Abstract
Objective
Protection against vaccine-preventable diseases is especially relevant in older adults due to age-related decline in immunity (immunosenescence). However, adult vaccination remains a challenge with overall low coverage rates, which has an impact on both the patients who have these diseases and the health care system in terms of resource use and costs derived. This study aimed to estimate the direct economic impact of herpes zoster, pneumococcal disease, influenza and pertussis in Spanish adults 45 years and older.
Methods
Data from 2015 were extracted from two Spanish public databases: the Minimum Basic Data Set for Hospitalisations and the Clinical Database of Primary Care. Codes from the International Classification of Diseases and the International Classification of Primary Care were used to identify and classify the diseases analysed. The variables extracted and calculated were hospitalisation (cases, percentage, length of stay, costs, mortality), primary care (cases, percentage, costs) and referrals (cases, percentage, costs). Results were presented for the age groups 45–64 years, 65–74 years, > 74 years and all ages.
Results
In adults 45 years and older, total costs amounted to €134.1 million in 2015 (i.e. 63.9% of the total direct costs for all age groups): 44.4% due to pneumococcal disease, 39.5% due to influenza, 16.0% due to herpes zoster and 0.1% due to pertussis. Hospitalisations represented 58.1% (€77.9 million) of the total costs, with 15,910 admissions, 144,752 days of hospitalisation and 1170 deaths. Primary care registered 566,556 visits with a cost of €35.0 million, and 269,186 referrals with a cost of €21.1 million.
Conclusion
The direct economic burden of herpes zoster, pneumococcal disease, influenza and pertussis in adults 45 years and older was high in Spain, and may be underestimated as it only considered medical assistance and not other applicable direct or indirect costs. Increasing vaccination rates in adults may potentially reduce the economic burden derived from these diseases, although future cost-effectiveness analysis including other disease-related costs, vaccination costs and vaccination effectiveness would be needed.
Graphical Abstract

Similar content being viewed by others
Adult vaccination is a public health challenge in countries like Spain, where the population is rapidly ageing. |
In Spain, a direct cost of €134.1 million is attributable to four vaccine-preventable diseases in adults aged ≥ 45 years (or 63.9% of direct healthcare expenditure for all ages); pneumococcal disease accounted for 44.4% of the burden, followed by influenza (39.5%), herpes zoster (16.0%) and pertussis (0.1%). |
Hospitalisations had the highest burden with 58.1% of the total costs (€77.9 million), with 15,910 admissions, 144,752 days of hospitalisation and 1170 deaths. It was followed by primary care (€35.0 million, 26.1%) and referrals (€21.1 million, 15.8%). |
1 Introduction
Vaccination is an efficient public health strategy to prevent infectious diseases. Its use has significantly reduced the burden of vaccine-preventable diseases over the past 40 years and prevents 4–5 million deaths every year around the world [1, 2]. However, while childhood immunisation is well established worldwide, vaccination of the older population remains a public health challenge [3].
Susceptibility to infectious diseases increases with age due to a decline in the immune system, called immunosenescence [4, 5]. This age-related phenomenon leads to an increased risk and severity of infectious diseases, which in turns lead to a loss of independence, disability and death [5]. Influenza and pneumonia, for example, are often associated with severe complications and are ranked as the sixth leading cause of death among adults over 65 years in developed countries [6, 7]. Moreover, ageing is also related to lower vaccine efficacy and persistence of immunity. However, it should be noted that significant improvements have been made in vaccines for older adults, either by the addition of novel adjuvants or by increasing antigen concentration, thus minimising the effect of ageing on vaccine efficacy [8].
