Abstract
Background
Hepatitis C virus (HCV) infection is associated with chronic liver disease, resulting in cirrhosis and hepatocellular carcinoma. Approximately 20% of HCV infections are spontaneously resolved. Here, we assessed the hierarchical relevance of host factors contributing to viral clearance.
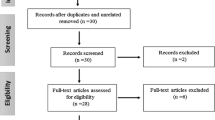
Methods
DNA samples from 40 resolved infections and 40 chronic HCV patients paired by age were analyzed. Bivariate analysis was performed to rank the importance of each contributing factor in spontaneous HCV clearance.
Results
Interestingly, 63.6% of patients with resolved infections exhibited the protective genotype CC for SNP rs12979860. Additionally, 59.3% of patients with resolved infections displayed the protective genotype TT/TT for SNP ss469415590. Moreover, a ranking of clearance factors was estimated. In order of importance, the IL28B CC genotype (OR 0.197, 95% CI 0.072–0.541) followed by the INFL4 TT/TT genotype (OR 0.237, 95% CI 0.083–0.679), and female gender (OR 0.394, 95% CI 0.159–0.977) were the main predictors for clearance of HCV infection.
Conclusions
HCV clearance is multifactorial and the contributing factors display a hierarchical order. Identifying all elements playing role in HCV clearance is of the most importance for HCV-related disease management. Dissecting the relevance of each contributing factor will certainly improve our understanding of the pathogenesis of HCV infection.
Similar content being viewed by others
References
Choo QL, Kuo G, Weiner AJ, Overby LR, Bradley DW, Houghton M (1989) Isolation of a cDNA clone derived from a blood-borne non-a, non-B viral hepatitis genome. Science 244(4902):359–362
Kato N, Hijikata M, Ootsuyama Y, Nakagawa M, Ohkoshi S, Sugimura T, Shimotohno K (1990) Molecular cloning of the human hepatitis C virus genome from Japanese patients with non-a, non-B hepatitis. Proc Natl Acad Sci U S A 87(24):9524–9528
Takamizawa A, Mori C, Fuke I, Manabe S, Murakami S, Fujita J, Onishi E, Andoh T, Yoshida I, Okayama H (1991) Structure and organization of the hepatitis C virus genome isolated from human carriers. J Virol 65(3):1105–1113
Hijikata M, Mizushima H, Akagi T, Mori S, Kakiuchi N, Kato N, Tanaka T, Kimura K, Shimotohno K (1993) Two distinct proteinase activities required for the processing of a putative nonstructural precursor protein of hepatitis C virus. J Virol 67(8):4665–4675
Kiyosawa K, Sodeyama T, Tanaka E, Gibo Y, Yoshizawa K, Nakano Y, Furuta S, Akahane Y, Nishioka K, Purcell RH, Alter HJ (1990) Interrelationship of blood transfusion, non-a, non-B hepatitis and hepatocellular carcinoma: analysis by detection of antibody to hepatitis C virus. Hepatology 12(4 Pt 1):671–675
Alter HJ, Seeff LB (2000) Recovery, persistence, and sequelae in hepatitis C virus infection: a perspective on long-term outcome. Semin Liver Dis 20(1):17–35
Lavanchy D (2009) The global burden of hepatitis C. Liver Int 29(Suppl 1):74–81
Stenkvist J, Nystrom J, Falconer K, Sonnerborg A, Weiland O (2014) Occasional spontaneous clearance of chronic hepatitis C virus in HIV-infected individuals. J Hepatol 61(4):957–961
Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST (2013) Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology 57(4):1333–1342
Amini M, Poustchi H (2012) Hepatitis C virus spontaneous clearance: immunology and genetic variance. Viral Immunol 25(4):241–248
