Abstract
Nlrp2 encodes a protein of the oocyte subcortical maternal complex (SCMC), required for embryo development. We previously showed that loss of maternal Nlrp2 in mice causes subfertility, smaller litters with birth defects, and growth abnormalities in offspring, indicating that Nlrp2 is a maternal effect gene and that all embryos from Nlrp2-deficient females that were cultured in vitro arrested before the blastocysts stage. Here, we used time-lapse microscopy to examine the development of cultured embryos from superovulated Nlrp2-deficient and wild-type mice after in vivo and in vitro fertilization. Embryos from Nlrp2-deficient females had similar abnormal cleavage and fragmentation and arrested by blastocyst stage, irrespective of fertilization mode. This indicates that in vitro fertilization does not further perturb or improve the development of cultured embryos. We also transferred embryos from superovulated Nlrp2-deficient and wild-type females to wild-type recipients to investigate if the abnormal reproductive outcomes of Nlrp2-deficient females are primarily driven by oocyte dysfunction or if a suboptimal intra-uterine milieu is a necessary factor. Pregnancies with transferred embryos from Nlrp2-deficient females produced smaller litters, stillbirths, and offspring with birth defects and growth abnormalities. This indicates that the reproductive phenotype is oocyte-specific and is not rescued by development in a wild-type uterus. We further found abnormal DNA methylation at two maternally imprinted loci in the kidney of surviving young adult offspring, confirming persistent DNA methylation disturbances in surviving offspring. These findings have implications for fertility treatments for women with mutations in NLRP2 and other genes encoding SCMC proteins.







Similar content being viewed by others
References
Barbieri RL. Female infertility. In: Strauss III JF, Barbieri RL, Gargiulo AR, editors. Yen & Jeffe’s reproductive endocrinology. Physiology, pathophysiology and clinical management, eighth ed. Philadelphia: Elsevier; 2019. p. 556–81.
Practice Committee of the American Society for Reproductive Medicine. Electronic address aao, Practice Committee of the American Society for Reproductive M. Evidence-based treatments for couples with unexplained infertility: a guideline. Fertil Steril. 2020;113:305–22.
Tarin JJ, Garcia-Perez MA, Cano A. Assisted reproductive technology results: why are live-birth percentages so low? Mol Reprod Dev. 2014;81:568–83.
Gunn DD, Bates GW. Evidence-based approach to unexplained infertility: a systematic review. Fertil Steril. 2016;105:1566–74 e1561.
Pisarska MD, Chan JL, Lawrenson K, Gonzalez TL, Wang ET. Genetics and epigenetics of infertility and treatments on outcomes. J Clin Endocrinol Metab. 2019;104:1871–86.
Thirumavalavan N, Gabrielsen JS, Lamb DJ. Where are we going with gene screening for male infertility? Fertil Steril. 2019;111:842–50.
Yatsenko SA, Rajkovic A. Genetics of human female infertility. Biol Reprod. 2019; 101(3), 549–566.
Wang H, Dey SK. Roadmap to embryo implantation: clues from mouse models. Nat Rev Genet. 2006;7:185–99.
Kim KH, Lee KA. Maternal effect genes: findings and effects on mouse embryo development. Clin Exp Reprod Med. 2014;41:47–61.
Begemann M, Rezwan FI, Beygo J, Docherty LE, Kolarova J, Schroeder C, Buiting K, Chokkalingam K, Degenhardt F, Wakeling EL, Kleinle S, Gonzalez Fassrainer D, et al. Maternal variants in NLRP and other maternal effect proteins are associated with multilocus imprinting disturbance in offspring. J Med Genet. 2018; J Med Genet, 55(7), 497–504.
Amoushahi M, Sunde L, Lykke-Hartmann K. The pivotal roles of the NOD-like receptors with a PYD domain, NLRPs, in oocytes and early embryo development. Biol Reprod. 2019;101:284–96.
