Abstract
Background
Acromegaly is a rare, chronic and debilitating disease whose treatment places a high burden on health systems. In the reality of the Brazilian public health network, many patients are kept on drug treatment because of barriers to access to surgery.
Objective
The aim of this study was to estimate the costs and budget impact of routine transsphenoidal endoscopic surgery in relation to those of long-term drug treatment with octreotide long-acting release (LAR) from a cohort of patients followed at the referral medical centre for acromegaly treatment in the Federal District, Brazil.
Methods
Based on micro-costing data collected using mixed methods from a local perspective of the public health system, we performed a budget impact analysis (BIA) on a 3-year time horizon. Uncertainty was handled with deterministic (tornado and scenario) and probabilistic (Monte Carlo simulations) sensitivity analyses.
Results
Compared with the continued use of octreotide LAR at a dose of 30 mg every 28 days, the incremental budget impact of conducting two surgeries per month, considering a cure rate of 55%, could bring savings of approximately US$879,362.18 (95% CI 860,176.29–898,548.08) over 3 years. Depending on the key variable values, the savings amplitude ranged from US$431,836.39 to US$1,519,132.04.
Conclusions
Improving access to surgery could result in significant cost reductions in acromegaly treatment. The present study stands out for being the first to estimate the costs of transsphenoidal surgery in the context of the public health system in Brazil.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Acromegaly is a rare condition associated with multiple comorbidities and increased mortality. |
Medical treatment is usually life-long and entails a high cost. |
Improving access to surgery can promote cure and significant cost reductions. |
1 Introduction
Acromegaly is a rare disease with high morbidity and mortality that is complex and expensive to manage [1]. Commonly caused by a pituitary adenoma that overproduces growth hormone (GH) and results in increased levels of insulin-like growth factor 1 (IGF-1), acromegaly is associated with chronic complications and impaired quality of life [2, 3]. Despite being a rare disease, its related comorbidities and requirement for life-long management suggest that this disease can place a considerable burden on health systems [1].
The therapeutic approach to acromegaly is multimodal; it can entail surgery, medications and radiotherapy, used alone or in combination. Transsphenoidal surgery is the first line of treatment for most cases because of the considerable chance of complete removal of the tumour when the procedure is performed by an experienced neurosurgeon [2,3,4]. However, in low- and middle-income countries, surgery may not be feasible due to difficulties related to the structure of the public health system. Medications are indicated for patients with persistent disease following surgery or as a primary treatment; the medications include somatostatin analogues, cabergoline and pegvisomant [4].
In Brazil, for rare diseases, including acromegaly, diagnosis and treatment criteria in the public health system are defined by published Clinical Protocols and Therapeutic Guidelines [5], which provide pharmacological treatment strategies for only the first two medications (somatostatin analogues and cabergoline). Conventional radiotherapy is also available through the public health system, but it is considered an adjuvant treatment and reserved only for selected cases [4].
Studying the costs of healthcare services is essential for efficient resource allocation and healthcare [6,7,8]. In many cases, this information is obtained via cost-effectiveness analysis, an economic evaluation that comprises an analysis of costs (costing study) and the effects (benefits) of a healthcare intervention [6]. In this field, budget impact analyses (BIA) are an important tool complementary to economic evaluation that are able to estimate the financial consequences of adopting and disseminating a new strategy or technology in a given health system [9]. If properly performed, budget impact studies can predict how the change in the supply of inputs or services will influence the future costing of a health problem [10].
Considering that the costs of treating acromegaly can be high [11, 12], economic studies with the objective of promoting the best possible use of public resources are essential to ensure continuity in the lines of care, especially in times of budget constraints [13]. Although there exists a range of cost studies in Brazil, including real-world data studies with large samples [14, 15], the results of a systematic review on BIA [16] have found that 95% of the papers were published in Europe and the US. In addition, the authors conclude that there was a low adherence to key characteristics of BIA and strong conflict of interest in the published studies. Thus, these economic studies are still scarce in Brazil, potentially affecting policy planning in the public health system [17]. To our knowledge, the budget impact of pituitary surgery compared with that of long-term pharmacological therapy with somatostatin analogues has not been assessed in published studies.