In Spain, as in many parts of the world, the population is rapidly ageing, with the proportion of people over 65 years of age increasing every year (19.3% of the population in 2019). Furthermore, the mean age has increased by more than 10 years in the past 50 years (from 32.7 years in 1970 to 43.3 years in 2019) [9]. Life expectancy is one of the highest in the European Union (EU), reaching 86.7 years for women and 81.1 years for men in 2019, while the EU average was 84.0 years for women and 78.5 years for men [10]. When considering healthy life expectancy (i.e. an indicator of population health that considers whether the gains in life expectancy are lived in good health or with some health issues and disabilities), men above 65 years live 59.0% of their remaining time in good health without disabilities, while this value in women is 48.1% (54.1% for men and 46.3% for women in the EU) [9, 11].
The ageing population has a direct economic impact since older adults were responsible for 45.9% of hospital admissions in 2018 in Spain, with longer hospital stays and a higher risk of comorbidities than the younger population [9]. In previously published economic analyses, four adult vaccine-preventable diseases (i.e. influenza, pertussis, herpes zoster and pneumococcal disease) were associated with substantial human and economic burden [12, 13]. However, currently only two vaccines (i.e. pneumococcal and influenza) are included in the Spanish National Immunisation Programme (NIP) for adults ≥ 65 years of age [14]. Although Spain is one of the most advanced countries in childhood immunisation, with coverage rates above 97%, rates in adults remain low and, in some cases, decrease over time. For instance, influenza vaccination coverage among adults older than 65 years was 70.1% in the 2005–2006 season and 65.7% in 2009–2010, dropping to 54.7% in the 2019–2020 season (EU average 38.6% in 2018) [11, 15,16,17].
This study aims to estimate the direct economic burden attributable to four vaccine-preventable infectious diseases in older adults in Spain: herpes zoster, pneumococcal disease, influenza and pertussis.
2 Methods
This is a health economics study based on data extraction and calculations from two Spanish public databases, in order to obtain the direct economic costs of medical services attributable to four adult preventable diseases, from the Spanish National Healthcare System (NHS) perspective. The databases used were the Minimum Basic Data Set for Hospitalisations (CMBD-H, Conjunto Mínimo Básico de Datos—Hospitalización) [18] and the Clinical Database of Primary Care (BDCAP, Base de Datos Clínicos de Atención Primaria) [19], which both contain information directly registered by healthcare professionals of the NHS. The analysis was carried out with data from 2015 as it was the latest available at the time of the study, in order to estimate the annual direct costs of four vaccine-preventable diseases (i.e. herpes zoster, pneumococcal disease, influenza and pertussis) in Spain for older adults aged 45 years and over.
2.1 Description of Databases
The CMBD-H integrates administrative and clinical information on patients admitted to hospitals. This database includes annual data from 505 public (since 1997; 313 hospitals) and private (since 2005; 192 hospitals) hospitals that cover approximately 93% of the total hospitalisations from all regions in Spain [18]. The CMBD-H uses the International Classification of Diseases ninth edition (ICD-9) to classify and report diseases [20, 21]. The list of ICD-9 codes used can be found in Table 1. For this study, primary diagnosis for diseases (identified through the ICD-9 codes) is used in the extraction of hospitalisation data.
The BDCAP annually gathers standardised clinical data in the domain of primary care (PC) consultations. Data are collected randomly from a sample (around 10%) of the population’s medical records and are representative of each region (except Ceuta and Melilla from a total of 17 regions). However, the number of cases presented in this database is adjusted to the reference population, and not just to the sample included [19, 22]. The BDCAP is coded following the International Classification of Primary Care (ICPC-2) as shown in Table 1 [23].
These two databases were selected on the basis that they are publicly available and collect data from both healthcare levels (PC consultations and hospitalisations) to estimate the direct economic burden.
2.2 Population and Variables Included in the Study
In both databases, data were extracted and analysed for the year 2015 and for the age groups 45–64 years, 65–74 years, > 74 years and all ages. The focus of the study is to show data on adults ≥ 45 years of age, so total stay and information regarding the number of deaths in the ‘all ages’ group are not reported.
