Key Summary points
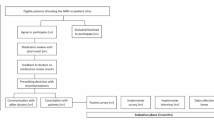
A modified Delphi study was conducted to (1) identify intervention elements that are considered by geriatricians to be important in optimizing prescribing for older adults with multimorbidity, and (2) to select the accompanying behavior change techniques to be incorporated into a context-relevant intervention to support prescribing.
AbstractSection FindingsIntervention elements such as medication review identified by the Delphi panel mirrored results from a previous scoping review. Statements involving roles of pharmacists selected by the panel validated findings in the literature that pharmacists play important collaborative roles to help reduce potentially inappropriate prescribing among older adults with multimorbidity.
AbstractSection MessageWe identified relevant intervention elements and their accompanying behavior change techniques to aid in the development of a context-specific intervention.
Abstract
Purpose
Potentially inappropriate prescribing among older adults is a rising concern, attributed mainly by polypharmacy and multimorbidity. We aimed to identify key components and strategies for construction of a context-relevant intervention to facilitate appropriate prescribing in outpatient clinics in Singapore.
Methods
The modified Delphi study was conducted in two rounds with 20 geriatricians from seven public hospitals in Singapore. Round one survey presented 69 statements formulated from a scoping review, while round two presented 23 statements with some modifications based on round one comments. The statements were rated against a 7-point Likert scale on their importance and impact on prescribing for older adults with multimorbidty.
Results
Consensus were achieved for 90% of the statements. Seven intervention elements were identified as being important: medication review, training, medication therapy management, shared decision making, patient interview, medication reconciliation, comprehensive geriatric assessment. In addition, some commonly identified behavior change techniques included goal setting (behavior), goal setting (outcome) and problem solving.
Conclusions
This study identified important intervention elements and their potential strategies that could be adopted in an intervention to optimize appropriate prescribing for older adults with multimorbidity.

Similar content being viewed by others
Data availability
All data generated and analyzed for this study are available within the article and its supplementary information.
Code availability
Not applicable.
References
Who.int (2018) Ageing and health. World Health Organization (WHO). https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed 26 Jan 2021
National Population and Talent Division, Strategy Group, Prime Minister’s Office, Singapore Department of Statistics, Ministry of Home Affairs, Immigration & Checkpoints Authority, Ministry of Manpower (2020) Population in Brief 2020. https://www.strategygroup.gov.sg/files/media-centre/publications/population-in-brief-2020.pdf. Accessed 26 Jan 2021
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE (2017) What is polypharmacy? A systematic review of definitions. BMC Geriatr 17(1):1–10. https://doi.org/10.1186/s12877-017-0621-2
Salive ME (2013) Multimorbidity in older adults. Epidemiol Rev 35(1):75–83. https://doi.org/10.1093/epirev/mxs009
Midão L, Giardini A, Menditto E, Kardas P, Costa E (2018) Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch Gerontol Geriatr 78:213–220. https://doi.org/10.1016/j.archger.2018.06.018
Cahir C, Fahey T, Teeling M, Teljeur C, Feely J, Bennett K (2010) Potentially inappropriate prescribing and cost outcomes for older people: a national population study. Br J Clin Pharmacol 69(5):543–552. https://doi.org/10.1111/j.1365-2125.2010.03628.x
Bradley MC, Motterlini N, Padmanabhan S, Cahir C, Williams T, Fahey T, Hughes CM (2014) Potentially inappropriate prescribing among older people in the United Kingdom. BMC Geriatr 14(1):1–9. https://doi.org/10.1186/1471-2318-14-72
