during BS. If it is not possible to stay focused on a dynamic target such as the breath for this duration, it will be too difficult to do so on a static target such as a shoulder or an elbow. The decision to transition from MOB to BS after one week is guided by both the manualized procedure and the patient’s capacity to sustain attention sufficiently, which is more often than not a function of their adherence to practice frequency, duration and accuracy. If the patient needs more time to develop MOB skills sufficiently, the therapist suggests extending MOB for a few days, after verifying MOB practice and occasionally modifying its duration or frequency when needed (e.g., with moderate ADHD comorbidity, suggesting four 15-min instead of two 30-min practices daily).
For BS, participants surveyed the body part by part, continuously and systematically in a bi-directional vertical order, in increasingly subtle ways while learning to experience body sensations “just as body sensations” and preventing automatic reactions (i.e., equanimously). They also witnessed the transient and co-emerging nature of thoughts and body sensations that underlie emotions and learned not to identify with them. Body-scanning methods may be operationalized behaviorally as an interoceptive desensitization method which involves a systematic exposure to body sensations and the prevention of the prepotent (learned) response. Progress with this practice allows the detection of early distress cues which emerge spontaneously in interoception and helps to inhibit learned maladaptive responses (see Appendix 1 for detail).
The third step of Stage 1 requires externalizing equanimity by applying the above skills in daily situations. Once a degree of equanimity was developed through exposure to internal cues during mindfulness meditation, participants were asked to remain aware of body-sensations throughout the day and apply equanimity in distressing situations or situations in which craving (e.g., unhealthy food) occurs.
2.1.3.1 Delivery of the rationale
The rationale for BS can be delivered experientially and/or in a psychoeducational manner. A full description with verbatim dialogue for the experiential delivery can be found in Cayoun et al. [45] and is beyond the scope of this paper. Below is a description of a typical Socratic dialogue used to offer the psychoeducational rationale for BS in MiCBT. The same approach was used in the current study, with slight variances in the Persian translation:
T. It sounds like you are ready to take the next step. Congratulation! Now we will begin with learning to regulate emotions by learning to survey each part of the body with an accepting and non-reactive attitude. You must be wondering how surveying your little finger can help you manage your emotions, right?
P. Yes, I wonder how this works.
T. Well, do you feel angry sometimes?
P. Yes, of course, I can get pretty angry, especially with myself!
T. When you feel the anger, how do you that you’re feeling it?
P. I usually slam a door, or I can even shout at the kids.
T. That’s the behavior; the thing that you do to feel better about how you feel, but before you react like this, how do you know that you are feeling anger, and not joy, for example.
P. I feel very agitated and hot.
T. Yes! Most people feel some heat and movement in the body, which can be caused by increased heart rate or trembling and the need to move, right?
P. Yes, that’s how it feels.
T. So you know that you feel the anger through your body, right? And do you feel anxious sometimes?
P. Yes, most of the time; this is also why I’m here.
T. When you feel the fear or anxiety, how do you know you are feeling it?
P. There’s also an agitation in my body but I feel compressed and tight in the chest and I have butterflies in the stomach when it’s bad.
T. So you know that you feel anxiety through your body as well, right?
P. Yes.
T. And what about sadness? Do you feel sad sometime?
P. Oh yes, way too often, I can cry just watching TV at the moment. My doctor told me this is because I’m depressed.
T. And how do you know that you are feeling sad when you are feeling it?
P. This I’m not sure; I cry?
T. Sure, crying is your reaction to how you feel, but can you remember how it actually feels to feel sad? Do you feel light and bubbly?
P. Not at all. I feel tired, no energy and no motivation.
T. And how do you know that you’re feeling tired and without energy?
P. I feel kind of heavy.
T. Yes! Heaviness is the hallmark of sadness!... So, whether you feel angry, anxious or sad, the only real way of knowing it is through feeling sensations in the body, correct?
P. Yes, I never thought about this, but it makes sense.
T. This is what scientists who specialize in emotion research have found too. The only way an emotion feels real to us is through feeling body sensations, which we call the ‘building block’ of emotions. If we can’t feel body sensations, we cannot truly feel an emotion. We may be dissociated from the body due to anxiety or stress and we cannot recognize what we are feeling.