The CMBD-H database provided the following variables included in the analysis: number of hospitalisation cases, average stay per hospitalisation, median cost of hospitalisation and number of deaths. From these data, the following have been calculated: percentage of cases, total length of hospital stays, total costs and percentage of deaths among patients per age group.
The variables included and available in the BDCAP database were number of PC cases and number of cases referred to specialists. Consultation costs both for PC and referrals were not directly available in the BDCAP as for the CMBD-H, so were estimated at €61.87/visit for first PC visit and €78.48/visit for referrals, as these were the average costs from data on the official tariffs from autonomous regions, available in a Spanish cost database for the year 2015 [24]. These costs were just for the visits themselves and did not include pharmacological costs derived from patient management. Based on these data, the following variables were calculated: percentage of total cases, cost of PC consultation, percentage of referrals to specialists and referrals costs. The number of cases presented at the BDCAP were already extrapolated to the total Spanish population from the sample used to estimate it. Data were analysed in age groups of 5 years. In regions with < 30 cases, data were not available (e.g. cases of herpes zoster in Extremadura). Furthermore, some regions do not report referral data.
3 Results
3.1 Hospitalisation
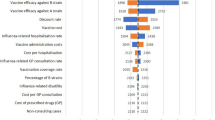
As shown in Fig. 1 and Table 2, the majority of the hospitalisations caused by the four preventable diseases were concentrated in the ≥ 45-years group (77.9%). Pneumococcal disease was responsible for the highest number of hospitalisations within the general population. Likewise, among adults 45 years and older, pneumococcal disease also ranked first when analysed for number of hospitalisations, average stay in hospital, mortality rate and median cost per admission.
Influenza was the second most common cause of hospital admission, with 75.9% occurring in the ≥ 45-years group.
For herpes zoster, 81.1% of the total admissions occurred in adults 45 years and older, while most pertussis hospitalisations were registered in the younger age group, with only 1.5% of the total admission in adults 45 years and older.
3.2 Primary Care and Referrals
Data from the BDCAP database showed that influenza accounts for the highest number of PC visits among all ages, followed by herpes zoster, pneumococcal disease and pertussis. However, in the ≥ 45-years group, herpes zoster accounted for most PC visits, followed by pneumococcal disease, influenza and pertussis (Table 3).
Regarding the referrals to specialists from PC visits, 48.8% of the referrals for all ages were for those in the ≥ 45-years group. This proportion was higher for pneumococcal disease and herpes zoster (Table 3).
3.3 Total Costs
As shown in Table 4, 63.9% (€134.1 million) of the total costs were incurred by adults aged 45 years and older. This percentage is even higher when looking at specific diseases, such as herpes zoster or pneumococcal disease. In this age group (≥ 45 years), pneumococcal disease had the highest burden (44.4% of the total direct cost), followed by influenza (39.5%), herpes zoster (16.0%) and pertussis (0.1%).
Regarding the distribution of the total cost by type of resource (shown in Fig. 2), hospitalisations have the highest impact on the total costs of all diseases, accounting for 58.1% of the total cost. However, within each disease, hospitalisations accounted for the highest impact on total cost for pneumococcal disease and influenza, but not for herpes zoster and pertussis, whose burdens are mainly derived from PC visits.
4 Discussion
This study analysed data from two public databases in 2015 and showed a direct economic burden of €134.1 million for the Spanish NHS attributable to the four preventable diseases in adults ≥ 45 years of age. Pneumococcal disease accounted for 44.4% of the burden, followed by influenza (39.5%), herpes zoster (16.0%) and pertussis (0.1%). Hospitalisations had the highest burden with 58.1% of the total costs (€77.9 million), then PC (€35.0 million, 26.1%) and referrals (€21.1 million, 15.8%). Moreover, the four preventable diseases in adults ≥ 45 years of age accounted for 63.9% of total direct healthcare expenditure of these diseases in the Spanish general population.
