Abstract
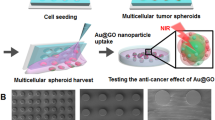
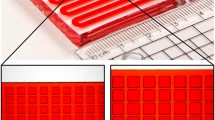
Drug resistance is one of the major obstacles in the drug therapy of cancers. Efforts in this area in pre-clinical research have focused on developing novel platforms to evaluate and decrease drug resistance. In this paper, inspired by the structure of hives where swarms live and breed, we propose porous hydrogel arrays with a uniform pore structure for the generation of hepatoma cell spheroids and the investigation of drug resistance. The porous hydrogel arrays were fabricated using polyethylene glycol diacrylate (PEGDA) hydrogel to negatively replicate a well-designed template. Benefiting from the elaborate processing of the template, the prepared porous hydrogel arrays possessed a uniform pore structure. Due to their anti-adhesion properties and the excellent biocompatibility of the PEGDA hydrogel, the hepatoma cells could form well-defined and uniform hepatoma cell spheroids in the porous hydrogel arrays. We found that the resistant hepatoma cell spheroids showed more significant Lenvatinib resistance and a migratory phenotype compared with a two-dimensional (2D) cell culture, which reveals the reason for the failure of most 2D cell-selected drugs for in vivo applications. These features give such porous hydrogel arrays promising application prospects in the investigation of tumor cell spheroid culture and in vitro drug resistance.





Similar content being viewed by others
References
Vasan N, Baselga J, Hyman DM (2019) A view on drug resistance in cancer. Nature 575:299–309. https://doi.org/10.1038/s41586-019-1730-1
Liu XZ, Zhang HB, Cheng RY et al (2018) An immunological electrospun scaffold for tumor cell killing and healthy tissue regeneration. Mater Horizons 5:1082–1091. https://doi.org/10.1039/c8mh00704g
Boumahdi S, de Sauvage FJ (2020) The great escape: tumour cell plasticity in resistance to targeted therapy. Nat Rev Drug Discov 19:39–56. https://doi.org/10.1038/s41573-019-0044-1
Liu J, Ye ZL, Xiang MX et al (2019) Functional extracellular vesicles engineered with lipid-grafted hyaluronic acid effectively reverse cancer drug resistance. Biomaterials 223:119475. https://doi.org/10.1016/j.biomaterials.2019.119475
Zhang H, Liu YX, Chen GP et al (2020) Immunotherapeutic silk inverse opal particles for post-surgical tumor treatment. Sci Bull 65:380–388. https://doi.org/10.1016/j.scib.2019.10.023
Friedmann Angeli JP, Krysko DV, Conrad M (2019) Ferroptosis at the crossroads of cancer-acquired drug resistance and immune evasion. Nat Rev Cancer 19:405–414. https://doi.org/10.1038/s41568-019-0149-1
Liu L, Tian XH, Ma Y (2018) A versatile dynamic mussel-inspired biointerface: from specific cell behavior modulation to selective cell isolation. Angew Chem 57:7878–7882. https://doi.org/10.1002/anie.201804802
Li JN, Xu WG, Li D et al (2018) Locally deployable nanofiber patch for sequential drug delivery in treatment of primary and advanced orthotopic hepatomas. ACS Nano 12:6685–6699. https://doi.org/10.1021/acsnano.8b01729
Wang YM, Wu D, Wu GH et al (2020) Metastasis-on-a-chip mimicking the progression of kidney cancer in the liver for predicting treatment efficacy. Theranostics 10:300–311. https://doi.org/10.7150/thno.38736
Muraca F, Alahmari A, Giannone VA et al (2019) A three-dimensional cell culture platform for long time-scale observations of bio-nano interactions. ACS Nano 13:13524–13536. https://doi.org/10.1021/acsnano.9b07453
Hassan S, Sebastian S, Maharjan S et al (2020) Liver-on-a-chip models of fatty liver disease. Hepatology 71:733–740. https://doi.org/10.1002/hep.31106
Zhang HB, Cui WG, Qu XM et al (2019) Photothermal-responsive nanosized hybrid polymersome as versatile therapeutics codelivery nanovehicle for effective tumor suppression. PNAS 116:7744–7749. https://doi.org/10.1073/pnas.1817251116
Roberge CL, Kingsley DM, Faulkner DE (2020) Non-destructive tumor aggregate morphology and viability quantification at cellular resolution, during development and in response to drug. Acta Biomater 117:322–334. https://doi.org/10.1016/j.actbio.2020.09.042
Li SS, Ip CKM, Tang MYH et al (2019) Sialyl Lewisx-P-selectin cascade mediates tumor-mesothelial adhesion in ascitic fluid shear flow. Nat Commun 1:2406. https://doi.org/10.1038/s41467-019-10334-6
Lee YB, Kim EM, Byun H et al (2018) Engineering spheroids potentiating cell-cell and cell-ECM interactions by self-assembly of stem cell microlayer. Biomaterials 165:105–120. https://doi.org/10.1016/j.biomaterials.2018.02.049
Shao CM, Liu YX, Chi JJ et al (2019) Responsive inverse opal scaffolds with biomimetic enrichment capability for cell culture. Research 2019:9783793. https://doi.org/10.34133/2019/9783793
Wu GH, Wu D, Lo J et al (2020) A bioartificial liver support system integrated with a DLM/GelMA-based bioengineered whole liver for prevention of hepatic encephalopathy via enhanced ammonia reduction. Biomater Sci 8:2814–2824. https://doi.org/10.1039/c9bm01879d
