Abstract
Some chronic pain conditions and comorbidities suppress the hypothalamic-pituitary-adrenal (HPA) axis and response to dynamic testing. We measured HPA axis responses to corticotropin-releasing hormone (CRH) administration in relation to chronic pelvic pain and endometriosis. In a cross-sectional study of women (n = 54) with endometriosis-associated chronic pelvic pain (n = 22), chronic pelvic pain alone (n = 12), or healthy volunteers (n = 20), adrenocorticotropic-releasing hormone (ACTH) and cortisol levels were measured at 0, 15, 30, and 45 min after intravenous ovine CRH administration. ACTH and cortisol delta (peak-baseline) and area under the curve (AUC) were compared by study group and assessed for association with race and menstrual and non-menstrual pain severity. HPA axis responses did not differ among the racially diverse groups or in those with pain compared with healthy volunteers. However, when stratified by race, ACTH delta (129.9 ± 130.7 vs. 52.5 ± 66.0 pg/mL; p = 0.003), ACTH AUC (4813 ± 4707 vs. 2290 ± 2900 min*pg/mL; p = 0.013), and cortisol delta (26.3 ± 21.5 vs. 13.2 ± 9.7 μg/mL; p = 0.005) were significantly higher in black (n = 10) than predominately white (non-black) subjects (n = 44; 39/44 white). In analyses among primarily white (non-black) women, greater menstrual pain severity was associated with blunted ACTH delta (p = 0.015) and cortisol delta (p = 0.023), and greater non-menstrual pain severity with blunted cortisol delta (p = 0.017). Neuroendocrine abnormalities in women with chronic pelvic pain may differ by pain manifestations and may vary by race. The higher HPA axis response in black women merits investigation in pelvic pain studies stratified by race. In white (non-black) women experiencing pain, a blunted response was related to pain severity suggesting pain affects women independently of endometriosis lesions.



Similar content being viewed by others
References
Peiris AN, Chaljub E, Medlock D. Endometriosis. Jama. 2018;320(24):2608. https://doi.org/10.1001/jama.2018.17953.
Stratton P, Khachikyan I, Sinaii N, Ortiz R, Shah J. Association of chronic pelvic pain and endometriosis with signs of sensitization and myofascial pain. Obstet Gynecol. 2015;125(3):719–28. https://doi.org/10.1097/AOG.0000000000000663.
Evans SF, Brooks TA, Esterman AJ, Hull ML, Rolan PE. The comorbidities of dysmenorrhea: a clinical survey comparing symptom profile in women with and without endometriosis. J Pain Res. 2018;11:3181–94. https://doi.org/10.2147/JPR.S179409.
Cavaggioni G, Lia C, Resta S, Antonielli T, Benedetti Panici P, Megiorni F, et al. Are mood and anxiety disorders and alexithymia associated with endometriosis? A preliminary study. Biomed Res Int. 2014;2014:786830–5. https://doi.org/10.1155/2014/786830.
Gambadauro P, Carli V, Hadlaczky G. Depressive symptoms among women with endometriosis: a systematic review and meta-analysis. Am J Obstet Gynecol. 2018;220:230–41. https://doi.org/10.1016/j.ajog.2018.11.123.
Nunes FR, Ferreira JM, Bahamondes L. Pain threshold and sleep quality in women with endometriosis. Eur J Pain. 2015;19(1):15–20. https://doi.org/10.1002/ejp.514.
Sinaii N, Cleary SD, Ballweg ML, Nieman LK, Stratton P. High rates of autoimmune and endocrine disorders, fibromyalgia, chronic fatigue syndrome and atopic diseases among women with endometriosis: a survey analysis. Hum Reprod. 2002;17(10):2715–24.
Cagnacci A, Della Vecchia E, Xholli A. Chronic pelvic pain improvement: impact on quality of life and mood. Gynecol Endocrinol. 2019;35:1–4. https://doi.org/10.1080/09513590.2018.1540571.
Dhabhar FS. Effects of stress on immune function: the good, the bad, and the beautiful. Immunol Res. 2014;58(2–3):193–210. https://doi.org/10.1007/s12026-014-8517-0.