The present study has only estimated the direct medical costs extracted from public databases; the costs calculated may be underestimated since other relevant direct or indirect costs, such as those derived from productivity losses, were not considered. Previously published studies on these four diseases have included other resources and parameters to estimate the burden. For instance, in Spain, workers take on average 5 days of sick leave for an influenza episode [25], which has an indirect impact on the economy. An observational study from 2006, which took into account both direct and indirect costs of an influenza epidemic in Spain, determined this burden at €1036.9 million, with €371.2 million on account of absenteeism [26]. This estimate is approximately ten times higher than the estimate for influenza in the present study (€102.9 million as seen in Table 4), probably due to the different methodology used to capture resource use.
In addition, several publications have shown results consistent with those of the present study, thus confirming the reliability of the analysis performed. A recent study estimated the economic burden of herpes zoster in Spanish adults aged 50 years or older from an NHS and societal perspective. The results of this analysis were aligned with the present study: costs were higher in older age groups and, in the distribution of direct costs, the burden was derived mainly from PC visits (44.9%; compared with 49.6% in the present study) [27].
Another study on the risk of hospitalisation due to pneumococcal disease in Spain pointed out that, in 2011, there were 10,861 hospital discharges, with significantly higher hospitalisation rates among patients over the age of 65 years [28]. The estimated cost of these hospitalisations was more than €57 million, which is consistent with the current estimation (€58.7 million). As expected, the disease burden was higher among the older population.
Regarding pertussis, prior studies have also revealed a marked age distribution in cases, with the highest incidence among the youngest [29, 30]. Although the incidence is not reported in our study, 89.7% of PC visits and 100% of referrals to specialists were recorded in the population < 45 years of age, which serves as an indicator of a greater number of cases in this group. In adults older than 45 years, Fernández-Cano et al. in Spain and Crespo et al. in the Catalonia region of Spain found similar incidence rates, with fewer than 0.1 cases per 100,000 and 0.11 cases per 100,000 people, respectively [29,30,31]. However, this number is far below the observed values in other countries (e.g. 1–2 cases per 100,000 people in the Netherlands, 2–5 cases per 100,000 people in Denmark and 2.9–4.6 cases per 100,000 people in North America), and the authors assumed severe underreporting [31]. Since pertussis symptoms are usually mild in the adult population, and PC physicians are less sensitised than paediatricians, it can be easily undiagnosed [29, 32].
Data used in the current study were from 2015, as these were the latest available at the time of the study. Despite the possible dynamics of healthcare costs, these data are still useful from a public health perspective since healthcare resources attributable to these four diseases can be assumed to have remained constant over the years until 2020 when the COVID-19 pandemic started. Three statements support this choice: first, the RENAVE reports showed no variation in the incidence of the four diseases over the last years in Spain, which suggest no variation in direct medical resources (i.e. herpes zoster incidence in Spain was constant from 2014 to 2018 [33], as well as flu incidence from 2015 to 2018 [34, 35]); second, vaccination coverage rates for adults aged 65 years or older remained low and constant over time [36, 37]; and finally, as shown by the Spanish National Institute of Statistics, the Consumer Price Index remained stable until 2020 [38].
Although childhood immunisation programmes are well known and implemented in Spain and are characterised by high vaccination coverage, adult vaccination is often neglected [37]. In 2019, a multidisciplinary panel of healthcare experts published an opinion paper about adult vaccination where they reviewed the main vaccine-preventable adult diseases (three of them included in the present study) and suggested following a vaccine selection based on that of the North American Advisory Committee on Immunisation Practices, which includes the four vaccine-preventable diseases analysed in this study among the seven diseases that would benefit most from a vaccination schedule in developed countries [25, 39].
The aim of this study was to show the distribution of the total direct costs attributable to these four diseases across all ages, and to compare them with the age group ≥ 45 years. Our findings highlighted that 63.9% of the total costs were attributable to this age group (adults ≥ 45 years). Given the low adult vaccination rates against pneumococcal disease and flu (the only ones included in the Spanish NIP) and considering that vaccination is an efficient public health intervention, our results suggest that increasing adult vaccination awareness may contribute to reduce direct medical costs, although future cost-effectiveness analysis including other disease-related costs, vaccination costs and vaccination effectiveness would be needed.