2 Objectives
The aim of this study was to estimate the budget impact of transsphenoidal surgery compared with that of the long-term use of octreotide long-acting release (LAR) (somatostatin analogue currently available through the local public health system) at the main centre for acromegaly treatment in the Federal District, Brazil.
3 Materials and Methods
3.1 Context, Time Horizon and Perspective
The Neuroendocrine Unit of the Brasilia University Hospital, which belongs to the public health system and is a tertiary centre of attention, comprises the main centre for pituitary diseases in the Federal District. The BIA evaluated the affordability of pituitary surgery for acromegalic patients undergoing octreotide LAR use (patients with active disease and need of medication) at the referral medical centre in both Brasilia (Brazil’s capital) and the metropolitan region.
A 3-year time horizon was used disregarding conventional economic adjustments (discount rate and inflation) in accordance with recommendations from methodological guidelines for BIA [9, 18]. The calculations were performed using Microsoft Excel® software, adopting the local public health system’s payer perspective. Costs were converted to US dollars assuming an exchange rate of 1.00 USD = 3.22 R$ in January 2018.
3.2 Population
The eligible population was estimated in a dynamic fashion, trough measuring the hospital demand and applying the incidence estimates to predict the entrance of new patients. Considering the analysis of a long-term follow-up of a cohort of 111 patients seen at the referral medical centre by 2014 (unpublished data), the total number of patients using somatostatin analogues in the year 2018 was estimated. Patient prediction at the beginning of the model and insertion of new patients were based on the annual onset rate of somatostatin analogue treatment over the last 10 years (2005–2014). We considered that all patients using somatostatin analogues could benefit from surgery, as it is considered the first-line treatment and reoperation should be evaluated when the first surgery is not effective [4].
3.3 Effectiveness of Surgery
The expected cure rate was obtained from a literature review [19,20,21,22,23,24], which supported estimates for the cure rate of the disease being between 40 and 70% among patients subjected to surgery. Among other factors related to adequate performance of the procedure, this rate can be affected by team experience and technical conditions.
3.4 Costs of Transsphenoidal Surgery
A mixed macro- and micro-costing technique [6, 25,26,27] was used to estimate the costs of endoscopic transsphenoidal surgery. Through consultation with specialists and other health professionals, the costs of the operating room, medications and materials usually used in the surgery; medical and auxiliary fees; use of special materials; expenses related to equipment maintenance; and daily rates for the intensive care unit (ICU) and general hospital ward were obtained.
A portion of these costs was provided through macro-costing by the Department of Health Costs of the Secretariat of Health of the Federal District, which participates in the National Programme for Cost Management of the Ministry of Health, whose methodology is based on absorption costing [28]. However, because this division was only recently implemented and could not measure specific values by procedure, it was necessary to estimate some cost components by micro-costing. Data regarding special material specific for neurosurgery and medications and general materials used in the operating room were obtained through this method.
To define the special materials for transsphenoidal surgery, three neurosurgeons with experience in conducting this type of procedure were consulted about the items that they considered necessary to carry out the surgery under suitable conditions. The items listed for each one were compared, and those that were noted by the majority were selected for costing (Table S1, see electronic supplementary material).
Drugs and materials used in the operating room were determined with the help of an anaesthesiologist, with the goal of including items that are usually used in this type of procedure. Subsequently, each item was looked up separately in our main price source, the computerized system (Alphalinc®) of the Secretariat of Health for the management of stock data of medications and medical-hospital materials (Table S2, see electronic supplementary material). In addition, the Department of Health Costs made available the charges for the operating room, the average costs related to the maintenance of equipment, and the medical and auxiliary fees based on a 6-h surgery. The current daily rates for the ICU and hospital were also reported.
The depreciation of equipment commonly handled by neurosurgeons and the anaesthesiologist was not calculated by a formal method. However, to minimize this limitation, the equipment maintenance calculation was adopted. This strategy was considered robust given the permanent nature of this type of apparatus.
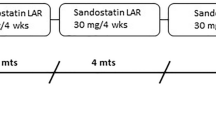
3.5 Costing of Octreotide LAR
The value for octreotide LAR acquisition was obtained through consultation in Alphalinc®. The presentation of 30 mg was considered because this is the most commonly used dose. Consistent with Brazilian guidelines, the assumption of 12 ampoules was used to estimate the annual cost [6].
