Abstract
Purpose
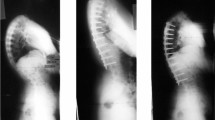
This study sought to investigate associations between upper instrumented vertebra (UIV) location and the risk of proximal junctional kyphosis (PJK) at 2 years following posterior spinal fusion (PSF) for Scheuermann’s kyphosis (SK).
Methods
In this retrospective cohort study, SK patients who underwent PSF and reached 2 years postop were identified in a multicenter international registry, excluding those with anterior release, prior spine surgery, neuromuscular comorbidity, post-traumatic kyphosis, or kyphosis apex below T11–T12. Location of UIV as well as the number of levels between UIV and preoperative kyphosis apex was determined. Additionally, the degree of kyphosis correction was evaluated. PJK was defined as a proximal junctional angle ≥ 10° that is ≥ 10° greater than the preoperative measurement.
Results
90 patients (16.5 ± 1.9 yo, 65.6% male) were included. Preoperative and 2-year postoperative major kyphosis was 74.6 ± 11.6° and 45.9 ± 10.5°, respectively. Twenty-two (24.4%) patients developed PJK at 2 years. Patients with UIV below T2 had a 2.09 times increased risk of PJK when compared to those with UIV at or above T2, adjusting for distance between UIV and preoperative kyphosis apex [95% Confidence Interval (CI) 0.94; 4.63, p = 0.070]. Patients with UIV ≤ 4.5 vertebrae from the apex had a 1.57 times increased risk of PJK, adjusting for UIV relative to T2 [95% CI 0.64; 3.87, p = 0.326].
Conclusion
SK patients with UIV below T2 had an increased risk of developing PJK at 2 years following PSF. This association supports consideration of UIV location during preoperative planning.
Level of Evidence
Prognostic Level II.
Similar content being viewed by others
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, RS, upon reasonable request.
Code availability
Not applicable.
References
Sardar ZM, Ames RJ, Lenke L (2019) Scheuermannʼs kyphosis. J Am Acad Orthop Surg 27:e462–e472. https://doi.org/10.5435/JAAOS-D-17-00748
Toombs C, Lonner B, Shah S et al (2018) Quality of life improvement following surgery in adolescent spinal deformity patients: a comparison between scheuermann kyphosis and adolescent idiopathic scoliosis*. Spine Deform 6:676–683. https://doi.org/10.1016/j.jspd.2018.04.009
Lorente A, Barrios C, Lorente R et al (2019) Severe hyperkyphosis reduces the aerobic capacity and maximal exercise tolerance in patients with Scheuermann disease. Spine J 19:330–338. https://doi.org/10.1016/j.spinee.2018.07.002
Polly DW, Ledonio CGT, Diamond B et al (2019) What are the indications for spinal fusion surgery in scheuermann kyphosis? J Pediatr Orthop 39:217–221. https://doi.org/10.1097/BPO.0000000000000931
Lowe TG, Kasten MD (1994) An analysis of sagittal curves and balance after cotrel-dubousset instrumentation for kyphosis secondary to scheuermann’s disease: a review of 32 patients. Spine (Phila Pa 1976) 19:1680–1685
Lowe T (1987) Double L-rod instrumentation in the treatment of severe kyphosis secondary to Scheuermann’s disease. Spine (Phila Pa 1976) 12:336–341. https://doi.org/10.1097/00007632-198705000-00005
Papagelopoulos PJ, Klassen RA, Peterson HA et al (2001) Surgical treatment of Scheuermann’s disease with segmental compression instrumentation. Clin Orthop Relat Res 386:139–149
Sturm PF, Dobson JC, Armstrong GW (1993) The surgical management of Scheuermann’s disease. Spine (Phila Pa 1976) 18:685–691. https://doi.org/10.1097/00007632-199305000-00002
Lonner BS, Newton P, Betz R et al (2007) Operative management of Scheuermann’s kyphosis in 78 patients: radiographic outcomes, complications, and technique. Spine (Phila Pa 1976) 32:2644–2652. https://doi.org/10.1097/BRS.0b013e31815a5238
Denis F, Sun EC, Winter RB (2009) Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine (Phila Pa 1976) 34:E729–E734. https://doi.org/10.1097/BRS.0b013e3181ae2ab2
