Key summary points
This study aims to identify differences between octogenarian (patients over 80 years old) and non-octogenarians (patients between 65 and 79 years old) in the course of acute pancreatitis.
AbstractSection FindingsThe incidence of local complications was higher in the non-octogenarian group. Mild acute pancreatitis was higher in the octogenarian group, while moderate acute pancreatitis was higher in the non-octogenarian group. There was no significant difference compared to severe cases.
AbstractSection MessageContrary to what was expected, no significant difference was observed between the octogenarian and non-octogenarian groups in terms of serious events in the course of acute pancreatitis.
Abstract
Background
In this study, we aimed to compare differences in disease course, etiology of acute pancreatitis admission to the intensive care unit, in-hospital mortality, disease severity, and local and systemic complications between patients aged ≥ 80 years (octogenarians) and patients aged between 65 and 79 years (non-octogenarians), all of whom were being followed with the diagnosis of acute pancreatitis.
Methods
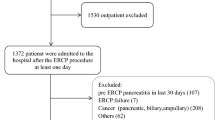
Patients aged 65 years and older with a diagnosis of acute biliary pancreatitis were included in the study. Clinical findings, routine laboratory test results, and imaging findings of all patients were reviewed retrospectively via the hospital’s records system.
Results
Of a total of 402 enrolled patients, 238 (59.2%) were female. Mean age was 77.1 ± 7.37 years. Pancreatitis after endoscopic retrograde cholangiopancreatography was detected more frequently among octogenarians than non-octogenarians (12.9% versus 5.3%, respectively; p = 0.007). Levels of blood urea nitrogen, creatinine, and total bilirubin were higher among octogenarians, while lymphocyte, calcium, and albumin levels were lower. The frequency of patients without local complications was higher among octogenarians than non-octogenarians (75.5% versus 63.6%, respectively; p = 0.013). Necrosis was less frequent in the octogenarian group than the non-octogenarian group (2.6% versus 8.9%, respectively; p = 0.012). Mild acute pancreatitis was higher in the octogenarian group, while moderate acute pancreatitis was higher in the non-octogenarian group (p = 0.028 and p = 0.012, respectively).
Conclusion
The frequencies of prolonged hospitalization, intensive care unit admission, and in-hospital mortality were similar in the octogenarian and non-octogenarian groups. In terms of disease severity, mild acute pancreatitis was higher in the octogenarian group, while moderate acute pancreatitis was higher in the non-octogenarian group.


Similar content being viewed by others
References
Barbara M, Tsen A, Rosenkranz L (2018) Acute pancreatitis in chronic dialysis patients. Pancreas 47:946–951. https://doi.org/10.1097/MPA.0000000000001119
Gloor B, Ahmed Z, Uhl W, Büchler MW (2002) Pancreatic disease in the elderly. Best Pract Res Clin Gastroenterol 16:159–170. https://doi.org/10.1053/bega.2002.0272
Somasekar K, Foulkes R, Morris-Stiff G, Hassn A (2011) Acute pancreatitis in the elderly—can we perform better? Surgeon 9:305–308. https://doi.org/10.1016/j.surge.2010.11.001
Sandblom G, Bergman T, Rasmussen I (2008) Acute pancreatitis in patients 70 years of age or older. Clin Med: Geriatr 2008:27–32
De Beaux AC, Palmer KR, Carter DC (1995) Factors influencing morbidity and mortality in acute pancreatitis; an analysis of 279 cases. Gut 37:121–126. https://doi.org/10.1136/gut.37.1.121
Gardner TB, Vege SS, Chari ST, Pearson RK, Clain JE, Topazian MD, Levy MJ, Petersen BT (2008) The effect of age on hospital outcomes in severe acute pancreatitis. Pancreatology 8:265–270. https://doi.org/10.1159/000134274
Miki C, Kusunoki M, Inoue Y, Uchida K, Mohri Y, Buckels JAC, McMaster P (2008) Remodeling of the immunoinflammatory network system in elderly cancer patients: implications of inflamm-aging and tumor-specific hyperinflammation. Surg Today 38:873–878. https://doi.org/10.1007/s00595-008-3766-y
Xin M-J, Chen H, Luo B, Sun J-B (2008) Severe acute pancreatitis in the elderly: etiology and clinical characteristics. World J Gastroenterol 14:2517–2521. https://doi.org/10.3748/wjg.14.2517
Gullo L, Migliori M, Oláh A, Farkas G, Levy P, Arvanitakis C, Lankisch P, Beger H (2002) Acute pancreatitis in five European countries: etiology and mortality. Pancreas 24:223–227. https://doi.org/10.1097/00006676-200204000-00003
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS (2013) Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut 62:102–111. https://doi.org/10.1136/gutjnl-2012-302779
Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N (1991) Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 37(3):383–393. https://doi.org/10.1016/s0016-5107(91)70740-2
Iqbal CW, Baron TH, Moir CR, Ishitani MB (2009) Post-ERCP pancreatitis in pediatric patients. J Pediatr Gastroenterol Nutr 49(4):430–434. https://doi.org/10.1097/01.mpg.0000361657.54810.19
Roberts SE, Morrison-Rees S, John A, Williams JG, Brown TH, Samuel DG (2017) The incidence and aetiology of acute pancreatitis across Europe. Pancreatology 17(2):155–165. https://doi.org/10.1016/j.pan.2017.01.005
Wenjing Pu, Luo G, Chen T, Jing L, Chen X (2021) Comparative analysis of epidemiology, etiology, and outcomes between elderly and young and middle-aged acute pancreatitis patients: a retrospective, single-center study. Eur J Gastroenterol Hepatol 33(10):1254–1259. https://doi.org/10.1097/MEG.0000000000001993
Van Steenbergen W (1996) Acute and chronic pancreatitis in the elderly patient. Tijdschr Gerontol Geriatr 27:191–196
O’Farrell A, Allwright S, Toomey D, Bedford D, Conlon K (2007) Hospital admission for acute pancreatitis in the Irish population, 1997–2004: could the increase be due to an increase in alcohol-related pancreatitis? J Public Health 29:398–404. https://doi.org/10.1093/pubmed/fdm069
Kim JE, Hwang J-H, Lee SH, Cha BH, Park YS, Kim J-W, Jeong S-H, Kim N, Dong Ho Lee JE, Hwang JH, Lee SH et al (2012) The clinical outcome of elderly patients with acute pancreatitis is not different in spite of the different etiologies and severity. Arch Gerontol Geriatr 54:256–260. https://doi.org/10.1016/j.archger.2011.01.004
Fukami Y, Kurumiya Y, Mizuno K, Sekoguchi Ei, Kobayashi S (2014) Cholecystectomy in octogenarians: be careful. Updates Surg 66:265–268. https://doi.org/10.1007/s13304-014-0267-y
Bingener J, Richards ML, Schwesinger WH, Strodel WE, Sirinek KR (2003) Laparoscopic cholecystectomy for elderly patients gold standard for golden years? Arch Surg 138(5):531–536. https://doi.org/10.1001/archsurg.138.5.531
Ding L, Yang Y, Li H, Wang H, Gao P (2020) Circulating lymphocyte subsets induce secondary infection in acute pancreatitis. Front Cell Infect Microbiol 2020(10):128. https://doi.org/10.3389/fcimb.2020.00128
Tavares SMQMC, de Lima Bravo W Jr, Silva MRLE (2014) Normal lymphocyte immunophenotype in an elderly population. Rev Bras Hematol Hemoter 36(3):180–183. https://doi.org/10.1016/j.bjhh.2014.03.021
Cabrerizo S, Cuadras D, Gomez-Busto F, Artaza-Artabe I, Marín-Ciancas F, Malafarina V (2015) Serum albumin and health in older people: review and meta analysis. Maturitas 81(1):17–27. https://doi.org/10.1016/j.maturitas.2015.02.009
Baeza-Zapata AA, García-Compean D, Jaquez-Quintana JO (2021) Acute pancreatitis in elderly patients. Gastroenterology 161(6):1736–1740. https://doi.org/10.1053/jigastro.2021.06.081
Roulin D, Girardet R, Duran R, Hajdu S, Denys A, Halkic N, Demartines N, Melloul E (2018) Outcome of elderly patients after acute biliary pancreatitis. Biosci Trends 12:54–59. https://doi.org/10.5582/bst.2017.01303
Koziel D, Gluszek-Osuch M, Suliga E, Zak M, Gluszek S (2019) Elderly persons with acute pancreatitis—specifics of the clinical course of the disease. Clin Interv Aging 14:33–41. https://doi.org/10.2147/CIA.S188520
Kayar RD, Konur Ş (2020) Clinical outcomes of acute pancreatitis in elderly patients: an experience of single tertiary center. Pancreatology 20(7):1296–1301. https://doi.org/10.1016/j.pan.2020.06.006
Quero MC, Fiorillo C et al (2019) Acute pancreatitis in elderly patients: a single-center retrospective evaluation of clinical outcomes. Scand J Gastroenterol 54(4):492–549. https://doi.org/10.1080/00365521.2019.1588369
Company L, Saez J, Martinez J, Aparicio JR, Laveda R, Grino P, Perez-Mateo M (2003) Factors predicting mortality in severe acute pancreatitis. Pancreatology 3(2):144–148. https://doi.org/10.1159/000070083
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Human and animal rights
The study was conducted in the Health Sciences University Ankara City Hospital in accordance with the Declaration of Helsinki and it received approval from Ankara City Hospital Ethics Committee No. 2 (dated 01/09/2021 and numbered E2-21-806).
Informed consent
For this type of study, consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Şahiner, E.S., Acehan, F., Inan, O. et al. Characteristics and clinical outcomes of patients over 80 years of age with acute pancreatitis. Eur Geriatr Med 13, 1013–1022 (2022). https://doi.org/10.1007/s41999-022-00631-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-022-00631-7