Key summary points
Examine characteristics of older patients presenting to the ED triaged with the presentational flowchart ‘unwell adult’ of the Manchester triage system (MTS) and to assess the different mortality and admission rates among triage categories.
AbstractSection FindingsOlder patients assigned to the ‘unwell’ flowchart have the highest non-trauma mortality rate, independent of urgency category, and highest admission rates of all presenting complaints. Surprisingly, mortality was also observed in the lowest triage categories.
AbstractSection MessagePatients in the category ‘unwell’ have the highest non-trauma 30-day mortality and highest hospital admission rates when compared to other presenting complaints, indicating that the nonspecific disease presentation "unwell" is a serious medical condition.
Abstract
Purpose
Older people often present to the Emergency Department with nonspecific complaints. We aimed (1) to examine characteristics of older patients presenting to the ED triaged with the presentational flowchart ‘unwell adult’ of the Manchester triage system (MTS) and (2) to assess the different mortality and admission rates among triage categories.
Methods
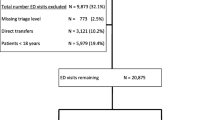
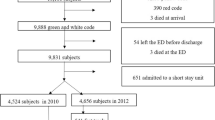
Retrospective cohort study including all consecutive patients aged 70 years and older who visited the ED of a tertiary care hospital in the Netherlands during a 1-year period. The primary outcome was 30-day mortality. Secondary outcomes were 7-day mortality, hospital admission and ED length of stay.
Results
4255 patients were included in this study. Mean age was 78 years (IQR 73.9–83.4) and 2098 were male (49.3%). The MTS presentational flowchart ‘unwell adult’ was the most commonly used flowchart (n = 815, 19.3%). After the infrequent flowchart ‘major trauma’ (n = 9, 13.8%), ‘unwell adult’ had the highest 30-day mortality (n = 88, 10.8%). When compared to all other flowcharts, patients assigned as ‘unwell adult’ have significantly higher 30-day mortality rates (OR 1.89 (95%CI 1.46–2.46), p = < 0.001), also when adjusted for age, gender and triage priority (OR 1.75 (95%CI 1.32–2.31), p = < 0.001). Patients from the ‘unwell adult’ flowchart had the highest hospital admission rate (n = 540, 66.3%), and had among the longest ED length of stay.
Conclusions
Older ED patients are most commonly assigned the presentational flowchart ‘unwell adult’ when using the MTS. Patients in this category have the highest non-trauma mortality and highest hospital admission rates when compared to other presenting complaints.


Similar content being viewed by others
Availability of data
Data are available upon reasonable request through the corresponding author.
References
Kuriyama A, Urushidani S, Nakayama T (2017) Five-level emergency triage systems: variation in assessment of validity. Emerg Med J 34(11):703–710. https://doi.org/10.1136/emermed-2016-206295
Mackway-Jones K (1997) Manchester Triage Group: emergency triage. BMJ Publishing Group, London
Parenti N, Reggiani ML, Iannone P, Percudani D, Dowding D (2014) A systematic review on the validity and reliability of an emergency department triage scale, the Manchester Triage System. Int J Nurs Stud 51(7):1062–1069. https://doi.org/10.1016/j.ijnurstu.2014.01.013
Nonnenmacher CL, Pires AUB, Moraes VM, Lucena AF (2017) Factors that influence care priority for chest pain patients using the manchester triage system. J Clin Nurs. https://doi.org/10.1111/jocn.14011
Graff I, Goldschmidt B, Glien P, Dolscheid-Pommerich RC, Fimmers R, Grigutsch D (2017) Validity of the Manchester Triage System in patients with sepsis presenting at the ED: a first assessment. Emerg Med J 34(4):212–218. https://doi.org/10.1136/emermed-2015-205309
Zachariasse JM, Seiger N, Rood PP, Alves CF, Freitas P, Smit FJ et al (2017) Validity of the Manchester Triage System in emergency care: a prospective observational study. PLoS ONE 12(2):e0170811. https://doi.org/10.1371/journal.pone.0170811
Brutschin V, Kogej M, Schacher S, Berger M, Graff I (2021) The presentational flow chart “unwell adult” of the Manchester Triage System-Curse or blessing? PLoS ONE 16(6):e0252730. https://doi.org/10.1371/journal.pone.0252730
Wallgren UM, Antonsson VE, Castren MK, Kurland L (2016) Longer time to antibiotics and higher mortality among septic patients with non-specific presentations–a cross sectional study of Emergency Department patients indicating that a screening tool may improve identification. Scand J Trauma Resusc Emerg Med 24:1. https://doi.org/10.1186/s13049-015-0193-0
Raven W, van den Hoven EMP, Gaakeer MI, Ter Avest E, Sir O, Lameijer H et al (2021) The association between presenting complaints and clinical outcomes in emergency department patients of different age categories. Eur J Emerg Med. https://doi.org/10.1097/MEJ.0000000000000860