Lonner BS, Parent S, Shah SA et al (2018) Reciprocal changes in sagittal alignment with operative treatment of adolescent scheuermann kyphosis—prospective evaluation of 96 patients. Spine Deform 6:177–184. https://doi.org/10.1016/j.jspd.2017.07.001
Lowe T, Berven SH, Schwab FJ et al (2006) The SRS classification for adult spinal deformity: building on the King/Moe and Lenke classification systems. Spine (Phila Pa 1976) 31:S119–S125. https://doi.org/10.1097/01.brs.0000232709.48446.be
Cahill PJ, Steiner CD, Dakwar E et al (2015) Sagittal spinopelvic parameters in Scheuermann’s kyphosis: a preliminary study. Spine Deform 3:267–271. https://doi.org/10.1016/J.JSPD.2014.11.001
Acknowledgements
Harms Study Group Investigators: Aaron Buckland, MD; New York University, Amer Samdani, MD; Shriners Hospitals for Children—Philadelphia, Amit Jain, MD; Johns Hopkins Hospital, Baron Lonner, MD; Mount Sinai Hospital, Benjamin Roye, MD; Columbia University, Burt Yaszay, MD; Rady Children’s Hospital, Chris Reilly, MD; BC Children’s Hospital, Daniel Hedequist, MD; Boston Children’s Hospital, Daniel Sucato, MD; Texas Scottish Rite Hospital, David Clements, MD; Cooper Bone & Joint Institute New Jersey, Firoz Miyanji, MD; BC Children’s Hospital, Harry Shufflebarger, MD; Paley Orthopedic & Spine Institute, Jack Flynn, MD; Children’s Hospital of Philadelphia, John Asghar, MD; Paley Orthopedic & Spine Institute, Jean Marc Mac Thiong, MD; CHU Sainte-Justine, Joshua Pahys, MD; Shriners Hospitals for Children—Philadelphia, Juergen Harms, MD; Klinikum Karlsbad-Langensteinbach, Karlsbad, Keith Bachmann, MD; University of Virginia, Lawrence Lenke, MD; Columbia University, Lori Karol, MD; Children’s Hospital, Denver Colorado, Mark Abel, MD; University of Virginia, Mark Erickson, MD; Children’s Hospital, Denver Colorado, Michael Glotzbecker, MD; Rainbow Children’s Hospital, Cleveland, Michael Kelly, MD; Washington University, Michael Vitale, MD; Columbia University, Michelle Marks, PT, MA; Setting Scoliosis Straight Foundation, Munish Gupta, MD; Washington University, Nicholas Fletcher, MD; Emory University, Noelle Larson, MD; Mayo Clinic Rochester Minnesota, Patrick Cahill, MD; Children’s Hospital of Philadelphia, Paul Sponseller, MD; Johns Hopkins Hospital, Peter Gabos, MD: Nemours/Alfred I. duPont Hospital for Children, Peter Newton, MD; Rady Children’s Hospital, Peter Sturm, MD; Cincinnati Children’s Hospital, Randal Betz, MD; Institute for Spine & Scoliosis, Stefan Parent, MD: CHU Sainte-Justine, Stephen George, MD; Nicklaus Children's Hospital, Steven Hwang, MD; Shriners Hospitals for Children—Philadelphia, Suken Shah, MD; Nemours/Alfred I. duPont Hospital for Children, Sumeet Garg, MD; Children’s Hospital, Denver Colorado , Tom Errico, MD; Nicklaus Children's Hospital, Vidyadhar Upasani, MD; Rady Children’s Hospital. Harms Non-Fusion Study Group Investigators: Amer Samdani, MD; Shriners Hospitals for Children—Philadelphia, Ahmet Alanay, MD; Acibadem Maslak Hospital, Turkey, Baron Lonner, MD; Mount Sinai Hospital, Bob Cho, MD; Shriner’s Pasadena CA, Burt Yaszay, MD; Rady Children’s Hospital, Caglar Yilgor, MD; Acibadem Maslak Hospital, Turkey, Dan Hoernschmeyer, MD; University of Missouri Health Care , Firoz Miyanji, MD; BC Children’s Hospital, Harry Shufflebarger, MD; Paley Orthopedic & Spine Institute, John Asghar, MD; Paley Orthopedic & Spine Institute, Josh Murphy, MD; Children's Healthcare of Atlanta, Kevin Neal, MD; Nemours Children’s Clinic, Jacksonville, Laurel Blakemore, MD; Pediatric Specialists of Virginia/Children’s National, Lawrence Haber, MD; Ochsner health center for children New Orleans, Noelle Larson, MD; Mayo Clinic Rochester Minnesota, Patrick Cahill, MD; Children’s Hospital of Philadelphia, Peter Newton, MD; Rady Children’s Hospital, Stefan Parent, MD: CHU Sainte-Justine, Suken Shah, MD; Nemours/Alfred I. duPont Hospital for Children.