3.6 Scenarios
The reference scenario was defined as the situation in which all patients were maintained under medical treatment with octreotide LAR because transsphenoidal surgery was unattainable due to local difficulties in the public health system. Alternative scenarios were delineated with different possibilities for the key parameters according to the surgery coverage: minimal (up to one surgery per month), mean (up to two surgeries per month) and maximum (up to four surgeries per month).
Thus, the base case of this analysis considered the mean coverage of 24 surgeries per year, the mean estimate of surgery effectiveness, surgery costs, and octreotide LAR costs (Table 1).
3.7 Sensitivity Analysis
With the variations of the main estimates included in the model, deterministic (tornado analysis) and probabilistic (Monte Carlo simulations) sensitivity analyses were conducted.
The tornado analysis considered the impacts of the minimum and maximum values of each variable in relation to the base case. Holding the surgery coverage parameter in the base, minimal and maximum values, the probabilistic analysis considered simulations with random selection in a uniform distribution of the range of possible values of the other key parameters (effectiveness and costs).
The variations considered the precision of the data identified in the literature (surgery effectiveness) and specialist opinion (surgery coverage). As an exception, although not being routinely recommended by methodological guidelines [9, 18], for the particular case of the surgery cost and drug prices, where there was no robust variation evidence, a conservative ± 20% amplitude was included (Table 1).
4 Results
In 2014, 54 patients used somatostatin analogues. The rate of onset of new treatments was 5.5 new cases/year considering data in the last 10 years. Applying this rate to the data, the numbers of patients in the years 2018 (n = 78), 2019 (n = 84) and 2020 (n = 90) were estimated.
4.1 Costs of Transsphenoidal Surgery
When considering a transsphenoidal surgery without major intercurrences followed by hospitalization for 3 days in the ICU and 2 days in the hospital, the average cost was estimated at US$8935.07, which included general expenses accumulated up to the patient’s discharge (Table 2).
4.2 Annual Cost per Patient for Octreotide LAR
The cost for octreotide LAR 30 mg found in Alphalinc® was US$1586.27, reflecting an annual cost of US$19,035.24. It should be emphasized that this is the somatostatin analogue currently available in the Federal District.
4.3 Budget Impact Analysis (BIA)
The results of the budget impact model were obtained after running the different planned scenarios. In the base case, providing surgery coverage at two procedures per month can bring savings of approximately –US$863,672.78 over 3 years (Table 3).
In comparison, the coverage of one surgery per month and up to four surgeries per month can alter the savings from − US$431,836.39 to − US$1,519,132.04, respectively. These data were robust in the sensitivity analysis, demonstrating a saving of resources in all the proposed scenarios. As noted in the tornado sensitivity analysis, the coverage and effectiveness of surgery are the variables that have the greatest impact on the results (Fig. 1).
In the probabilistic model with 1000 Monte Carlo simulations, the distribution of the budget impact estimates resulted in a mean savings of US$879,362.18 (95% CI 860,176.29–898,548.08) in the average coverage scenario. The budget varied from − US$427,088.49 (95% CI − 417,226.92 to − 436,950.06) to − US$1,509,229.14 (95% CI − 1,479,453.78 to − 1,539,004.51) in the minimum and maximum surgery coverage scenarios, respectively (Fig. 2).
5 Discussion
Potentially enhanced by a long and time-consuming queue for transsphenoidal surgery, a large number of patients are using somatostatin analogues in our setting. Several patients are receiving pharmacotherapy as an initial treatment because of non-availability of the procedure. This situation is not rare, as barriers such as accessibility, availability, affordability and acceptability of surgical care are common in low- and middle-income countries [29]. On the other hand, the estimated high costs of pharmacological therapy, approximately US$19,000.00 per patient per year, also demands a robust social protection system to prevent inequity issues in access to medicines [30]. These results reinforce the necessity of interventions to improve surgical care coverage.