Selvarajah S, Tobler LH, Simmons G, Busch MP (2010) Host genetic basis for hepatitis C virus clearance: a role for blood collection centers. Curr Opin Hematol 17(6):550–557
Thomas DL, Thio CL, Martin MP, Qi Y, Ge D, O’hUigin C, Kidd J, Kidd K, Khakoo SI, Alexander G, Goedert JJ, Kirk GD, Donfield SM, Rosen HR, Tobler LH, Busch MP, McHutchison JG, Goldstein DB, Carrington M (2009) Genetic variation in IL28B and spontaneous clearance of hepatitis C virus. Nature 461(7265):798–801
Seth RB, Sun L, Ea CK, Chen ZJ (2005) Identification and characterization of MAVS, a mitochondrial antiviral signaling protein that activates NF-kappaB and IRF 3. Cell 122(5):669–682
Baril M, Racine ME, Penin F, Lamarre D (2009) MAVS dimer is a crucial signaling component of innate immunity and the target of hepatitis C virus NS3/4A protease. J Virol 83(3):1299–1311
Bender S, Reuter A, Eberle F, Einhorn E, Binder M, Bartenschlager R (2015) Activation of type I and III interferon response by mitochondrial and peroxisomal MAVS and inhibition by hepatitis C virus. PLoS Pathog 11(11):e1005264
Ferreira AR, Magalhaes AC, Camoes F et al (2016) Hepatitis C virus NS3-4A inhibits the peroxisomal MAVS-dependent antiviral signalling response. J Cell Mol Med 20:750–757
Horner SM, Wilkins C, Badil S, Iskarpatyoti J, Gale M Jr (2015) Proteomic analysis of mitochondrial-associated ER membranes (MAM) during RNA virus infection reveals dynamic changes in protein and organelle trafficking. PLoS One 10(3):e0117963
Foy E, Li K, Wang C, Sumpter R Jr, Ikeda M, Lemon SM, Gale M Jr (2003) Regulation of interferon regulatory factor-3 by the hepatitis C virus serine protease. Science 300(5622):1145–1148
Li XD, Sun L, Seth RB, Pineda G, Chen ZJ (2005) Hepatitis C virus protease NS3/4A cleaves mitochondrial antiviral signaling protein off the mitochondria to evade innate immunity. Proc Natl Acad Sci U S A 102(49):17717–17722
Lin R, Lacoste J, Nakhaei P, Sun Q, Yang L, Paz S, Wilkinson P, Julkunen I, Vitour D, Meurs E, Hiscott J (2006) Dissociation of a MAVS/IPS-1/VISA/Cardif-IKKepsilon molecular complex from the mitochondrial outer membrane by hepatitis C virus NS3-4A proteolytic cleavage. J Virol 80(12):6072–6083
Galmozzi E, Vigano M, Lampertico P (2014) Systematic review with meta-analysis: do interferon lambda 3 polymorphisms predict the outcome of interferon-therapy in hepatitis B infection? Aliment Pharmacol Ther 39(6):569–578
Tillmann HL, Thompson AJ, Patel K et al (2010) A polymorphism near IL28B is associated with spontaneous clearance of acute hepatitis C virus and jaundice. Gastroenterology 139(5):1586–1592 1592 e1581
Ge D, Fellay J, Thompson AJ, Simon JS, Shianna KV, Urban TJ, Heinzen EL, Qiu P, Bertelsen AH, Muir AJ, Sulkowski M, McHutchison JG, Goldstein DB (2009) Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature 461(7262):399–401
Rauch A, Kutalik Z, Descombes P et al (2010) Genetic variation in IL28B is associated with chronic hepatitis C and treatment failure: a genome-wide association study. Gastroenterology 138(4):1338–1345 1345 e1331–1337
Tanaka Y, Nishida N, Sugiyama M, Kurosaki M, Matsuura K, Sakamoto N, Nakagawa M, Korenaga M, Hino K, Hige S, Ito Y, Mita E, Tanaka E, Mochida S, Murawaki Y, Honda M, Sakai A, Hiasa Y, Nishiguchi S, Koike A, Sakaida I, Imamura M, Ito K, Yano K, Masaki N, Sugauchi F, Izumi N, Tokunaga K, Mizokami M (2009) Genome-wide association of IL28B with response to pegylated interferon-alpha and ribavirin therapy for chronic hepatitis C. Nat Genet 41(10):1105–1109