Safwenberg U, Terent A, Lind L (2007) The Emergency Department presenting complaint as predictor of in-hospital fatality. Eur J Emerg Med 14(6):324–331. https://doi.org/10.1097/MEJ.0b013e32827b14dd
Bingisser R, Dietrich M, Nieves Ortega R, Malinovska A, Bosia T, Nickel CH (2017) Systematically assessed symptoms as outcome predictors in emergency patients. Eur J Intern Med 45:8–12. https://doi.org/10.1016/j.ejim.2017.09.013
Djarv T, Castren M, Martenson L, Kurland L (2015) Decreased general condition in the emergency department: high in-hospital mortality and a broad range of discharge diagnoses. Eur J Emerg Med 22(4):241–246. https://doi.org/10.1097/MEJ.0000000000000164
Karakoumis J, Nickel CH, Kirsch M, Rohacek M, Geigy N, Muller B et al (2015) Emergency presentations with nonspecific complaints-the burden of morbidity and the spectrum of underlying disease: nonspecific complaints and underlying disease. Medicine 94(26):e840. https://doi.org/10.1097/MD.0000000000000840
Kemp K, Mertanen R, Laaperi M, Niemi-Murola L, Lehtonen L, Castren M (2020) Nonspecific complaints in the emergency department—a systematic review. Scand J Trauma Resusc Emerg Med 28(1):6. https://doi.org/10.1186/s13049-020-0699-y
Wachelder J, Stassen PM, Fourmanov RS, Nickel CH, Haak HR (2019) Higher in-hospital mortality in patients with nonspecific complaints presenting to the emergency department. Acute Med J 18(4):232–238
Grossmann FF, Zumbrunn T, Frauchiger A, Delport K, Bingisser R, Nickel CH (2012) At risk of undertriage? Testing the performance and accuracy of the emergency severity index in older emergency department patients. Ann Emerg Med 60(3):317–25.e3. https://doi.org/10.1016/j.annemergmed.2011.12.013
Hofman SE, Lucke JA, Heim N, de Gelder J, Fogteloo AJ, Heringhaus C et al (2016) Prediction of 90-day mortality in older patients after discharge from an emergency department: a retrospective follow-up study. BMC Emerg Med 16(1):26. https://doi.org/10.1186/s12873-016-0090-5
Lucke JA, Gelder J, Clarijs F, Heringhaus C, de Craen AJM, Fogteloo AJ et al (2017) Early prediction of hospital admission for emergency department patients: a comparison between patients younger or older than 70 years. Emerg Med J. https://doi.org/10.1136/emermed-2016-205846
Bhalla MC, Wilber ST, Stiffler KA, Ondrejka JE, Gerson LW (2014) Weakness and fatigue in older ED patients in the United States. Am J Emerg Med 32(11):1395–1398. https://doi.org/10.1016/j.ajem.2014.08.027.
Malinovska A, Nickel CH, Bingisser R (2018) Trajectories of survival in patients with nonspecific complaints. Eur J Intern Med 55:e17–e18. https://doi.org/10.1016/j.ejim.2018.06.020
Graff I, Goldschmidt B, Glien P, Bogdanow M, Fimmers R, Hoeft A et al (2014) The German Version of the Manchester Triage System and its quality criteria–first assessment of validity and reliability. PLoS ONE 9(2):e88995. https://doi.org/10.1371/journal.pone.0088995
Hendin A, Eagles D, Myers V, Stiell IG (2018) Characteristics and outcomes of older emergency department patients assigned a low acuity triage score. CJEM 20:1–8. https://doi.org/10.1017/cem.2018.17
Romero-Ortuno R, Wallis S, Biram R, Keevil V (2016) Clinical frailty adds to acute illness severity in predicting mortality in hospitalized older adults: an observational study. Eur J Intern Med 35:24–34. https://doi.org/10.1016/j.ejim.2016.08.033
Blomaard LC, Speksnijder C, Lucke JA, de Gelder J, Anten S, Schuit SCE et al (2020) Geriatric screening, triage urgency, and 30-day mortality in older emergency department patients. J Am Geriatr Soc 68(8):1755–1762. https://doi.org/10.1111/jgs.16427
Kaeppeli T, Rueegg M, Dreher-Hummel T, Brabrand M, Kabell-Nissen S, Carpenter CR et al (2020) Validation of the clinical frailty scale for prediction of thirty-day mortality in the emergency department. Ann Emerg Med 76(3):291–300. https://doi.org/10.1016/j.annemergmed.2020.03.028
Funding
No specific funding was obtained for this study, authors received grants for other work. Institute for Evidence-based Medicine in Old Age (ZonMw project number 627003001) and Acutely Presenting Older Patient study (ZonMw project number 627005001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest reported by the authors of this study.
Ethical approval
The Medical Ethics Committee of the Leiden University Medical Center waived the need for approval of this study.
Informed consent
Informed consent is not applicable. Because the medical ethics committee waived the need for approval, they also waived the need for informed consent. Data were obtained from the electronic patient files.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lucke, J.A., Mooijaart, S.P., Conroy, S. et al. Mortality risk for different presenting complaints amongst older patients assessed with the Manchester triage system. Eur Geriatr Med 13, 323–328 (2022). https://doi.org/10.1007/s41999-021-00568-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00568-3