Funding
This study was supported in part by grants to the Setting Scoliosis Straight Foundation in support of Harms Study Group research from DePuy Synthes Spine, EOS imaging, Stryker Spine, Medtronic, NuVasive, Zimmer Biomet and the Food and Drug Administration.
Author information
Authors and Affiliations
Contributions
ANF, HM, RS, LB-O, BDR, RI, LGL, AL, AZB, ASM, PON, BSL, MGV: Made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data, or the creation of new software used in the work. Drafted the work or revised it critically for important intellectual content. Approved of the version to be published. Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
ANF has no conflicts of interest to disclose. HM has received consulting fees from the Pediatric Spine Study Group, as well as research grants from Pediatric Orthopaedic Society of North America and Scoliosis Research Society. RS has no conflicts of interest to disclose. LB has no conflicts of interest to disclose. AZB has no conflicts of interest to disclose. BDR has received research support from Children’s Spine Foundation, Scoliosis Research Society, Pediatric Orthopaedic Society of North America, Broadwater, Pediatric Orthopaedic Club of New York, OMeGA Medical Grants Association, and Setting Scoliosis Straight Foundation (Harms). RI has no conflicts of interest to disclose. LGL has received personal fees from Medtronic, non-financial support from Broadwater, grants and non-financial support from Scoliosis Research Society, grants from EOS, grants from Setting Scoliosis Straight Foundation, philanthropic support from Evans Family Donation, philanthropic support from Fox Family Foundation, grants and non-financial support from AOSpine, personal fees from Abryx, personal fees from EOS technologies, and personal fees from Acuity Surgical. AL has no conflicts of interest to disclose. ASM has no conflicts of interest to disclose. PON is a board member for Setting Scoliosis Straight Foundation, Rady Children’s Specialists, Scoliosis Research Society, and International Pediatric Orthopedic Think Tank. PON reports grants from Setting Scoliosis Straight Foundation, grants personal fees, and non-financial support from DePuy Synthes Spine, grants and personal fees from Scoliosis Research Society, grants from EOS imaging, personal fees from Thieme Publishing, grants from NuVasive, personal fees from Electrocore, personal fees from Cubist, grants, non-financial support and institutional support from Orthopediatrics, grants, personal fees and non-financial support from Stryker/K2M, grants and non-financial support from Alphatech, grants from Mazor Robotics, personal fees from MiRus, personal fees from Globus Medical, and personal fees from Pacira. PON has a patent Anchoring systems and methods for correcting spinal deformities (8540754) with royalties paid to DePuy Synthes Spine, a patent Low profile spinal tethering systems (8123749) licensed to DePuy Spine, Inc., a patent Screw placement guide (7981117) licensed to DePuy Spine, Inc., a patent Compressor for use in minimally invasive surgery (7189244) licensed to DePuy Spine, Inc., and a patent Posterior spinal fixation pending to K2M. BL has received grants from Depuy Synthes to Setting Scoliosis Straight Foundation in support of the Harms Study Group’s research, personal fees from DePuy synthes, personal fees from Zimmer Biomet, personal fees from ApiFix, personal fees from SpineSearch, personal fees from Paradigm Spine, non-financial support from Setting Scoliosis Straight Foundation. BL is on the editorial board for SRS Spine Deformity Journal. MGV has received grants and personal fees from Biomet, grants and non-financial support from Children’s Spine Foundation, personal fees from East Coast Orthotics and Prosthetics, financial support from Fox, non-financial support from IPOS, grants from OREF, grants and non-financial support from POSNA, non-financial support from Project for Safety in Spine Surgery, grants from OSRF, grants from SRS, personal fees from Stryker, and non-financial support from Wellinks.
Ethical approval
This study was approved by the Columbia University Institutional Review Board under protocol AAAT0762 and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all participants included in this study upon enrollment into the registry.
Consent for publication
No patient identifying information is included in the article. Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fano, A.N., Matsumoto, H., Sinha, R. et al. Operative choices matter: the role of UIV and sagittal balance in the development of proximal junctional kyphosis following posterior instrumentation for Scheuermann’s kyphosis. Spine Deform 11, 993–1000 (2023). https://doi.org/10.1007/s43390-023-00666-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00666-1