Honda M, Sakai A, Yamashita T, Nakamoto Y, Mizukoshi E, Sakai Y, Yamashita T, Nakamura M, Shirasaki T, Horimoto K, Tanaka Y, Tokunaga K, Mizokami M, Kaneko S, Hokuriku Liver Study Group (2010) Hepatic ISG expression is associated with genetic variation in interleukin 28B and the outcome of IFN therapy for chronic hepatitis C. Gastroenterology 139(2):499–509
Prokunina-Olsson L, Muchmore B, Tang W, Pfeiffer RM, Park H, Dickensheets H, Hergott D, Porter-Gill P, Mumy A, Kohaar I, Chen S, Brand N, Tarway MA, Liu L, Sheikh F, Astemborski J, Bonkovsky HL, Edlin BR, Howell CD, Morgan TR, Thomas DL, Rehermann B, Donnelly RP, O'Brien TR (2013) A variant upstream of IFNL3 (IL28B) creating a new interferon gene IFNL4 is associated with impaired clearance of hepatitis C virus. Nat Genet 45(2):164–171
Campiotto S, Pinho JR, Carrilho FJ et al (2005) Geographic distribution of hepatitis C virus genotypes in Brazil. Braz J Med Biol Res 38(1):41–49
Tengan FM, Eluf-Neto J, Cavalheiro NP, Barone AA (2001) Sexual transmission of hepatitis C virus. Rev Inst Med Trop Sao Paulo 43(3):133–137
Provazzi PJ, Mukherjee S, Hanson AM et al (2015) Analysis of the enzymatic activity of an NS3 helicase genotype 3a variant sequence obtained from a relapse patient. PLoS One 10(12):e0144638
Johnson T, Bryder K, Corbet S, Fomsgaard A (2003) Routine genotyping of human papillomavirus samples in Denmark. APMIS 111(3):398–404
Speich N, Schmitt C, Bollmann R, Bollmann M (2004) Human papillomavirus (HPV) study of 2916 cytological samples by PCR and DNA sequencing: genotype spectrum of patients from the west German area. J Med Microbiol 53(Pt 2):125–128
Vernon SD, Unger ER, Williams D (2000) Comparison of human papillomavirus detection and typing by cycle sequencing, line blotting, and hybrid capture. J Clin Microbiol 38(2):651–655
Moreno-Estrada A, Aparicio-Prat E, Sikora M, Engelken J, Ramírez-Soriano A, Calafell F, Bosch E (2010) African signatures of recent positive selection in human FOXI1. BMC Evol Biol 10:267
Bellecave P, Sarasin-Filipowicz M, Donze O et al (2010) Cleavage of mitochondrial antiviral signaling protein in the liver of patients with chronic hepatitis C correlates with a reduced activation of the endogenous interferon system. Hepatology 51(4):1127–1136
Caporaso N, Ascione A, Stroffolini T (1998) Spread of hepatitis C virus infection within families. Investigators of an Italian Multicenter Group. J Viral Hepat 5(1):67–72
Ghosn J, Pierre-Francois S, Thibault V, Duvivier C, Tubiana R, Simon A, Valantin MA, Dominguez S, Caumes E, Katlama C (2004) Acute hepatitis C in HIV-infected men who have sex with men. HIV Med. 5(4):303–306
Horner SM, Gale M Jr (2009) Intracellular innate immune cascades and interferon defenses that control hepatitis C virus. J Interf Cytokine Res 29(9):489–498
Huang KH, Bruneau J, Shoukry N, Bernard NF (2008) Spontaneous resolution of hepatitis C virus infection is not due to a mutation at Cys-508 of MAVS/VISA/IPS-1/CARDIF. J Clin Virol 42(2):229–230
Suppiah V, Moldovan M, Ahlenstiel G et al (2009) IL28B is associated with response to chronic hepatitis C interferon-alpha and ribavirin therapy. Nat Genet 41(10):1100–1104
Vandelli C, Renzo F, Romano L, Tisminetzky S, de Palma M, Stroffolini T, Ventura E, Zanetti A (2004) Lack of evidence of sexual transmission of hepatitis C among monogamous couples: results of a 10-year prospective follow-up study. Am J Gastroenterol 99(5):855–859
