Abstract
Background
Virtual Fracture Clinics (VFCs) are an alternative to the conventional model of fracture and minor injuries care. It is a new, evolving service designed to speed up patient access to orthopaedic care introduced in the United Kingdom in 2011 and has been increasingly used in the management of certain musculoskeletal injuries.
Methods
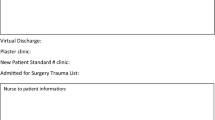
This observational, pilot study evaluates the possibility of combining telemedicine technology and a virtual fracture clinical assessment pathway to remotely assess patients supported by radiology imaging in India.
Results
Piloting and developing a virtual fracture clinical assessment pathway model in India is faced with many challenges including regulations, internet, and data connectivity issues, and concerns of medico-legal implications.
Conclusion
Recent studies have reported Virtual Fracture Clinics (VFCs) to be able to provide a safe, cost-effective model of patient care in a subset of musculoskeletal injuries. Limitations and shortcomings of Virtual Fracture Clinics (VFCs) in India can be mitigated with effective communication, enhanced documentation, appropriate training, and information governance. This pathway is not a replacement for conventional ‘face-to-face’ evaluation but a credible option to complement the delivery of trauma and orthopaedic care in the future in India.



Similar content being viewed by others
References
Iyengar, K., Vaish, A., Toh, E., & Vaishya, R. (2020). COVID-19 and remote consulting strategies in managing trauma and orthopaedics. Postgraduate Medical Journal, 96(1137), 438–439. https://doi.org/10.1136/postgradmedj-2020-137917
Greenhalgh, T., Vijayaraghavan, S., Wherton, J., Shaw, S., Byrne, E., Campbell-Richards, D., Bhattacharya, S., Hanson, P., Ramoutar, S., Gutteridge, C., Hodkinson, I., Collard, A., & Morris, J. (2016). Virtual online consultations: Advantages and limitations (VOCAL) study. British Medical Journal Open, 6(1), e009388. https://doi.org/10.1136/bmjopen-2015-009388
Logishetty, K. (2017). Adopting and sustaining a Virtual Fracture Clinic model in the District Hospital setting—A quality improvement approach. British Medical Journal Quality Improvement Reports, 6(1), u220211.w7861. https://doi.org/10.1136/bmjquality.u220211.w7861
Murphy, E. P., Fenelon, C., Murphy, R. P., O’Sullivan, M. D., Pomeroy, E., Sheehan, E., & Moore, D. P. (2020). Are virtual fracture clinics during the COVID-19 pandemic a potential alternative for delivering fracture care? A systematic review. Clinical Orthopaedics and Related Research, 478(11), 2610–2621. https://doi.org/10.1097/CORR.0000000000001388
Bellringer, S. F., Brogan, K., Cassidy, L., & Gibbs, J. (2017). Standardised virtual fracture clinic management of radiographically stable Weber B ankle fractures is safe, cost effective and reproducible. Injury, 48(7), 1670–1673. https://doi.org/10.1016/j.injury.2017.04.053
Robinson, P. M., Sim, F., Latimer, M., & Mitchell, P. D. (2017). Paediatric fracture clinic re-design: Incorporating a virtual fracture clinic. Injury, 48(10), 2101–2105. https://doi.org/10.1016/j.injury.2017.08.006
Jain, V. K., & Vaishya, R. (2020). COVID-19 and orthopaedic surgeons: The Indian scenario. Tropical Doctor, 50(2), 108–110. https://doi.org/10.1177/0049475520921616
Jain, A. K. (2016). Current state of orthopaedic education in India. Indian J Orthop, C50, 341–344. https://doi.org/10.4103/0019-5413.185586
Seewoonarain, S., Babu, S., Sangoi, D., Avasthi, A., & Ricketts, D. (2019). Introducing a virtual fracture clinic increases efficiency and reduces costs in torus fracture management. Pediatr Qual Saf., 4(6), e202. https://doi.org/10.1097/pq9.0000000000000202
Evans, D., Hardman, J., Middleton, S. D., & Anakwe, R. E. (2018). Developing a virtual fracture clinic for hand and wrist injuries. J Hand Surg Eur, 43(8), 893–894. https://doi.org/10.1177/1753193418778472
McKirdy, A., & Imbuldeniya, A. M. (2017). The clinical and cost effectiveness of a virtual fracture clinic service: An interrupted time series analysis and before-and-after comparison. Bone Joint Res., 6(5), 259–269. https://doi.org/10.1302/2046-3758.65.BJR-2017-0330.R1
British Orthopaedic Association. Legal aspects of virtual fracture clinics. Retrieved from https://www.boa.ac.uk/resources/medicolegalarticles/legal-aspects-of-virtual-fracture-clinics.html. 10 Oct 2020.