This study has several limitations. First, the databases used in the analysis capture only 93% of hospitalisations and 10% of the information on PC visits; however, as explained in the methods section, the data that BDCAP retrieves for PC visits are adjusted to the entire population. Additionally, although there is representation of the whole geographical area, not all the Spanish regions are included in the BDCAP. Data analysed were retrieved from medical records, and thus carried bias related to their collection and there was little margin to minimise this risk. However, a detailed analysis of the ICD-9 and ICPC-2 codes was performed to ensure a precise inclusion/exclusion of patients/cases. Related to the codification, ICD-9 is still in use in Spain, which does not allow the same level of specificity as the ICD-10 code would allow. Likewise, the ICPC-2 codification is not very specific, which could cause some bias due to an inadequate specificity of disease definition. In addition, since 2015, some updates have been made to the codification of the databases, which do not meet the needs of the project. Consultation costs for both PC and referrals were just for the visits themselves and did not include the pharmacological costs derived from patients’ management. Finally, the information available is related to episodes of the diseases (e.g. hospitalisation, PC visits) but not to patients; therefore, data can only be used as an approximation of the diseases’ incidence, and exact incidence cannot be calculated.
5 Conclusion
This study showed that the direct economic burden of herpes zoster, pneumococcal disease, influenza and pertussis was high in Spain for adults ≥ 45 years of age, accounting for 63.9% of the direct economic burden of these diseases across all ages, and even with estimated costs being potentially underestimated due to the absence of other direct and indirect costs. Hospitalisations accounted for more than half of this burden, followed by PC visits and referrals. Increasing preventative healthcare such as vaccination coverage among older adults may potentially reduce the economic burden of these four vaccine-preventable infectious diseases, especially herpes zoster, pneumococcal disease and influenza, for the NHS and allow for redistribution of available healthcare resources. However, future cost-effectiveness analysis including other disease-related costs, vaccination costs and vaccination effectiveness would be needed to confirm this assumption.
References
Turner HC, Thwaites GE, Clapham HE. Vaccine-preventable diseases in lower-middle-income countries. Lancet Infect Dis. 2018;18(9):937–9. https://doi.org/10.1016/S1473-3099(18)30478-X.
World Health Organization (WHO). Immunization. 2019. https://www.who.int/news-room/facts-in-pictures/detail/immunization. Accessed 09 Aug 2021.
Gaillat J. Where are the keys to improve vaccine uptake in adults and elders in European countries? Aging Clin Exp Res. 2021;33(4):1123–31. https://doi.org/10.1007/s40520-019-01443-9.
Fülöp T, Dupuis G, Witkowski JM, Larbi A. The role of immunosenescence in the development of age-related diseases. Rev Invest Clin. 2016;68(2):84–91.
Weinberger B, Herndler-Brandstetter D, Schwanninger A, Weiskopf D, Grubeck-Loebenstein B. Biology of immune responses to vaccines in elderly persons. Clin Infect Dis. 2008;46(7):1078–84. https://doi.org/10.1086/529197.
Eurostat. Causes of death statistics—people over 65. 2020. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Causes_of_death_statistics_-_people_over_65. Accessed 09 Aug 2021.
Heron M. Deaths: leading causes for 2019. National Center for Health Statistics (U.S.). Division of Vital Statistics. 2021;70(9). https://doi.org/10.15620/cdc:107021. Accessed 09 Aug 2021.
Cunningham AL, McIntyre P, Subbarao K, Booy R, Levin MJ. Vaccines for older adults. BMJ. 2021;372: n188. https://doi.org/10.1136/bmj.n188.