Li L, Lu X, Dean J. The maternal to zygotic transition in mammals. Mol Asp Med. 2013;34:919–38.
Eckersley-Maslin MA, Alda-Catalinas C, Reik W. Dynamics of the epigenetic landscape during the maternal-to-zygotic transition. Nat Rev Mol Cell Biol. 2018;19:436–50.
Ohsugi M, Zheng P, Baibakov B, Li L, Dean J. Maternally derived FILIA-MATER complex localizes asymmetrically in cleavage-stage mouse embryos. Development. 2008;135:259–69.
Li L, Baibakov B, Dean J. A subcortical maternal complex essential for preimplantation mouse embryogenesis. Dev Cell. 2008;15:416–25.
Yu XJ, Yi Z, Gao Z, Qin D, Zhai Y, Chen X, et al. The subcortical maternal complex controls symmetric division of mouse zygotes by regulating F-actin dynamics. Nat Commun. 2014;5:4887.
Zhu K, Yan L, Zhang X, Lu X, Wang T, Yan J, et al. Identification of a human subcortical maternal complex. Mol Hum Reprod. 2015;21:320–9.
Bebbere D, Masala L, Albertini DF, Ledda S. The subcortical maternal complex: multiple functions for one biological structure? J Assist Reprod Genet. 2016;33:1431–8.
Monk D, Sanchez-Delgado M, Fisher R. NLRPs, the subcortical maternal complex and genomic imprinting. Reproduction. 2017;154:R161–70.
Yurttas P, Vitale AM, Fitzhenry RJ, Cohen-Gould L, Wu W, Gossen JA, et al. Role for PADI6 and the cytoplasmic lattices in ribosomal storage in oocytes and translational control in the early mouse embryo. Development. 2008;135:2627–36.
Li L, Zheng P, Dean J. Maternal control of early mouse development. Development. 2010;137:859–70.
Zheng P, Dean J. Role of Filia, a maternal effect gene, in maintaining euploidy during cleavage-stage mouse embryogenesis. Proc Natl Acad Sci U S A. 2009;106:7473–8.
Duncan FE, Padilla-Banks E, Bernhardt ML, Ord TS, Jefferson WN, Moss SB, et al. Transducin-like enhancer of split-6 (TLE6) is a substrate of protein kinase A activity during mouse oocyte maturation. Biol Reprod. 2014;90:63.
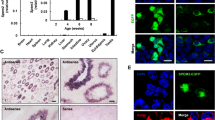
Mahadevan S, Sathappan V, Utama B, Lorenzo I, Kaskar K, Van den Veyver IB. Maternally expressed NLRP2 links the subcortical maternal complex (SCMC) to fertility, embryogenesis and epigenetic reprogramming. Sci Rep. 2017;7:44667.
Murdoch S, Djuric U, Mazhar B, Seoud M, Khan R, Kuick R, et al. Mutations in NALP7 cause recurrent hydatidiform moles and reproductive wastage in humans. Nat Genet. 2006;38:300–2.
Kou YC, Shao L, Peng HH, Rosetta R, del Gaudio D, Wagner AF, et al. A recurrent intragenic genomic duplication, other novel mutations in NLRP7 and imprinting defects in recurrent biparental hydatidiform moles. Mol Hum Reprod. 2008;14:33–40.
Meyer E, Lim D, Pasha S, Tee LJ, Rahman F, Yates JR, et al. Germline mutation in NLRP2 (NALP2) in a familial imprinting disorder (Beckwith-Wiedemann syndrome). PLoS Genet. 2009;5:e1000423.
Alazami AM, Awad SM, Coskun S, Al-Hassan S, Hijazi H, Abdulwahab FM, et al. TLE6 mutation causes the earliest known human embryonic lethality. Genome Biol. 2015;16:240.
Aghajanova L, Mahadevan S, Altmae S, Stavreus-Evers A, Regan L, Sebire N, et al. No evidence for mutations in NLRP7, NLRP2 or KHDC3L in women with unexplained recurrent pregnancy loss or infertility. Hum Reprod. 2015;30:232–8.