Franco S, Aparicio E, Parera M, Clotet B, Tural C, Martinez MA (2014) IFNL4 ss469415590 variant is a better predictor than rs12979860 of pegylated interferon-alpha/ribavirin therapy failure in hepatitis C virus/HIV-1 coinfected patients. AIDS 28(1):133–136
Knapp S, Zakaria Z, Hashem M, Zaghla H, Khakoo SI, Waked I, Thursz M, Abdelwahab SF (2015) Influence of IFNL3.rs12979860 and IFNL4.ss469415590 polymorphism on clearance of hepatitis C virus infection among Egyptians. Hepatol Int 9(2):251–257
Covolo L, Bibert S, Donato F, Bochud PY, Lagging M, Negro F, Fattovich G (2014) The novel ss469415590 variant predicts virological response to therapy in patients with chronic hepatitis C virus type 1 infection. Aliment Pharmacol Ther 39(3):322–330
Miyamura T, Kanda T, Nakamoto S et al (2014) IFNL4 ss469415590 variant is associated with treatment response in Japanese HCV genotype 1 infected individuals treated with IFN-including regimens. Int J Hepatol 2014:723868
Stattermayer AF, Strassl R, Maieron A et al (2014) Polymorphisms of interferon-lambda4 and IL28B - effects on treatment response to interferon/ribavirin in patients with chronic hepatitis C. Aliment Pharmacol Ther 39(1):104–111
Wu R, Chi X, Wang X, Sun H, Lv J, Gao X, Yu G, Kong F, Xu H, Hua R, Jiang J, Sun B, Zhong J, Pan Y, Niu J (2016) IFNL4 ss469415590 polymorphism contributes to treatment decisions in patients with chronic hepatitis C virus genotype 1b, but not 2a, infection. Infect Genet Evol 39:132–140
Lupberger J, Felmlee DJ, Baumert TF (2013) Interferon-lambda polymorphisms and hepatitis C virus clearance revisited. Hepatology 58(1):439–441
Real LM, Neukam K, Herrero R, Guardiola JM, Reiberger T, Rivero-Juarez A, Salazar J, Mandorfer M, Merino D, Soriano V, Rivero A, Macías J, Pineda JA, Caruz A (2014) IFNL4 ss469415590 variant shows similar performance to rs12979860 as predictor of response to treatment against hepatitis C virus genotype 1 or 4 in Caucasians. PLoS One 9(4):e95515
Micallef JM, Kaldor JM, Dore GJ (2006) Spontaneous viral clearance following acute hepatitis C infection: a systematic review of longitudinal studies. J Viral Hepat 13(1):34–41
Alric L, Bonnet D, Fort M (2014) Association between female sex, IL28B genotype, but also DQB1*0301 allele and the outcome of acute hepatitis C virus infection. Hepatology 60:2127
Alric L, Fort M, Izopet J, Vinel JP, Bureau C, Sandre K, Charlet JP, Beraud M, Abbal M, Duffaut M (2000) Study of host- and virus-related factors associated with spontaneous hepatitis C virus clearance. Tissue Antigens 56(2):154–158
Terrault NA (2002) Sexual activity as a risk factor for hepatitis C. Hepatology 36(5 Suppl 1):S99–S105
Boonyarad V, Chutaputti A, Choeichareon S, Bedi K, Theamboonlers A, Chinchai T, Poovorawan Y (2003) Interspousal transmission of hepatitis C in Thailand. J Gastroenterol 38(11):1053–1059
Tahan V, Karaca C, Yildirim B, Bozbas A, Ozaras R, Demir K, Avsar E, Mert A, Besisik F, Kaymakoglu S, Senturk H, Cakaloglu Y, Kalayci C, Okten A, Tozun N (2005) Sexual transmission of HCV between spouses. Am J Gastroenterol 100(4):821–824
Gilleece YC, Browne RE, Asboe D, Atkins M, Mandalia S, Bower M, Gazzard BG, Nelson MR (2005) Transmission of hepatitis C virus among HIV-positive homosexual men and response to a 24-week course of pegylated interferon and ribavirin. J Acquir Immune Defic Syndr 40(1):41–46