P. Yes, sometime this happens to me; I feel like I walk on cottonwool.
T. That’s right. So, given that all emotions are made of body sensations, what do think could happen if you learn to feel sensations in every part of the body, by ‘scanning’ the body systematically from head to toe and toe to head, feeling, accepting, and moving to the next part, twice daily, day after day, and week after week in different ways, so that progressively all body sensation, including those caused by emotions, become acceptable. If all emotions are made of body sensations and all body sensations have become acceptable, what will it be like when you feel angry, anxious or sad?
P. I think I’ll be more ok with my emotion?
T. Do you mean they will feel more acceptable to you?
P. Yes, that’s what I mean. I’ll be able to cruise through them!
T. This sounds good. Would you like to learn this skill?
P. Absolutely! I need it.
Then the therapist provides the practice instructions and reiterates the importance of maintaining a commitment to sufficient practice frequency, duration and accuracy in order to develop adequate interoceptive awareness and equanimity, which will be ‘invested’ in Stage 2 to facilitate exposure tasks. Here too, the entire explanation is free from cultural loading and no references to Buddhism were made to prevent potential fear or dilemmas related to religious matters, as mentioned above. If a person asks if this is a Buddhist method, the therapist explains that meditation has been used by many contemplative traditions, and in our therapy context, we are only focusing on the science of interoceptive attention and equanimity and their positive effects on the brain and behavior. Religion and culture are separate issues, and anyone, of any religion, can achieve the same positive results.
2.1.3.2 Practice explanation and instructions
Basic explanation of co-emergence When something seems important to us, it automatically creates some sensations inside the body, and when the sensations are intense enough, we perceive them as feelings or emotions. For example, if you have the thought that you are not successful at losing weight or exercising, you may be able to notice some discomfort somewhere in the body. Some changes happen, even small ones that we normally don’t pay attention to. Even if you are not aware of these changes, they affect how you feel and react. When we have a negative or fearful thought, unpleasant sensations also arise in the body, such as a warm swirling movement in the stomach. We may react to these sensations by trying to avoid them. We may drink alcohol or coffee, smoke a cigarette, eat food, or distract our mind in other ways. This may mask the sensations and provide some relief for a short while, but it can also become a problem later. We begin to realize this connection between thoughts and feelings as we develop our mindfulness practice. We also understand that learning to pay attention to body sensations allows us to be aware of emotions more quickly and manage them more skillfully as soon as they arise. This week, the practice will involve sitting still with your neck and back straight, and focusing all your attention on the entire body, part by part, instead of just attending to the breath.
Basic instructions (After practicing MOB for about 2 minutes) Now focus all your attention at the top of your head, on the very top of your head and feel any possible sensation that may take place there, at the top of your head on a small area of about 6 to 8 centimeters diameter spot of attention... Body sensations are ordinary sensations, such as movement, an itching sensation, pressure, cold or heat, heaviness or lightness, tightness or looseness, tingling or prickling sensations, a sense of expansion or contraction, etc. There are infinite possibilities of sensations. Just as you prevented getting involved with the thoughts during MOB last week, here too, prevent getting involved with body sensations that you come across. Just observe them instead... This doesn’t mean visualize them or imagine them; it means do your best to feel whatever may be taking at the top of your head...We need to witness the ‘reality’ taking place in this part of the body as it occurs, from moment to moment, and as much as possible without affecting it or being affected by it. Simply witness what is happening... As soon as you notice a sensation of any sort, gently move your attention to the next area of about the same size, without attachment or avoidance, without evaluating the sensation as good or bad, acceptable or unacceptable... ... Even if nothing seems to be happening on this part of the body, simply be aware of this, patiently, equanimously, which means without any reaction and with an accepting attitude toward your experience... After all, this is also an experience. It is the reality that you experience at this time, on this part of the body... After about half a minute, if no sensation has been felt, on this part, move to next part of about the same size and do the same, calmly and equanimously... ... In this way, survey the entire body systematically, from the top of the head to the tip of the toes, part by part, and when you reach the toes, return in the same way back up to the top of the head, developing your awareness of sensations and equanimity with each part of the body... ... Learn to prevent craving and aversion with each body part. Make sure that you accept not feeling any sensation on certain parts. This is normal when we start this practice, but this will also change...