Along with clinical and quality-of-life benefits for the patient [31], our BIA showed that improving access to surgery would be associated with economic benefits due to a significant reduction in public health system expenses. Savings of over US$400,000.00 could be reached at the end of 3 years, even in the most conservative scenario. Regarding the results generalization to the average target population, even knowing that the results of surgery are better in microadenomas, we decided to adopt a conservative cure rate of 55% (40–70%), avoiding savings overestimation (a potential result with higher cure rates). Optimizing this scenario can result in even greater savings. In the experience of a public tertiary reference centre for pituitary neurosurgery in northeast Brazil, reaching a cure rate of 75% was possible with endoscopic transsphenoidal surgery [22]. This statistic demonstrates that the achievement of good surgical results is plausible in similar contexts of the public health system if appropriate actions are implemented, which is consistent with the evidence that even in low- and middle-income countries, interventions to improve surgical care can be cost effective [30, 31].
Moreover, with better surgery coverage, a greater possibility of pharmacological control in cases with no curative perspective can also be expected, which would also result in savings. Even when it is not possible to completely remove a tumour due to anatomical reasons, the resection of all possible tumour tissue (debulking) promotes a better response to drug treatment, which could lead to the use of lower doses of somatostatin analogues and a reduction in costs of treatment [4, 32,33,34].
Our results are also consistent with the implementation of recent clinical recommendations, as the latest acromegaly guidelines from the Endocrine Society reinforce and prioritize surgery as the treatment of choice for most patients because it can produce immediate lowering of GH levels and provide tumour tissue for pathological characterization [4]. Currently, these recommendations are not implemented in our service due to issues inherent to the public health system in the Federal District, especially a lack of local investment and planning for surgery.
A strength of the present economic study is its accurate reflection of the local reality, both in the estimation of costs and in the estimation of the population. The costs are highly representative, as they were collected via validated methods in macro- and micro-costing, including absorption costing, database registries and interviews. Our clinical setting is based on data obtained via the historical analysis of a 10-year service follow-up. Considering the current population of the Federal District, approximately 3,000,000, the rate of treatment initiation assessed as six new cases per year is not overestimated relative to the disease incidence rate, usually documented in approximately three to four cases per million [35] and is consistent with barriers to diagnosis and access to medical care.
This study conducted all analyses according to the latest guidelines of the Ministry of Health of Brazil [18], which follows the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) recommendations [9]. The results were robust through both deterministic and probabilistic sensitivity analyses with Monte Carlo simulations. The tornado diagram showed that coverage of surgery and its effectiveness are the parameters that have the greatest repercussions on the magnitude of the reduction of costs.
However, the study also has limitations that should be taken into account when the results are interpreted. It is important to mention that the estimated cost of surgery was performed from the perspective of a single centre in Brasilia. Even though it is feasible to extrapolate the results to the entire Federal District, it is important to consider the main differences in healthcare management when applying the results to other settings in Brazil.
Another limitation is the fact that costs related to complications of surgery, adverse effects of drug treatment and complications of acromegaly in inadequately treated patients were not evaluated. Although transsphenoidal surgery is considered a safe procedure with a low incidence of delayed complications [36], some immediate complications can occur. Nevertheless, the incidence of these complications is considered very low, not invalidating our model. In a series of more than 1100 surgeries, endocrine complications, including transient diabetes insipidus (4.3%), symptomatic hyponatraemia (4.2%) and new hypopituitarism (any axis, 3.6%), were the most frequent. Serious events, such as mortality (0.1%), occurred in < 3% of patients [37]. In relation to drug therapy, there are potential side effects of long-term use. According to published follow-up data, approximately 25% of patients can develop gallstones, usually during the first year of treatment [38]. Cholelithiasis is a risk of somatostatin analogue therapy, but most patients with cholelithiasis are asymptomatic and rarely develop cholecystitis [38]. Thus, despite some limitations, the conclusions of our model are still robust considering that drug side effects would probably enhance the savings observed.
It is also important to reinforce that the BIA is a complementary study to an economic evaluation. For a complete body of evidence, results from an economic evaluation that considers not only the monetary benefits but also the consequences on health, such as cost-effective and cost-utility analyses, are highly recommended [6]. Yet, with all the adopted scenarios supporting decisions in favour of surgery due to resource savings, we believe that our results already provide convincing evidence for improving access to surgery for patients with acromegaly treated in the public health system. As one of the main implications for practice, supported by our results, we hope that the surgery access could be a priority issue to be discussed in future acromegaly guidelines revisions by the Ministry of Health.