Kuehl LK, Michaux GP, Richter S, Schachinger H, Anton F. Increased basal mechanical pain sensitivity but decreased perceptual wind-up in a human model of relative hypocortisolism. Pain. 2010;149(3):539–46. https://doi.org/10.1016/j.pain.2010.03.026.
McEwen BS, Kalia M. The role of corticosteroids and stress in chronic pain conditions. Metabolism. 2010;59(Suppl 1):S9–15. https://doi.org/10.1016/j.metabol.2010.07.012.
Wingenfeld K, Heim C, Schmidt I, Wagner D, Meinlschmidt G, Hellhammer DH. HPA axis reactivity and lymphocyte glucocorticoid sensitivity in fibromyalgia syndrome and chronic pelvic pain. Psychosom Med. 2008;70(1):65–72. https://doi.org/10.1097/PSY.0b013e31815ff3ce.
Wingenfeld K, Wolf OT. Effects of cortisol on cognition in major depressive disorder, posttraumatic stress disorder and borderline personality disorder - 2014 Curt Richter Award Winner. Psychoneuroendocrinology. 2015;51:282–95. https://doi.org/10.1016/j.psyneuen.2014.10.009.
Nederhof E, van Oort FV, Bouma EM, Laceulle OM, Oldehinkel AJ, Ormel J. Predicting mental disorders from hypothalamic-pituitary-adrenal axis functioning: a 3-year follow-up in the TRAILS study. Psychol Med. 2015;45(11):2403–12. https://doi.org/10.1017/S0033291715000392.
Vincent K, Warnaby C, Stagg CJ, Moore J, Kennedy S, Tracey I. Dysmenorrhoea is associated with central changes in otherwise healthy women. Pain. 2011;152(9):1966–75. https://doi.org/10.1016/j.pain.2011.03.029.
Petrelluzzi KF, Garcia MC, Petta CA, Grassi-Kassisse DM, Spadari-Bratfisch RC. Salivary cortisol concentrations, stress and quality of life in women with endometriosis and chronic pelvic pain. Stress. 2008;11(5):390–7. https://doi.org/10.1080/10253890701840610.
van Aken M, Oosterman J, van Rijn T, Ferdek M, Ruigt G, Kozicz T, et al. Hair cortisol and the relationship with chronic pain and quality of life in endometriosis patients. Psychoneuroendocrinology. 2018;89:216–22. https://doi.org/10.1016/j.psyneuen.2018.01.001.
Yanovski JA, Yanovski SZ, Boyle AJ, Gold PW, Sovik KN, Sebring NG, et al. Hypothalamic-pituitary-adrenal axis activity during exercise in African American and Caucasian women. J Clin Endocrinol Metab. 2000;85(8):2660–3. https://doi.org/10.1210/jcem.85.8.6708.
Yanovski JA, Yanovski SZ, Friedman TC, Loh YP, Jayasvasti V, Cutler GB Jr, et al. Etiology of the differences in corticotropin-releasing hormone-induced adrenocorticotropin secretion of black and white women. J Clin Endocrinol Metab. 1996;81(9):3307–11. https://doi.org/10.1210/jcem.81.9.8784088.
Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. The effect of age on pain, function, and quality of life after total hip and knee arthroplasty. Arch Intern Med. 2001;161(3):454–60.
Skinner ML, Shirtcliff EA, Haggerty KP, Coe CL, Catalano RF. Allostasis model facilitates understanding race differences in the diurnal cortisol rhythm. Dev Psychopathol. 2011;23(4):1167–86. https://doi.org/10.1017/S095457941100054X.
Azziz R, Fox LM, Zacur HA, Parker CR Jr, Boots LR. Adrenocortical secretion of dehydroepiandrosterone in healthy women: highly variable response to adrenocorticotropin. J Clin Endocrinol Metab. 2001;86(6):2513–7. https://doi.org/10.1210/jcem.86.6.7587.
Parkerson GR Jr, Broadhead WE, Tse CK. The Duke Health Profile. A 17-item measure of health and dysfunction. Med Care. 1990;28(11):1056–72.