Kaufmann CP, Tremp R, Hersberger KE, Lampert ML (2014) Inappropriate prescribing: a systematic overview of published assessment tools. Eur J Clin Pharmacol 70(1):1–11. https://doi.org/10.1007/s00228-013-1575-8
Maher RL, Hanlon J, Hajjar ER (2014) Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf 13(1):57–65. https://doi.org/10.1517/14740338.2013.827660
By the American Geriatrics Society 2015 Beers Criteria Update Expert Panel (2015) American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 63(11):2227–2246. https://doi.org/10.1111/jgs.13702
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P (2015) STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 44(2):213–218. https://doi.org/10.1093/ageing/afu145
Bahat G, Bay I, Tufan A, Tufan F, Kilic C, Karan MA (2017) Prevalence of potentially inappropriate prescribing among older adults: a comparison of the beers 2012 and screening tool of older person’s prescriptions criteria version 2. Geriatr Gerontol Int 17(9):1245–1251. https://doi.org/10.1111/ggi.12850
Tan YW, Suppiah S, Bautista MAC, Malhotra R (2019) Polypharmacy among community-dwelling elderly in Singapore: prevalence, risk factors and association with medication non-adherence. Proc Singapore Healthc 28(4):224–231. https://doi.org/10.1177/2010105819868485
Mangin D, Bahat G, Golomb BA, Mallery LH, Moorhouse P, Onder G et al (2018) International Group for Reducing Inappropriate Medication Use & Polypharmacy (IGRIMUP): position statement and 10 recommendations for Action. Drugs Aging 35:575–587. https://doi.org/10.1007/s40266-018-0554-2
Hanlon JT, Schmader KE, Samsa GP, Weinberger M, Uttech KM, Lewis IK et al (1992) A method for assessing drug therapy appropriateness. J Clin Epidemiol 45(10):1045–1051. https://doi.org/10.1016/0895-4356(92)90144-C
Onder G, Landi F, Fusco D, Corsonello A, Tosato M, Battaglia M et al (2014) Recommendations to prescribe in complex older adults: results of the CRIteria to assess appropriate medication use among elderly complex patients (CRIME) project. Drugs Aging 31(1):33–45. https://doi.org/10.1007/s40266-013-0134-4
Lee JQ, Ying K, Lun P, Tan KT, Ang W, Munro Y, Ding YY (2020) Intervention elements to reduce inappropriate prescribing for older adults with multimorbidity receiving outpatient care: a scoping review. BMJ Open 10(8):e039543. https://doi.org/10.1136/bmjopen-2020-039543
Michie S, van Stralen MM, West R (2011) The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 6(1):42. https://doi.org/10.1186/1748-5908-6-42
Michie S, Atkins L, West R (2014) The behaviour change wheel: a guide to designing interventions. Silverback Publishing, London
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W et al (2013) The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 46(1):81–95. https://doi.org/10.1007/s12160-013-9486-6
Hsu CC, Sandford BA (2007) The Delphi technique: making sense of consensus. Pract Assess Res Evaluation 12(10):1–8. https://doi.org/10.7275/pdz9-th90
Trevelyan EG, Robinson PN (2015) Delphi methodology in health research: how to do it? Eur J Integr Med 7(4):423–428. https://doi.org/10.1016/j.eujim.2015.07.002
de Villiers MR, de Villiers PJT, Kent AP (2005) The Delphi technique in health sciences education research. Med Teach 27(7):639–643. https://doi.org/10.1080/13611260500069947
Humphrey-Murto S, de Wit M (2019) The Delphi method—more research please. J Clin Epidemiol 106(2019):136–139. https://doi.org/10.1016/j.jclinepi.2018.10.011
Lewthwaite H, Effing TW, Lenferink A, Olds T, Williams MT (2018) Improving physical activity, sedentary behaviour and sleep in COPD: perspectives of people with COPD and experts via a Delphi approach. PeerJ 6:e4604. https://doi.org/10.7717/peerj.4604
Rezakhani Moghaddam H, Allahverdipour H, Matlabi H (2018) Successful recruitment and retention strategies for women health volunteers: viewpoints of the volunteers’ supervisors and relevant researchers. J Multidiscip Healthc 11:621–634. https://doi.org/10.2147/JMDH.S180544