So far, with Stage 1 of MiCBT, participants developed metacognitive and interoceptive awareness, along with equanimity, both during meditation practice and in daily life. They learned to regulate emotions by becoming aware of body sensations in a non-reactive manner. In this way, they also learned how to extinguish their conditioned responses to internal triggers by inhibiting their usual responses to thoughts and co-emerging body sensations. In other words, they have been learning to desensitize unhelpful emotions by focusing initially internally from week 1 to week 3, and then started to apply their emotion-regulating skills externally in week 4. They are now ready to apply their skills in external contexts for the purpose of regulating behavior in challenging situations, where avoidance may maintain the problems which they are trying to resolve.
2.2 Stage 2: ‘Exposure stage’ (behavioral regulation)
2.2.1 Purpose
At the start of Stage 2, patients are taught the first advanced body-scanning technique, ‘symmetrical scanning’. This consists of the same part-by-part scanning method used in Stage 1, but attention is passed on both sides of the midline of the body simultaneously and symmetrically. This bilateral scanning method engages the somatosensory and insular cortices of both hemispheres simultaneously, allowing more rapid and frequent cycling of attention through the body. As a consequence, interoceptive awareness improves more rapidly. In daily life, this wider scope of interoceptive awareness also improves the detection of early distress cues and the application of equanimity at an earlier point of the emergence of emotions. In Stage 2, participants began to use mindfulness skills to manage their fears and build self-confidence. A brief explanation of what constitutes avoidance and a rationale for Stage 2 were provided. It was explained that unhelpful avoidance, whichever form it takes, is an important contributor to maladaptive behavior and deprives people from enjoying a fuller life, such as taking the risk to change for the better.
Whereas the purpose of traditional exposure therapy is to reduce avoidance of certain triggers or situations, the exposure methods in MiCBT use a combination of interoceptive and exteroceptive desensitization to produce a ‘less fearful brain’, so to speak, across all feared situations. This is partly done by reducing the size of the right basolateral amygdala and the resulting activation of stress hormones through mindfulness practice during Stage 1 [73], and partly by placing the less reactive person in various contexts of previously feared stimuli. We observe during the two weeks of Stage 2 that people’s fears decrease even to previously avoided situations to which they have not yet been exposed. Besides increasing one’s sense of self-efficacy of self-confidence, this ‘generalization of desensitization’ is helpful in reducing several types of avoidance with complex comorbidity. In the present study, all participants were typically avoidant of several contexts due to depression (social, chores, pleasurable activities, etc.), and avoidant of self-care behavior commonly associated with type 2 DM (exercising, maintaining a healthy diet, etc.). Using interoceptive exposure while also exposed to these particular contexts helped change behavior rapidly, hence the resulting reduced depression, increased adherence to self-care and medical treatment and reduced glycemic levels in the MiCBT group.
2.2.2 Structure of exposure
Prior to commencing exposure, participants wrote down a list of situations they commonly avoid and rate out of 10 each situation according to the expected level of distress that would occur if they were exposed to it. They then selected five of these situations that have an incremental level of distress (e.g., 2/10, 4/10, 5/10, 8/10, 9/10). They then started exposure to these five situations, one at a time. There are two types of exposure methods used in Stage 2: ‘bipolar exposure’ and ‘in vivo exposure’. Bipolar exposure (BPE) simply means being exposed to two extreme opposite experiences of the same situation (pleasant and unpleasant). BPE consists of a three-step exercise which lasts eleven minutes and is self-implemented immediately after every 30-min of mindfulness meditation. It requires using imagination to simulate various scenarios which the patient could come across in an avoided situation. This is done in four successive sessions, preferably over two days, before putting oneself into the situation in real life (in vivo exposure). Participants were asked to keep their eyes closed throughout the procedure to allow effective imagery. Below are the instructions given to them for each avoided situation listed on their ‘subjective units of distress’ form.
2.2.3 Instructions
-
1.