Quinones M, Urrutia R, Torres-Reveron A, Vincent K, Flores I. Anxiety, coping skills and hypothalamus-pituitary-adrenal (HPA) axis in patients with endometriosis. J Reprod Biol Health. 2015;3:1–17. https://doi.org/10.7243/2054-0841-3-2.
Gold PW, Chrousos GP. Organization of the stress system and its dysregulation in melancholic and atypical depression: high vs low CRH/NE states. Mol Psychiatry. 2002;7(3):254–75. https://doi.org/10.1038/sj.mp.4001032.
Dinan TG, Quigley EM, Ahmed SM, Scully P, O'Brien S, O’Mahony L, et al. Hypothalamic-pituitary-gut axis dysregulation in irritable bowel syndrome: plasma cytokines as a potential biomarker? Gastroenterology. 2006;130(2):304–11. https://doi.org/10.1053/j.gastro.2005.11.033.
Neeck G, Crofford LJ. Neuroendocrine perturbations in fibromyalgia and chronic fatigue syndrome. Rheum Dis Clin N Am. 2000;26(4):989–1002.
Pariante CM, Lightman SL. The HPA axis in major depression: classical theories and new developments. Trends Neurosci. 2008;31(9):464–8. https://doi.org/10.1016/j.tins.2008.06.006.
Galli U, Gaab J, Ettlin DA, Ruggia F, Ehlert U, Palla S. Enhanced negative feedback sensitivity of the hypothalamus-pituitary-adrenal axis in chronic myogenous facial pain. Eur J Pain. 2009;13(6):600–5. https://doi.org/10.1016/j.ejpain.2008.07.010.
Brawn J, Morotti M, Zondervan KT, Becker CM, Vincent K. Central changes associated with chronic pelvic pain and endometriosis. Hum Reprod Update. 2014;20(5):737–47. https://doi.org/10.1093/humupd/dmu025.
Blackburn-Munro G. Hypothalamo-pituitary-adrenal axis dysfunction as a contributory factor to chronic pain and depression. Curr Pain Headache Rep. 2004;8(2):116–24.
Gold PW. The organization of the stress system and its dysregulation in depressive illness. Mol Psychiatry. 2015;20(1):32–47. https://doi.org/10.1038/mp.2014.163.
Bulun SE. Endometriosis. N Engl J Med. 2009;360(3):268–79. https://doi.org/10.1056/NEJMra0804690.
Cuevas M, Flores I, Thompson KJ, Ramos-Ortolaza DL, Torres-Reveron A, Appleyard CB. Stress exacerbates endometriosis manifestations and inflammatory parameters in an animal model. Reprod Sci. 2012;19(8):851–62. https://doi.org/10.1177/1933719112438443.
Appleyard CB, Cruz ML, Hernandez S, Thompson KJ, Bayona M, Flores I. Stress management affects outcomes in the pathophysiology of an endometriosis model. Reprod Sci. 2015;22(4):431–41. https://doi.org/10.1177/1933719114542022.
Torres-Reveron A, Rivera-Lopez LL, Flores I, Appleyard CB. Antagonizing the corticotropin releasing hormone receptor 1 with antalarmin reduces the progression of endometriosis. PLoS One. 2018;13(11):e0197698. https://doi.org/10.1371/journal.pone.0197698.
Friggi Sebe Petrelluzzi K, Garcia MC, Petta CA, Ribeiro DA, de Oliveira Monteiro NR, Cespedes IC, et al. Physical therapy and psychological intervention normalize cortisol levels and improve vitality in women with endometriosis. J Psychosom Obstet Gynaecol. 2012;33(4):191–8. https://doi.org/10.3109/0167482X.2012.729625.
Yanovski JA, Yanovski SZ, Gold PW, Chrousos GP. Differences in the hypothalamic-pituitary-adrenal axis of black and white women. J Clin Endocrinol Metab. 1993;77(2):536–41. https://doi.org/10.1210/jcem.77.2.8393890.