6 Conclusions
The BIA showed that significant savings could be achieved by improving access to transsphenoidal surgery. This research within the Federal District has generated important public information that can be applied to the local planning of actions with the objective of improving the quality of care for acromegalic patients and reducing the costs associated with treatment.
Data Availability Statement
All the costs and values used in this model are available in the supplementary materials (Tables S1 and S2). The full model spreadsheets are also available online in a public repository (Mendeley Data), which can be freely accessed and referenced through its unique digital object identifier (https://doi.org/10.17632/y3gvkz8gmz.1).
References
Ben-Shlomo A, Sheppard MC, Stephens JM, Pulgar S, Melmed S. Clinical, quality of life, and economic value of acromegaly disease control. Pituitary. 2011;14:284–94.
Melmed S. Acromegaly. N Engl J Med. 2006;355:2558–73.
Abreu A, Tovar AP, Castellanos R, Valenzuela A, Giraldo CMG, Pinedo AC, et al. Challenges in the diagnosis and management of acromegaly: a focus on comorbidities. Pituitary. 2016;19:448–57.
Katznelson L, Laws ER Jr, Melmed S, Molitch ME, Murad MH, Utz A, et al. Acromegaly: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(11):3933–51.
Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Portaria SAS/MS no 199 - 25/02/2013. Protocolo Clínico e Diretrizes Terapêuticas da Acromegalia. 2013.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. 4th ed. Oxford: Oxford University Press; 2015.
Rudmik L, Drummond M. Health economic evaluation: Important principles and methodology. Laryngoscope. 2013;123:1341–7.
Shepard DS, Hodgkin D, Anthony YE. Analysis of hospital costs: a manual for managers. Geneva: World Health Organization; 2000.
Sullivan SD, Mauskopf JA, Augustovski F, Jaime Caro J, Lee KM, Minchin M, et al. Budget impact analysis—principles of good practice: report of the ISPOR 2012 budget impact analysis good practice ii task force. Value Heal. 2014;17:5–14.
Silva MT, da Silva EN, Pereira MG, Silva MT, da Silva EN, Pereira MG. Análise de impacto orçamentário. Epidemiol e Serviços Saúde. 2017;26:421–4.
da Silva EN, Sousa TRV. Economic evaluation in the context of rare diseases: is it possible? Cad Saude Publica. 2015;31:496–506.
Kimmell KT, Weil RJ, Marko NF. Multi-modal management of acromegaly: a value perspective. Pituitary. 2015;18:658–65.
Arbel R, Greenberg D. Rethinking cost-effectiveness in the era of zero healthcare spending growth. Int J Equity Health. 2016;15:33.
Barbosa WB, de Costa JO, de Lemos LLP, Gomes RM, de Oliveira HN, Ruas CM, et al. Costs in the treatment of schizophrenia in adults receiving atypical antipsychotics: an 11-year cohort in Brazil. Appl Health Econ Health Policy [Internet]. 2018;16:697–709. https://doi.org/10.1007/s40258-018-0408-4 (Springer International Publishing).
Diniz IM, Guerra AA, de Lemos LLP, Souza KM, Godman B, Bennie M, et al. The long-term costs for treating multiple sclerosis in a 16-year retrospective cohort study in Brazil. PLoS One. 2018;13:1–14.
Faleiros DR, Álvares J, Almeida AM, de Araújo VE, Andrade EI, Godman BB, et al. Budget impact analysis of medicines: updated systematic review and implications. Expert Rev Pharmacoecon Outcomes Res. 2016;16(2):257–66. https://doi.org/10.1586/14737167.2016.1159958.
Vieira FS. Reflexões sobre o papel das unidades de economia da saúde no âmbito de sistemas nacionais de saúde. Saúde e Soc. 2016;25:306–19.
Ferreira-Da-Silva AL, Ribeiro RA, Santos VCC, Elias FTS, D’Oliveira ALP, Polanczyk CA. Diretriz para análises de impacto orçamentário de tecnologias em saúde no Brasil. Cad Saude Publica. 2012;28:1223–38.
Briceno V, Zaidi HA, Doucette JA, Onomichi KB, Alreshidi A, Mekary RA, et al. Efficacy of transsphenoidal surgery in achieving biochemical cure of growth hormone-secreting pituitary adenomas among patients with cavernous sinus invasion: a systematic review and meta-analysis. Neurol Res. 2017;39:387–98.