Chao YC, Shum HC (2020) Emerging aqueous two-phase systems: from fundamentals of interfaces to biomedical applications. Chem Soc Rev 49:114–142. https://doi.org/10.1039/c9cs00466a
Rebelo SP, Pinto C, Martins TR et al (2018) 3D–3-culture: a tool to unveil macrophage plasticity in the tumour microenvironment. Biomaterials 163:185–197. https://doi.org/10.1016/j.biomaterials.2018.02.030
Zhang LY, Chen KW, Zhang HY et al (2018) Microfluidic templated multicompartment microgels for 3D encapsulation and pairing of single cells. Small 14:1702955. https://doi.org/10.1002/smll.201702955
Zhang LC, Xiang Y, Zhang HB et al (2020) A biomimetic 3D-self-forming approach for microvascular scaffolds. Adv Sci 7:1903553. https://doi.org/10.1002/advs.201903553
Hortelão AC, Carrascosa R, Murillo-Cremaes N et al (2019) Targeting 3D bladder cancer spheroids with urease-powered nanomotors. ACS Nano 13:429–439. https://doi.org/10.1021/acsnano.8b06610
Li WC, Liu XB, Deng ZS et al (2019) Tough bonding, on-demand debonding, and facile rebonding between hydrogels and diverse metal surfaces. Adv Mater 31:e1904732. https://doi.org/10.1002/adma.201904732
Cai YL, Wu FY, Yu YR et al (2019) Porous scaffolds from droplet microfluidics for prevention of intrauterine adhesion. Acta Biomater 84:222–230. https://doi.org/10.1016/j.actbio.2018.11.016
Sun XM, Zhang HB, He JL et al (2018) Adjustable hardness of hydrogel for promoting vascularization and maintaining sternness of stem cells in skin flap regeneration. Appl Mater Today 13:54–63. https://doi.org/10.1016/j.apmt.2018.08.007
An CF, Liu WJ, Zhang Y et al (2020) Continuous microfluidic encapsulation of single mesenchymal stem cells using alginate microgels as injectable fillers for bone regeneration. Acta Biomater 111:181–196. https://doi.org/10.1016/j.actbio.2020.05.024
Chen KW, Fen YYF, Zhang Y et al (2019) Entanglement-driven adhesion, self-healing, and high stretchability of double-network PEG-based hydrogels. ACS Appl Mater Interf 11:36458–36468. https://doi.org/10.1021/acsami.9b14348
Shao CM, Chi JJ, Zhang H et al (2020) Development of cell spheroids by advanced technologies. Adv Mater Technol 5:2000183. https://doi.org/10.1002/admt.202000183
Faivre S, Rimassa L, Finn RS (2020) Molecular therapies for HCC: looking outside the box. J Hepatol 72:342–352. https://doi.org/10.1016/j.jhep.2019.09.010
Stemmler MP, Eccles RL, Brabletz S (2019) Non-redundant functions of EMT transcription factors. Nat Cell Biol 21:102–112. https://doi.org/10.1038/s41556-018-0196-y
Wang L, Chang Y, Feng YL (2019) Nitric oxide stimulated programmable drug release of nanosystem for multidrug resistance cancer therapy. Nano Lett 19:6800–6811. https://doi.org/10.1021/acs.nanolett.9b01869
Dastvan R, Mishra S, Peskova YB et al (2019) Mechanism of allosteric modulation of p-glycoprotein by transport substrates and inhibitors. Science 364:689–692. https://doi.org/10.1126/science.aav9406
Erin N, Grahovac J, Brozovic A et al (2020) Tumor microenvironment and epithelial mesenchymal transition as targets to overcome tumor multidrug resistance. Drug Resist Updat 53:100715. https://doi.org/10.1016/j.drup.2020.100715
Acknowledgements
This work was supported by the National Key Research and Development Program of China (No. 2020YFA0908200), the National Natural Science Foundation of China (Nos. 52073060, 61927805, 81974312, and 81501823), the Natural Science Foundation of Jiangsu Province (No. BE2018707), the Shenzhen Fundamental Research Program (No. JCYJ20190813152616459), the Zhejiang Provincial Natural Science Foundation of China (Nos. LY18H160049 and LQ19H160008), the Medical Scientific Research of Zhejiang Province (No. 2017KY459), Wenzhou Municipal Science and Technology Bureau (No. Y20190203), and Wenzhou Institute, University of Chinese Academy of Sciences’s startup fund (No. WIUCASQD2019007).
Author information
Authors and Affiliations
Contributions
YJZ was involved in conceptualization; XL was involved in data curation analyzed, investigation, writing—original draft; XL and CMS contributed to formal analysis, validation, writing—review & editing and visualization; XS, LS, and KQS contributed to the project administration and supervision.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human or animal subjects performed by any of the authors.
Consent to participate
All authors agree to participate in the work related to this article.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 368 kb)
Rights and permissions
About this article
Cite this article
Lei, X., Shao, C., Shou, X. et al. Porous hydrogel arrays for hepatoma cell spheroid formation and drug resistance investigation. Bio-des. Manuf. 4, 842–850 (2021). https://doi.org/10.1007/s42242-021-00141-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42242-021-00141-8