Vogel M, Deterding K, Wiegand J, Grüner NH, Baumgarten A, Jung MC, Manns MP, Wedemeyer H, Rockstroh JK, German Hepatitis Group, Hep‐Net (2009) Initial presentation of acute hepatitis C virus (HCV) infection among HIV-negative and HIV-positive individuals-experience from 2 large German networks on the study of acute HCV infection. Clin Infect Dis 49(2):317–319 author reply 319
Schmidt AJ, Rockstroh JK, Vogel M, An der Heiden M, Baillot A, Krznaric I, Radun D (2011) Trouble with bleeding: risk factors for acute hepatitis C among HIV-positive gay men from Germany--a case-control study. PLoS One 6(3):e17781
Danta M, Brown D, Bhagani S, Pybus OG, Sabin CA, Nelson M, Fisher M, Johnson AM, Dusheiko GM, HIV and Acute HCV (HAAC) group (2007) Recent epidemic of acute hepatitis C virus in HIV-positive men who have sex with men linked to high-risk sexual behaviours. AIDS 21(8):983–991
van de Laar T, Pybus O, Bruisten S, Brown D, Nelson M, Bhagani S, Vogel M, Baumgarten A, Chaix ML, Fisher M, Gőtz H, Matthews GV, Neifer S, White P, Rawlinson W, Pol S, Rockstroh J, Coutinho R, Dore GJ, Dusheiko GM, Danta M (2009) Evidence of a large, international network of HCV transmission in HIV-positive men who have sex with men. Gastroenterology 136(5):1609–1617
Seaberg EC, Witt MD, Jacobson LP, Detels R, Rinaldo CR, Young S, Phair JP, Thio CL (2014) Differences in hepatitis C virus prevalence and clearance by mode of acquisition among men who have sex with men. J Viral Hepat 21(10):696–705
Ingiliz P, Krznaric I, Stellbrink HJ, Knecht G, Lutz T, Noah C, Stocker H, Obermeier M, Dupke S, Boesecke C, Rockstroh JK, Baumgarten A, Hoffmann C (2014) Multiple hepatitis C virus (HCV) reinfections in HIV-positive men who have sex with men: no influence of HCV genotype switch or interleukin-28B genotype on spontaneous clearance. HIV Med 15(6):355–361
Vanhommerig JW, Thomas XV, van der Meer JT et al (2014) Hepatitis C virus (HCV) antibody dynamics following acute HCV infection and reinfection among HIV-infected men who have sex with men. Clin Infect Dis 59(12):1678–1685
Funding
This work was supported by Foundation for Research Support of the State of São Paulo (FAPESP - 2014/22198-0) and the Brazilian National Council for Scientific and Technological Development (CNPq - 2015/34857; 2010/15686).
Author information
Authors and Affiliations
Contributions
PJSP, PR, LMGR, GV, and BMC wrote of the manuscript. PJSP, PR, and MLN conceived and designed the experiments; PJSP, BMC, VCM, PCRR, LRC, and STQA performed the experiments; RMF, RMTG, GFS, CRV, and PSN performed the management of samples collection and patients’ data; PJSP, PR, LMGR, BMC, and JAC analyzed the data.
Corresponding author
Ethics declarations
The project was approved by the in-house Ethics Committee of Sao Paulo State University (IBILCE-UNESP, São José do Rio Preto) (No. 049/09), and all participants signed an informed consent form.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Responsible Editor: Giliane Trindade
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Provazzi, P.J.S., Rossi, L.M.G., Carneiro, B.M. et al. Hierarchical assessment of host factors influencing the spontaneous resolution of hepatitis C infection. Braz J Microbiol 50, 147–155 (2019). https://doi.org/10.1007/s42770-018-0008-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-018-0008-3