Díaz JP, García AA, Nieto PA, Fariñas DR. Informes Envejecimiento en red nº 25, 39p. Un perfil de las personas mayores en España, 2020. Indicadores estadísticos básicos 2020. http://envejecimiento.csic.es/documentos/documentos/enred-indicadoresbasicos2020.pdf. Accessed 01 June 2021.
Instituto Nacional de Estadística. 4.1. Esperanza de vida. 2020. https://www.ine.es/ss/Satellite?c=INESeccion_C&cid=1259926380048&p=1254735110672&pagename=ProductosYServicios%2FPYSLayout Accessed 09 Aug 2021.
OECD/European Union. Health at a Glance: Europe 2020: State of Health in the EU Cycle. 2020. https://ec.europa.eu/health/sites/default/files/state/docs/2020_healthatglance_rep_en.pdf. Accessed 01 June 2021.
Carrico J, Talbird SE, La EM, Poston S, Poirrier J-E, DeMartino JK, et al. Cost-benefit analysis of vaccination against four preventable diseases in older adults: impact of an aging population. Vaccine. 2021;39(36):5187–97. https://doi.org/10.1016/j.vaccine.2021.07.029.
McLaughlin JM, McGinnis JJ, Tan L, Mercatante A, Fortuna J. Estimated human and economic burden of four major adult vaccine-preventable diseases in the United States, 2013. J Prim Prev. 2015;36(4):259–73. https://doi.org/10.1007/s10935-015-0394-3.
Consejo Interterritorial. Sistema Nacional de Salud. Calendario común de vacunación a lo largo de toda la vida. Calendario recomendado año 2021. 2021. https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/calendario-y-coberturas/docs/CalendarioVacunacion_Todalavida.pdf. Accessed 24 Nov 2021.
Ministerio de Sanidad, Consumo y Bienestar Social. Tabla coberturas de vacunación frente a gripe en ≥ 65 años, personas de 60–64 años, embarazadas y personal sanitario. Comunidades Autónomas. Campaña 2018–2019. https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/calendario-y-coberturas/coberturas/docs/Tabla13.pdf. Accessed 31 May 2021.
Sociedad Española de Geriatría y Gerontologia. Recomendaciones de vacunación para adultos y mayores y calendarios vacunales 2019–2020. https://www.segg.es/media/descargas/VACUNAS-SEGG-2019-2020.pdf. Accessed 31 May 2021.
Ministerio de Sanidad, Consumo y Bienestar Social. Tabla evolución coberturas de primovacunación. España, 2009–2019. https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/calendario-y-coberturas/coberturas/docs/Tabla1.pdf. Accessed 31 May 2021.
Ministerio de Sanidad. Portal estadistico. Area de Inteligencia de Gestion. Conjunto Mínimo Básico de Datos—Hospitalización (CMBD-H). Desde 1997 hasta 2015 incluido. https://pestadistico.inteligenciadegestion.mscbs.es/publicoSNS/N/rae-cmbd/cmbd-h. Accessed 01 June 2021.
Ministerio de Sanidad. Portal estadistico. Area de Inteligencia de Gestion. Base de Datos de Clínicos de Atención Primaria (BDCAP). https://pestadistico.inteligenciadegestion.mscbs.es/publicoSNS/S/base-de-datos-de-clinicos-de-atencion-primaria-bdcap. Accessed 03 June 2021.
Centers for Disease Control and Prevention. National Center for Health Statistics. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). 2015. https://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed 01 June 2021.
Ministerio de Sanidad, Política Social e Igualdad. Informacion y Estadisticas sanitarias 2011. Clasificación Internacional de Enfermedades. 9ª Revisión Modificación Clínica (CIE-9-MC). 8ª Edición. 2012. https://www.mscbs.gob.es/estadEstudios/estadisticas/docs/CIE9MC_8ed.pdf. Accessed 01 June 2021.
Ministerio de Sanidad. BDCAP. Base de Datos Clínicos de Atención Primaria. Ficha técnica—Datos 2018. 2018. https://www.mscbs.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SIAP/Ficha_tecnica_BDCAP_2018.pdf. Accessed 09 Aug 2021.