Let’s start with the first situation on your list: “exercising at home”. You will need to be sitting with your eyes closed. You will also need a way of timing the exercise. For the first five minutes, the task is to visualize one or more worst-case scenarios that could occur if you were not avoiding the situation and you were exercising at home. While visualizing and catastrophizing the event, do your best to remain equanimous, as you are when you meditate and feel an unpleasant body sensation. You need to imagine the worst that could happen when you will be in that situation in real life two days from now. At the same time, monitor the unpleasant sensations that these negative expectations create in your body and do your best to not react because of these sensations. Do your best also to not identify with them, and perceive them for what they are, just impermanent sensations in the body, as you do when scan the body during meditation. As you combine an imagined unpleasant experience with equanimity, the emotional aspect of your anticipated distress becomes neutralized because unpleasant sensations are now associated with acceptance and non-reactivity. Does this make sense? Do you have any questions at this point?
-
2.
After these first five minutes, have a break by switching your attention to the entrance of your nostrils for about one minute, and rest your mind on your breath while keeping your eyes closed. Let your mind relax as your breath settles. Later on, with more distressing situations on your list, you might need a longer break than one minute to regain a sufficiently relaxed mind before continuing to the next task. The 1-min duration is only a rough guide for less distressing items, but longer than 3 min may reduce the effect of exposure, so please dose what feels right for you. The more equanimous you are during the worst-case scenarios, the easier it is to relax afterward.
-
3.
For the last five minutes, you will need to switch your attention to the same situation, which is exercising at home, also while keeping your eyes closed, but this time visualizing one or more best-case scenarios that could realistically happen when you will be in this situation in real life, two days from now. While visualizing and embellishing the situation, do your best to remain equanimous, even though the situation is now pleasant. While you imagine the very best scenarios, some pleasant body sensations are likely to co-emerge with your imagination. Do their best to not react with attachment to these sensations, wanting more of them or wanting them to last longer because they are pleasant. Some people can be surprised by this procedure, sometimes wondering why it wouldn’t be useful to want pleasant scenarios. The problem with this view is that we would create a preference for a chosen outcome and become attached to it. As soon as we do this, we unintentionally decide that another type of outcome is not preferred or would even be unacceptable. We may resent it. Consequently, if the outcome is not what we prefer, we repeat the habit of craving what we don’t have and resenting what we have. For example, with the exercising scenario, you could imagine that you find exercising to be pleasant and very rewarding in itself, and that your family members are very supporting by letting you take all the time you need and praise you for your effort, and that you will feel very good about yourself. But what if none of this happens? If you develop attachment to your positive expectations but things don’t turn out the way you want, then you are likely to be disappointed and discouraged. It is the same in our lives when we don’t get what we want, but we are working on changing this habit. With bipolar exposure, we also extinguish the craving to avoid disappointment if the outcome is not according to our wishes. This is why you will train to remain equanimous and unattached with both pleasant and unpleasant experiences. Remember to prevent any personal judgment regarding body sensations, and observe them objectively, as passing events. When you practice in this way, you neutralize the usual craving response, rather than the aversive response. Do you think that this could also help you reduce your craving for unhealthy food?
After four practices of BPE, you will be ready for in vivo exposure, which means exposure in real life. After doing bipolar exposure to situation 1 on your list four time in the next two days, you can start exercising in real life, and on the same day start BPE to situation 2 on your list after each morning and evening meditation practice, which is “watching TV without eating any snacks”. In this way, one situation is being neutralized with imaginal exposure while the previous one your list is being experienced more equanimously in real life. Can you see how one task follows the other nicely for each targeted situation? You can proceed with this method until all the listed situations have been addressed and none of them remains a source of avoidance. Please take the time you need but try to keep up the momentum because it will help maintain your progress. People can usually complete bipolar and in-vivo exposure for two to three situations per week. Accordingly, the usual duration of Stage 2 is two weeks, but we can a bit more time if you need. When we meet again next week, we can review the level of distress for each situation that you listed and see if your anxiety has changed. Do you have any questions?
Baseline ratings of expected distress are usually reviewed weekly with the therapist. Note that while the procedure used in this study did not include the behavioral components of Stage 3 and 4, it did include their related scanning methods.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sohrabi, F., Sohrabi, A., Shams-Alizadeh, N. et al. Managing type 2 diabetes and depression with Mindfulness-integrated Cognitive Behavior Therapy (MiCBT). Discov Psychol 2, 10 (2022). https://doi.org/10.1007/s44202-022-00026-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44202-022-00026-6