Nguyen NMP, Ge ZJ, Reddy R, Fahiminiya S, Sauthier P, Bagga R, et al. Causative mutations and mechanism of androgenetic hydatidiform moles. Am J Hum Genet. 2018;103:740–51.
Wang X, Song D, Mykytenko D, Kuang Y, Lv Q, Li B, Chen B, Mao X, Xu Y, Zukin V, Mazur P, Mu J, et al. Novel mutations in genes encoding subcortical maternal complex proteins may cause human embryonic developmental arrest. Reproductive BioMedicine Online. 2018; 36(6), 698–704.
Qian J, Nguyen NMP, Rezaei M, Huang B, Tao Y, Zhang X, et al. Biallelic PADI6 variants linking infertility, miscarriages, and hydatidiform moles. Eur J Hum Genet. 2018;26:1007–13.
Robbins SM, Thimm MA, Valle D, Jelin AC. Genetic diagnosis in first or second trimester pregnancy loss using exome sequencing: a systematic review of human essential genes. J Assist Reprod Genet. 2019;36:1539–48.
Demond H, Anvar Z, Jahromi BN, Sparago A, Verma A, Davari M, et al. A KHDC3L mutation resulting in recurrent hydatidiform mole causes genome-wide DNA methylation loss in oocytes and persistent imprinting defects post-fertilisation. Genome Med. 2019;11:84.
Xu Y, Shi Y, Fu J, Yu M, Feng R, Sang Q, et al. Mutations in PADI6 cause female infertility characterized by early embryonic arrest. Am J Hum Genet. 2016;99:744–52.
Mahadevan S, Wen S, Wan YW, Peng HH, Otta S, Liu Z, et al. NLRP7 affects trophoblast lineage differentiation, binds to overexpressed YY1 and alters CpG methylation. Hum Mol Genet. 2014;23:706–16.
Judson H, Hayward BE, Sheridan E, Bonthron DT. A global disorder of imprinting in the human female germ line. Nature. 2002;416:539–42.
Parry DA, Logan CV, Hayward BE, Shires M, Landolsi H, Diggle C, et al. Mutations causing familial biparental hydatidiform mole implicate c6orf221 as a possible regulator of genomic imprinting in the human oocyte. Am J Hum Genet. 2011;89:451–8.
Reddy R, Akoury E, Phuong Nguyen NM, Abdul-Rahman OA, Dery C, Gupta N, Daley WP, Ao A, Landolsi H, Ann Fisher R, Touitou I, Slim R. Report of four new patients with protein-truncating mutations in C6orf221/KHDC3L and colocalization with NLRP7. Eur J Hum Genet. 2013; 21(9), 957–964.
Ulker V, Gurkan H, Tozkir H, Karaman V, Ozgur H, Numanoglu C, et al. Novel NLRP7 mutations in familial recurrent hydatidiform mole: are NLRP7 mutations a risk for recurrent reproductive wastage? Eur J Obstet Gynecol Reprod Biol. 2013;170:188–92.
Andreasen L, Bolund L, Niemann I, Hansen ES, Sunde L. Mosaic moles and non-familial biparental moles are not caused by mutations in NLRP7, NLRP2 or C6orf221. Mol Hum Reprod. 2012;18:593–8.
Huang JY, Su M, Lin SH, Kuo PL. A genetic association study of NLRP2 and NLRP7 genes in idiopathic recurrent miscarriage. Hum Reprod. 2013;28:1127–34.
Mu J, Wang W, Chen B, Wu L, Li B, Mao X, et al. Mutations in NLRP2 and NLRP5 cause female infertility characterised by early embryonic arrest. J Med Genet. 2019;56:471–80.
Tian X, Pascal G, Monget P. Evolution and functional divergence of NLRP genes in mammalian reproductive systems. BMC Evol Biol. 2009;9:202–14.