World Health Organization. International Classification of Primary Care, 2nd edition (ICPC-2). 2021. https://www.who.int/standards/classifications/other-classifications/international-classification-of-primary-care. Accessed 03 June 2021.
Oblikue Consulting S.L. Spanish Health Costs and cost-effectiveness ratios Database: eSalud. http://oblikue.com/bddcostes/. Accessed 03 June 2021.
Bouza E, Ancochea-Bermúdez J, Campins M, Eirós-Bouza JM, Fargas J, Rojas AG, et al. The situation of vaccines for the prevention of infections in adults: an opinion paper on the situation in Spain. Rev Esp Quimioter. 2019;32(4):333–64.
Llach XB, Gamisans MR, Tudel JMF, Sanz CA, Rubio TC. Study of flu costs. Aten Primaria. 2006;38(5):260–7. https://doi.org/10.1157/13092984.
Díez-Domingo J, Curran D, Cambronero MdR, Garcia-Martinez J-A, Matthews S. Economic burden and impact on quality of life of Herpes Zoster in Spanish adults aged 50 years or older: a prospective cohort study. Adv Ther. 2021. https://doi.org/10.1007/s12325-021-01717-7.
Gil-Prieto R, Pascual-Garcia R, Walter S, Álvaro-Meca A, Gil-De-Miguel Á. Risk of hospitalization due to pneumococcal disease in adults in Spain. The CORIENNE study. Hum Vaccin Immunother. 2016;12(7):1900–5. https://doi.org/10.1080/21645515.2016.1143577.
Fernández-Cano MI, Armadans Gil L, Martínez Gómez X, Campins MM. Incidence of whooping cough in Spain (1997–2010): an underreported disease. Eur J Pediatr. 2014;173(6):721–6. https://doi.org/10.1007/s00431-013-2228-8.
Crespo I, Broner S, Soldevila N, Martínez A, Godoy P, Sala-Farré M-R, et al. Characteristics of pertussis outbreaks in Catalonia, Spain, 1997 to 2010. Hum Vaccin Immunother. 2015;11(1):231–5. https://doi.org/10.4161/hv.36156.
Kandeil W, Atanasov P, Avramioti D, Fu J, Demarteau N, Li X. The burden of pertussis in older adults: what is the role of vaccination? A systematic literature review. Expert Rev Vaccines. 2019;18(5):439–55. https://doi.org/10.1080/14760584.2019.1588727.
Campinsa M, Moreno-Pérez D, Gil-de Miguel A, González-Romo F, Moraga-Llop FA, Arístegui-Fernández J, et al. Tos ferina en España. Situación epidemiológica y estrategias de prevención y control. Recomendaciones del Grupo de Trabajo de Tos ferina [Whooping cough in Spain. Current epidemiology, prevention and control strategies. Recommendations by the Pertussis Working Group]. Enferm Infect Microbiol Clin. 2013;31(4):240–53. https://doi.org/10.1016/j.eimc.2012.12.011.
Masa-Calles J, López-Perea N, Cordero BV, Carmona R. Vigilancia y epidemiología del herpes zóster en España. Rev Esp Salud Pública. 2021;95:e1-13.
Centro Nacional de Epidemiología. CIBER Epidemiología y Salud Pública (CIBERESP). Instituto de Salud Carlos II. Resultados de la Vigilancia Epidemiológica de las enfermedades transmisibles. Informe anual. Año 2015. 2017. https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/INFORMES%20RENAVE/RENAVE_INFORME_ANUAL_2015.pdf. Accessed 23 Nov 2021.
Red Nacional de Vigilancia Epidemiológica. Instituto de Salud Carlos III. Ministerio de Ciencia e Innovación. Resultados de la Vigilancia Epidemiológica de las enfermedades transmisibles. Informe anual. Años 2017–2018. 2020. https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/INFORMES%20RENAVE/ultimo%20informe.pdf. Accessed 23 Nov 2021.
