Abstract
Objective
To assess maternal and neonatal outcomes in women with or without preexisting diabetes mellitus (DM) undergoing assisted reproduction technology (ART) treatment.
Methods
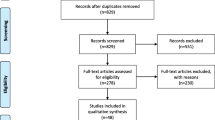
Prospective or retrospective controlled trials reporting on women with or without preexisting DM undergoing ART treatment were considered eligible. Twelve electronic databases were systematically searched up to December 2020. The risk of bias was assessed by the Cochrane Risk OF Bias In Non-randomized Studies of Interventions (ROBINS-I) tool. Each primary outcome was extracted and pooled as maternal- or neonatal-related.
Results
Two studies were included in the systematic review, reporting on both maternal- and neonatal-related parameters after ART treatment. Due to the limited data, no meta-analysis was conducted. Preterm birth, placenta previa, and excessive bleeding during pregnancy were observed more often in pregnancies complicated by preexisting DM conceived by ART compared with pregnancies without DM. There was no difference in the risk for placental abruption between the groups. Regarding the neonatal outcomes, large-for-gestational-age (LGA) embryos and neonatal intensive care unit (NICU) admission were more commonly reported for women with preexisting DM. In one study, preexisting DM was marginally associated with infant mortality.
Conclusions
Despite the scarce data, preexisting DM in pregnancies conceived by ART is associated with increased risk for maternal and neonatal complications.
Trial registration
Registered in PROSPERO (registration number: 143187).

Similar content being viewed by others
References
Cunningham J (2017) Infertility: a primer for primary care providers. JAAPA 30(9):19–25
Jenabi E, Seyedi M, Hamzehei R, Bashirian S, Rezaei M, Razjouyan K, Khazaei S (2020) Association between assisted reproductive technology and autism spectrum disorders in Iran: a case-control study. Clin Exp Pediatr 63(9):368–372
Yenice MG, Danacıoğlu YO, Mert M, Karakaya P, Seker KG, Akkaş F, Şimşek A, Şahin S, Taşçı AI (2020) Evaluation of factors affecting sexual dysfunction in female patients with diabetes mellitus. Arch Endocrinol Metab 64(3):319–325
Solis-Herrera C, Triplitt C, Reasner C, DeFronzo RA, Cersosimo E. Classification of diabetes mellitus. Endotext 2018.
Tefera YG, Gebresillassie BM, Emiru YK, Yilma R, Hafiz F, Akalu H, Ayele AA. Diabetic health literacy and its association with glycemic control among adult patients with type 2 diabetes mellitus attending the outpatient clinic of a university hospital in Ethiopia. PLoS One 2020;15(4).
Wellons MF, Matthews JJ, Kim C (2017) Ovarian aging in women with diabetes: an overview. Maturitas 96:109–113
Avci R, Whittington JR, Blossom SJ, Escalona-Vargas D, Siegel ER, Preissl HT, Eswaran H. Studying the effect of maternal pregestational diabetes on fetal neurodevelopment using magnetoencephalography. Clin EEG Neurosci 2020;1550059420909658.