Lupfer C, Kanneganti TD. Unsolved mysteries in NLR biology. Front Immunol. 2013;4:285.
Palladino MA, Johnson TA, Gupta R, Chapman JL, Ojha P. Members of the toll-like receptor family of innate immunity pattern-recognition receptors are abundant in the male rat reproductive tract. Biol Reprod. 2007;76:958–64.
Fazeli A, Bruce C, Anumba DO. Characterization of toll-like receptors in the female reproductive tract in humans. Hum Reprod. 2005;20:1372–8.
Kumaki Y, Oda M, Okano M. QUMA: quantification tool for methylation analysis. Nucleic Acids Res. 2008;36:W170–5.
Demond H, Anvar Z, Jahromi BN, Sparago A, Verma A, Davari M, et al. A KHDC3L mutation resulting in recurrent hydatidiform mole causes genome-wide DNA methylation loss in oocytes and persistent imprinting defects post-fertilisation. Genome Med. 2019;11:1–14.
Lu X, Gao Z, Qin D, Li L. A maternal functional module in the mammalian oocyte-to-embryo transition. Trends Mol Med. 2017;23:1014–23.
Docherty LE, Rezwan FI, Poole RL, Turner CL, Kivuva E, Maher ER, et al. Mutations in NLRP5 are associated with reproductive wastage and multilocus imprinting disorders in humans. Nat Commun. 2015;6:8086.
Lin J, Xu H, Chen B, Wang W, Wang L, Sun X, et al. Expanding the genetic and phenotypic spectrum of female infertility caused by TLE6 mutations. J Assist Reprod Genet. 2020;37:437–42.
Pal L, Toth TL, Leykin L, Isaacson KB. High incidence of triploidy in in-vitro fertilized oocytes from a patient with a previous history of recurrent gestational trophoblastic disease. Hum Reprod. 1996;11:1529–32.
Sills ES, Obregon-Tito AJ, Gao H, McWilliams TK, Gordon AT, Adams CA, et al. Pathogenic variant in NLRP7 (19q13.42) associated with recurrent gestational trophoblastic disease: data from early embryo development observed during in vitro fertilization. Clin Exp Reprod Med. 2017;44:40–6.
Ogura Y, Sutterwala FS, Flavell RA. The inflammasome: first line of the immune response to cell stress. Cell. 2006;126:659–62.
Pinheiro AS, Proell M, Eibl C, Page R, Schwarzenbacher R, Peti W. Three-dimensional structure of the NLRP7 pyrin domain: insight into pyrin-pyrin-mediated effector domain signaling in innate immunity. J Biol Chem. 2010;285:27402–10.
Kufer TA, Sansonetti PJ. NLR functions beyond pathogen recognition. Nat Immunol. 2011;12:121–8.
Tilburgs T, Meissner TB, Ferreira LMR, Mulder A, Musunuru K, Ye J, et al. NLRP2 is a suppressor of NF-kB signaling and HLA-C expression in human trophoblasts. Biol Reprod. 2017;96:831–42.
Huang JY, Yu PH, Li YC, Kuo PL. NLRP7 contributes to in vitro decidualization of endometrial stromal cells. Reprod Biol Endocrinol. 2017;15:66.
Bullon P, Navarro JM. Inflammasome as a key pathogenic mechanism in endometriosis. Curr Drug Targets. 2017;18:997–1002.
Akoury E, Gupta N, Bagga R, Brown S, Dery C, Kabra M, et al. Live births in women with recurrent hydatidiform mole and two NLRP7 mutations. Reprod BioMed Online. 2015;31:120–4.
Fisher RA, Lavery SA, Carby A, Abu-Hayyeh S, Swingler R, Sebire NJ, et al. What a difference an egg makes. Lancet. 2011;378:1974.
Peng H, Chang B, Lu C, Su J, Wu Y, Lv P, et al. Nlrp2, a maternal effect gene required for early embryonic development in the mouse. PLoS One. 2012;7:e30344.