Ministerio de Sanidad, Consumo y Bienestar Social. Vacunas y Programa de Vacunación. 2021. https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/calendario-y-coberturas/coberturas/home.htm. Accessed 23 Nov 2021.
Ministerio de Sanidad, Consumo y Bienestar Social. Coberturas de Vacunación. Datos Estadísticos. 2021. https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/calendario-y-coberturas/coberturas/home.htm. Accessed 09 June 2021.
Instituto Nacional de Estadística. Índices nacionales: general y de grupos ECOICOP. 2021. https://www.ine.es/jaxiT3/Tabla.htm?t=22344. Accessed 23 Nov 2021.
Kim DK, Riley LE, Harriman KH, Hunter P, Bridges CB. Recommended immunization schedule for adults aged 19 years or older, United States, 2017. Ann Intern Med. 2017;166(3):209–19. https://doi.org/10.7326/M16-2936.
Acknowledgements
The authors would like to thank Joffrey Baneton for operational assistance and project management during the conduct of the study. They also thank Business & Decision Life Sciences platform for editorial assistance and manuscript coordination, on behalf of GSK. Lyes Derouiche coordinated manuscript development and editorial support. Leire Iralde Lorente provided writing support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
GlaxoSmithKline Biologicals SA funded this study/research [GSK study identifier HO-19-19871] and was involved in all stages of study conduct, including analysis of the data. GlaxoSmithKline Biologicals SA also took in charge of all costs associated with the development and publication of this manuscript.
Conflicts of interest
Ángel Gil de Miguel, José María Eiros Bouza and Luis Ignacio Martínez Alcorta declare they have received consulting fees from the GSK group of companies, during the conduct of the study. Luis Ignacio Martínez Alcorta declares receiving lecturing fees from Merck Sharp & Dohme Corp, outside the submitted work. Daniel Callejo and Carlos Miñarro are employed by IQVIA, which received funding from the GSK group of companies for the conduct of this study. Laura Amanda Vallejo-Aparicio, Andrea García, Mónica Tafalla, M del Rosario Cambronero, Rubén Rodríguez and Laura Martin-Gomez are employed by the GSK group of companies. Laura Amanda Vallejo-Aparicio, Mónica Tafalla, M. del Rosario Cambronero, Rubén Rodríguez and Laura Martin-Gomez hold shares in the GSK group of companies. Mónica Tafalla was a GSK employee when the study was conducted. All authors declare no other financial or non-financial relationships and activities.
Availability of data and material
GSK makes available anonymised individual participant data and associated documents from interventional clinical studies which evaluate medicines, upon approval of proposals submitted to www.clinicalstudydatarequest.com. To access data for other types of GSK-sponsored research, for study documents without patient-level data and for clinical studies not listed, please submit an enquiry via the website.
Code availability
Not applicable.
Authors’ contributions
AGdM, JMEB, DC, CM, AG, MT, RR and LM-G participated in the conception or the design of the study. AGdM, DC, LAV-A and CM participated in the collection or generation of the data. All authors were involved in the analyses or interpretation of the data and the development of this manuscript. All authors had full access to the data and gave final approval before submission.
Ethics approval
This is a health economics study using aggregated data sourced from public databases, not using patient-level data, so no ethical consideration was applicable.
Consent to participate
Not applicable as no individual-related data were used in this study.
Consent for publication
Not applicable as no individual-related data were used in this study.
Congress presentation
Sociedad Española de Epidemiologia—XXXIX Reunión Científica 2021.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gil de Miguel, Á., Eiros Bouza, J.M., Martínez Alcorta, L.I. et al. Direct Medical Costs of Four Vaccine-Preventable Infectious Diseases in Older Adults in Spain. PharmacoEconomics Open 6, 509–518 (2022). https://doi.org/10.1007/s41669-022-00329-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-022-00329-3