Hajat A, Diez-Roux A, Franklin TG, Seeman T, Shrager S, Ranjit N, et al. Socioeconomic and race/ethnic differences in daily salivary cortisol profiles: the multi-ethnic study of atherosclerosis. Psychoneuroendocrinology. 2010;35(6):932–43. https://doi.org/10.1016/j.psyneuen.2009.12.009.
Karlamangla AS, Friedman EM, Seeman TE, Stawksi RS, Almeida DM. Daytime trajectories of cortisol: demographic and socioeconomic differences--findings from the National Study of Daily Experiences. Psychoneuroendocrinology. 2013;38(11):2585–97. https://doi.org/10.1016/j.psyneuen.2013.06.010.
Ehrstrom S, Kornfeld D, Rylander E, Bohm-Starke N. Chronic stress in women with localised provoked vulvodynia. J Psychosom Obstet Gynaecol. 2009;30(1):73–9. https://doi.org/10.1080/01674820802604359.
Stalder T, Kirschbaum C, Kudielka BM, Adam EK, Pruessner JC, Wust S, et al. Assessment of the cortisol awakening response: expert consensus guidelines. Psychoneuroendocrinology. 2016;63:414–32. https://doi.org/10.1016/j.psyneuen.2015.10.010.
Wolfram M, Bellingrath S, Kudielka BM. The cortisol awakening response (CAR) across the female menstrual cycle. Psychoneuroendocrinology. 2011;36(6):905–12. https://doi.org/10.1016/j.psyneuen.2010.12.006.
Pluchino N, Wenger JM, Petignat P, Tal R, Bolmont M, Taylor HS, et al. Sexual function in endometriosis patients and their partners: effect of the disease and consequences of treatment. Hum Reprod Update. 2016;22(6):762–74. https://doi.org/10.1093/humupd/dmw031.
Funding
This study was financially supported by the NIH Clinical Center and Intramural Research Program of Eunice Kennedy Shriver National Institute of Child Health and Human Development and National Institute of Neurological Disorders and Stroke, Clinical Trial Registration Number NCT00073801.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Stegmann worked for Merck for 3 years and owns Merck stock. Dr. Stratton is conducting a different NIH clinical trial on endometriosis and chronic pelvic pain, which is supported by Allergan through a clinical trial agreement and has received royalties from UpToDate for a section about acute pelvic pain. The remaining authors report no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (National Institutes of Health Clinical Center and the NICHD IRB (NCT00073801)) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
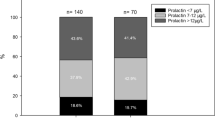
Fig. 1
Adrenocorticotropic releasing hormone (ACTH) measures in women with endometriosis, chronic pelvic pain only, and healthy volunteers, by race. Subjects were women with chronic pelvic pain only (chronic pelvic pain and no endometriosis) (n = 12, black subjects n = 3), chronic pelvic pain and biopsy-proven endometriosis (n = 22, black subjects n = 3), and healthy volunteers (n = 20, black subjects = 4). Data are mean and standard errors; the only observed statistically significant difference among groups was for age-adjusted baseline ACTH in the non-black subjects (p = 0.020). (PPTX 66.9 kb)
Fig. 2
Cortisol measures in women with endometriosis, chronic pelvic pain only, and healthy volunteers, by race. Subjects were women with chronic pelvic pain only (chronic pelvic pain and no endometriosis) (n = 12, black subjects n = 3), chronic pelvic pain and biopsy-proven endometriosis (n = 22, black subjects n = 3), and healthy volunteers (n = 20, black subjects = 4). Data are mean and standard errors; no statistically significant differences in baseline, delta, or AUC cortisol values were observed among groups of either race. (PPTX 65.6 kb)
Rights and permissions
About this article
Cite this article
Ortiz, R., Gemmill, J.A.L., Sinaii, N. et al. Hypothalamic-Pituitary-Adrenal Axis Responses in Women with Endometriosis-Related Chronic Pelvic Pain. Reprod. Sci. 27, 1839–1847 (2020). https://doi.org/10.1007/s43032-020-00201-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-020-00201-x