Acknowledgments
We thank our lab members for critical reading of the manuscript and helpful suggestions.
Funding
This work was supported in part by grants from Integramed to J.R. and S.A., by grants R01HD079442 and R01HD092746 to IBV, and by the administrative core of the IDDRC grant U54 HD083092 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. We thank the Mouse ES Cell Core and the Genetically Engineered Mouse Core, partially supported by the National Institutes of Health (NIH) grant P30CA125123.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All experiments were approved by the Baylor College of Medicine Institutional Animal Care and Use Committee (protocol AN-2035). Animal facilities were accredited by the Association for Assessment and Accreditation for Laboratory Animal Care International (AAALAC).
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Institutes of Health.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Summary Sentence
Female mice with loss of Nlrp2 have poor reproductive outcomes that are not rescued by in vitro fertilization or transfer of embryos to the uterus of a wild-type female, supporting that this maternal effect mutation causes an oocyte-specific defect.
Electronic Supplementary Material
Supplemental Figure 1
Embryo transfer pregnancy outcomes including recipients that did not achieve pregnancy. (A) Litter sizes (Y-axis) at postnatal day 0 (PND0; left two bars) and remaining litter sizes at postnatal day 21 (PND21; right two bars ) of ICR recipients of Nlrp2M+/P-/Z+ (blue) and Nlrp2M-/P+/Z+ (red) embryos, including recipients that did not achieve pregnancy. The average litter size +/- standard deviation is given below each bar and the N above each bar indicates the total number of offspring for respective stage and genotype; p-values indicate the significance of difference between genotype. (B) Livebirth rates of Nlrp2M+/P-/Z+ and Nlrp2M-/P+/Z+ offspring, including recipients that did not achieve a pregnancy. (PNG 169 kb)
Supplemental figure 2
Comparisons of skeletal staining between the Nlrp2M+/P-/Z+ and Nlrp2M-/P+/Z+ offspring. (A) Skeletal staining at PND21 of the same mice shown in Figure 6, but from a lateral view; Nlrp2M+/P-/Z+ is on the left and Nlrp2M-/P+/Z+ is on the right. The Nlrp2M-/P+/Z+ mouse is severely growth restricted with shortened long bones. (B) Black arrows point to fusion between vertebral bones in the Nlrp2M+/P-/Z+ mouse which is not seen in the Nlrp2M-/P+/Z+ mouse (dashed arrows). (C) Black arrow in the Nlrp2M+/P-/Z+ mouse points to the patella, which was not seen in the Nlrp2M-/P+/Z+ mouse (dashed arrow). (D) Secondary ossification centers in the hind-paw of Nlrp2M+/P−/Z+ offspring (black arrow) appears to underdeveloped in the Nlrp2M-/P+/Z+ mouse (dashed arrow). (PNG 1232 kb)
ESM 1
(DOCX 15 kb)
Supplemental video 1
Embryoscope time-lapse microscopy (Orignal 149.7 h, condensed to 28.76 sec) of in vivo fertilized embryos from Nlrp2tm1a/tm1a mice cultured in vitro. Developmental arrest at two-cell stage (bottom embryo) and no obvious blastocoel cavity formation followed by fragmentation (top embryo) are shown. (MP4 2071 kb)
Supplemental video 2
Embryoscope time-lapse microscopy (Orignal 161.8 h, condensed to 31.16 sec) of cultured in vitro fertilized embryos from Nlrp2tm1a/tm1a mice. Morphologically atypical blastocoel cavities are formed in both embryos before fragmentation is observed. (MP4 2794 kb)
Rights and permissions
About this article
Cite this article
Arian, S., Rubin, J., Chakchouk, I. et al. Reproductive Outcomes from Maternal Loss of Nlrp2 Are Not Improved by IVF or Embryo Transfer Consistent with Oocyte-Specific Defect. Reprod. Sci. 28, 1850–1865 (2021). https://doi.org/10.1007/s43032-020-00360-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-020-00360-x