Ebbing C, Kessler J, Moster D, Rasmussen S (2020) Single umbilical artery and risk of congenital malformation: population-based study in Norway. Ultrasound Obstet Gynecol 55:510–515
Al-Qahtani S, Heath A, Quenby S, Dawood F, Floyd R, Burdyga T, Wray S (2012) Diabetes is associated with impairment of uterine contractility and high caesarean section rate. Diabetologia 55:489–498
El-Achi V, de Vries B, O’Brien C, Park F, Tooher J, Hyett J (2020) First-trimester prediction of preterm prelabour rupture of membranes. Fetal Diagn Ther 8:1–6
Kouhkan A, Khamseh ME, Pirjani R, Moini A, Arabipoor A, Maroufizadeh S, Hosseini R, Baradaran HR (2018) Obstetric and perinatal outcomes of singleton pregnancies conceived via assisted reproductive technology complicated by gestational diabetes mellitus: a prospective cohort study. BMC Pregnancy Childbirth 18:495
Luke B, Stern JE, Kotelchuck M, Declercq ER, Anderka M, Diop H (2016) Birth outcomes by infertility treatment: analyses of the population-based cohort: Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART). J Reprod Med 61:114–127
Xu XK, Wang YA, Li Z, Lui K, Sullivan EA (2014) Risk factors associated with preterm birth among singletons following assisted reproductive technology in Australia 2007–2009–a population-based retrospective study. BMC Pregnancy Childbirth 14:406
Luke B, Brown MB, Wantman E, Seifer DB, Sparks AT, Lin PC, Doody KJ, Van Voorhis BJ, Spector LG (2019) Risk of prematurity and infant morbidity and mortality by maternal fertility status and plurality. J Assist Reprod Genet 36:121–138
Márton V, Zádori J, Kozinszky Z, Keresztúri A (2016) Prevalences and pregnancy outcome of vanishing twin pregnancies achieved by in vitro fertilization versus natural conception. Fertil Steril 106:1399–1406
Razem K, Tul N, Verdenik I, Vidmar Simic M, Blickstein I (2019) Maternal characteristics of preterm singleton birth following assisted reproduction: a population-based study. J Matern Fetal Neonatal Med 29:1–3
Higgins JPT, Green S (eds) (2011) Cochrane handbook for systematic reviews of interventions. Version 5.1.0, updated March 2011. The Cochrane Collaboration. Available at: http://handbook.cochrane.org/. Accessed Oct 2020
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1-34
Beller EM, Glasziou PP, Altman DG, Hopewell S, Bastian H, Chalmers I, Gøtzsche PC, Lasserson T, Tovey D, PRISMA for Abstracts Group (2013) PRISMA for Abstracts: reporting systematic reviews in journal and conference abstracts. PLoS Med 10:e1001419
Sterne JA et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:4919
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L (2008) Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol 61:991–996
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in metaanalysis detected by a simple, graphical test. BMJ 315:629–634
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56:455–463
Guyatt GH, Oxman AD, Schünemann H, Tugwell P, Knottnerus A (2011) GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol 64:380–382
Schieve LA, Cohen B, Nannini A, Ferre C, Reynolds MA, Zhang Z, Jeng G, Macaluso M, Wright VC (2007) A population-based study of maternal and perinatal outcomes associated with assisted reproductive technology in Massachusetts. Matern Child Health J 11(6):517–525
Jauniaux E, Englert Y, Vanesse M, Hiden M, Wilkin P (1990) Pathologic features of placentas from singleton pregnancies obtained by in vitro fertilization and embryo transfer. Obstet Gynecol 76:61–64
Sazonova A, Kallen K, Thurin-Kjellberg A, Wennerholm U-B, Bergh C (2011) Obstetric outcome after in vitro fertilization with single or double embryo transfer. Hum Reprod 26:442–450
Helmerhorst FM, Perquin DAM, Donker D, Keirse MJNC (2004) Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ 31:328
Ban Frangez H, Korosec S, Verdenik I, Kotar V, Kladnik U, Vrtacnik BE (2014) Preterm delivery risk factors in singletons born after in vitro fertilization procedures. Eur J Obstet Gynecol Reprod Biol 176:183–186
Poon LC, Shennan A, Hyett JA, Kapur A, Hadar E, Divakar H, McAuliffe F, da Silva CF, von Dadelszen F, McIntyre HD, Kihara AB, Di Renzo GC, Romero R, D’Alton M, Berghella V, Nicolaides KH, Hod M (2019) The International Federation of Gynecology and Obstetrics (FIGO) initiative on preeclampsia (PE): a pragmatic guide for first trimester screening and prevention. Int J Gynaecol Obstet 145:1–33
Wei HJ, Young R, Kuo IL, Liaw CM, Chiang HS, Yeh CY (2008) Abnormal preconception oral glucose tolerance test predicts an unfavorable pregnancy outcome after an in vitro fertilization cycle. Fertil Steril 90:613–618
McGrath RT, Glastras SJ, Hocking SL, Fulcher GR (2018) Large-for-gestational-age neonates in type 1 diabetes and pregnancy: contribution of factors beyond hyperglycemia. Diabetes Care 41:1821–1828
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zymperdikas, C.F., Zymperdikas, V.F., Mastorakos, G. et al. Assisted reproduction technology outcomes in women with infertility and preexisting diabetes mellitus: a systematic review. Hormones 21, 23–31 (2022). https://doi.org/10.1007/s42000-021-00329-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-021-00329-8