Vardy, J., Jenkins, P. J., Clark, K., Chekroud, M., Begbie, K., Anthony, I., Rymaszewski, L. A., & Ireland, A. J. (2014). Effect of a redesigned fracture management pathway and 'virtual' fracture clinic on ED performance. BMJ Open. 4(6), e005282. https://doi.org/10.1136/bmjopen-2014-005282.
Thelwall, C. (2021). A service evaluation after 4 year’s use of the virtual fracture clinic model by a district general hospital in the south west of England. Int J Orthop Trauma Nurs., 41, 100798. https://doi.org/10.1016/j.ijotn.2020.100798
Rhind, J. H., Ramhamadany, E., Collins, R., Govilkar, S., Dass, D., & Hay, S. (2020). An analysis of virtual fracture clinics in orthopaedic trauma in the UK during the coronavirus crisis. EFORT Open Rev., 5(7), 442–448. https://doi.org/10.1302/2058-5241.5.200041
Ministry of Health and Family Welfare, Government of India. Telemedicine practice guidelines. Retrieved from https://www.mohfw.gov.in/pdf/Telemedicine.pdf. Published 25 March 2020. 10 Oct 2020.
Government of India. E-Sanjeevani. Retrieved from https://esanjeevani.com/. 10 Oct 2020.
Ghosh, A., Gupta, R., & Misra, A. (2020). Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: Guidelines for physicians. Diabetes and Metabolic Syndrome: Clinical Research and Reviews, 14(4), 273–276. https://doi.org/10.1016/j.dsx.2020.04.001
Mayadevi, M., Thankappan, K., Limbachiya, S. V., et al. (2018). Interdisciplinary telemedicine in the management of dysphagia in head and neck. Dysphagia, 33(4), 474–480. https://doi.org/10.1007/s00455-018-9876-9
Lal, H., Sharma, D. K., Patralekh, M. K., Jain, V. K., & Maini, L. (2020). Out Patient Department practices in orthopaedics amidst COVID-19: The evolving model. J Clin Orthop Trauma., 11(4), 700–712. https://doi.org/10.1016/j.jcot.2020.05.009
Ghosh, A., Dutta, K., Tyagi, K., Gupta, R., & Misra, A. (2020). Roadblock in application of telemedicine for diabetes management in India during COVID19 pandemic. Diabetes and Metabolic Syndrome: Clinical Research and Reviews, 14(4), 577–578. https://doi.org/10.1016/j.dsx.2020.05.010
Iyengar, K., Upadhyaya, G. K., Vaishya, R., & Jain, V. (2020). COVID-19 and applications of smartphone technology in the current pandemic. Diabetes and Metabolic Syndrome: Clinical Research and Reviews, 14(5), 733–737. https://doi.org/10.1016/j.dsx.2020.05.033
Ministry of Electronics and Information Technology, Government of India. Retrieved from https://digitalindia.gov.in/. Accessed 10 Oct 2020.
General Medical Council. Good medical practice. (Updated 29 April 2019). Retrieved from https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice.
Iyengar, K., Jain, V. K., & Vaishya, R. (2020). Pitfalls in telemedicine consultations in the era of COVID 19 and how to avoid them. Diabetes and Metabolic Syndrome: Clinical Research and Reviews, 14(5), 797–799. https://doi.org/10.1016/j.dsx.2020.06.007
Funding
Nil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Iyengar, K.P., Jain, V.K., Nallakumarasamy, A. et al. Virtual Fracture Clinic Model in India: A Technological Innovation. JOIO 57, 1–6 (2023). https://doi.org/10.1007/s43465-022-00763-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-022-00763-9