Campbell SM, Shield T, Rogers A, Gask L (2004) How do stakeholder groups vary in a Delphi technique about primary mental health care and what factors influence their ratings? BMJ Qual Saf 13(6):428–434. https://doi.org/10.1136/qshc.2003.007815
Hansen CR, O’Mahony D, Kearney PM, Sahm LJ, Cullinan S, Huibers CJA et al (2018) Identification of behaviour change techniques in deprescribing interventions: a systematic review and meta-analysis. Br J Clin Pharmacol 84(12):2716–2728. https://doi.org/10.1111/bcp.13742
Isenor JE, Bai I, Cormier R, Helwig M, Reeve E, Whelan AM et al (2020) Deprescribing interventions in primary health care mapped to the behaviour change wheel: a scoping review. Res Social Adm Pharm 17(7):1229–1241. https://doi.org/10.1016/j.sapharm.2020.09.005
Reynolds A (2009) Patient-centered Care. Radiol Technol 81:133–147
Clay-Williams R, Braithwaite J (2009) Determination of health-care teamwork training competencies: a Delphi study. Int J Qual Health Care 21(6):433–440. https://doi.org/10.1093/intqhc/mzp042
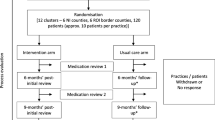
Cardwell K, Clyne B, Moriarty F, Wallace E, Fahey T, Boland F et al (2018) Supporting prescribing in Irish primary care: protocol for a non-randomised pilot study of a general practice pharmacist (GPP) intervention to optimise prescribing in primary care. Pilot Feasibility Stud 4(1):122. https://doi.org/10.1186/s40814-018-0311-7
Acknowledgements
We would like to thank our Delphi panel experts for their time and dedication in this study and Ms Kate Ying for planning, formulating, and reviewing the Delphi statements for the first round of the survey. None received compensation for their contributions. This study is funded by the Geriatric Education and Research Institute, Singapore.
Funding
This study is funded by the Geriatric Education and Research Institute, Singapore through the Intramural Grant Award (GERI1622) for the project “Appropriate prescribing for older adults with multimorbidity: from barriers to solutions”.
Author information
Authors and Affiliations
Contributions
Study design PL, WA, KTT and YYD. Data collection and analysis JYT, PL, PHJT and YYD. Manuscript preparation JYT, PL, PHJT, WA, KTT and YYD. All authors listed provided feedback on draft versions of the paper and approved the final manuscript in its current version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no relevant conflict of interest.
Ethical approval
The study was granted ethical approval by the National Health Group Domain Specific Review Board, Singapore (NHG DSRB Ref: 2019/00521).
Consent to participate and for publication
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
41999_2021_566_MOESM1_ESM.pdf
Supplementary file1 Supplementary material 1: Round one survey questions for Delphi study: Intervention Elements to Reduce Inappropriate Prescribing for Older Adults (PDF 203 KB)
41999_2021_566_MOESM2_ESM.pdf
Supplementary file2 Supplementary material 2: Round two survey questions for Delphi study: Intervention Elements to Reduce Inappropriate Prescribing for Older Adults (PDF 147 KB)
41999_2021_566_MOESM3_ESM.pdf
Supplementary file3 Supplementary table 1: BCTs statements with high group agreement for low importance. The mapped intervention functions and their associated BCTs with the statements adapted for the survey are shown (PDF 80 KB)
41999_2021_566_MOESM4_ESM.pdf
Supplementary file4 Supplementary table 2: BCTs statements with low group agreement. The mapped intervention functions and their associated BCTs with the statements adapted for the survey are shown (PDF 16 KB)
Rights and permissions
About this article
Cite this article
Tang, J.Y., Lun, P., Teng, P.H.J. et al. Intervention elements and behavior change techniques to improve prescribing for older adults with multimorbidity in Singapore: a modified Delphi study. Eur Geriatr Med 13, 531–539 (2022). https://doi.org/10.1007/s41999-021-00566-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00566-5