Almutairi RD, Muskens IS, Cote DJ, Dijkman MD, Kavouridis VK, Crocker E, et al. Gross total resection of pituitary adenomas after endoscopic vs. microscopic transsphenoidal surgery: a meta-analysis. Acta Neurochir (Wien). 2018;160(5):1005–21. https://doi.org/10.1007/s00701-017-3438-z.
Buchfelder M, Schlaffer S-M. The surgical treatment of acromegaly. Pituitary [Internet]. 2017;20:76–83. https://doi.org/10.1007/s11102-016-0765-7.
Gondim JA, Almeida JP, de Albuquerque LAF, Gomes E, Schops M, Ferraz T. Pure endoscopic transsphenoidal surgery for treatment of acromegaly: results of 67 cases treated in a pituitary center. Neurosurg Focus. 2010;29:E7.
Netuka D, Májovský M, Masopust V, Belšán T, Marek J, Kršek M, et al. Intraoperative magnetic resonance imaging during endoscopic transsphenoidal surgery of growth hormone-secreting pituitary adenomas. World Neurosurg. 2016;91:490–6.
Starnoni D, Daniel RT, Marino L, Pitteloud N, Levivier M, Messerer M. treatment of acromegaly according to the remission criteria: systematic review and meta-analysis. Acta Neurochir (Wien). 2010;2016:158.
Ruger JP, Reiff M. A checklist for the conduct, reporting, and appraisal of microcosting studies in health care: protocol development. JMIR Res Protoc. 2016;5:e195.
de Oliveira ML, Santos LMP, da Silva EN. Bases metodológicas para estudos de custos da doença no Brasil. Rev Nutr. 2014;27:585–95.
da Silva NE, Tolentino Silva M, Gomes Pereira M. Identificação, mensuração e valoração de custos em saúde. Epidemiol e Serviços Saúde. 2016;25:1–12.
Brasil. Ministério da Saúde. Secretaria de Ciência Tecnologia e Insumos Estratégicos. Departamento de Economia da Saúde. In: Programa Nacional de Gestão de Custos : manual técnico de custos – conceitos e metodologia. Brasília: Ministério da Saúde; 2006.
Ologunde R, Maruthappu M, Shanmugarajah K, Shalhoub J. Surgical care in low and middle-income countries: burden and barriers. Int J Surg. 2014;12:858–63.
Ahmadiani S, Nikfar S. Challenges of access to medicine and the responsibility of pharmaceutical companies: a legal perspective. DARU J Pharm Sci. 2016;24:13.
Banerji D, Das N, Sharma S, Jindal Y, Jain V, Behari S. Surgical management of acromegaly: long term functional outcome analysis and assessment of recurrent/residual disease. Asian J Neurosurg. 2016;11:261.
Fahlbusch R, Kleinberg D, Biller B, Bonert V, Buchfelder M, Cappabianca P, et al. Surgical debulking of pituitary adenomas improves responsiveness to octreotide lar in the treatment of acromegaly. Pituitary. 2017;20:668–75.
Gheorghiu ML, Găloiu S, Vintilă M, Purice M, Hortopan D, Dumitraşcu A, et al. Beneficial effect of dose escalation and surgical debulking in patients with acromegaly treated with somatostatin analogs in a Romanian tertiary care center. Hormones. 2016;15:224–34.
Colao A, Auriemma RS, Pivonello R, Kasuki L, Gadelha MR. Interpreting biochemical control response rates with first-generation somatostatin analogues in acromegaly. Pituitary. 2016;19:235–47.
Melmed S. Acromegaly. N Engl J Med. 2006;355:2558–73.
Alzhrani G, Sivakumar W, Park MS, Taussky P, Couldwell WT. Delayed complications after transsphenoidal surgery for pituitary adenomas. World Neurosurg. 2018;109:233–41. https://doi.org/10.1016/j.wneu.2017.09.192.
Agam MS, Wedemeyer MA, Wrobel B, Weiss MH, Carmichael JD, Zada G. Complications associated with microscopic and endoscopic transsphenoidal pituitary surgery: experience of 1153 consecutive cases treated at a single tertiary care pituitary center. J Neurosurg [Internet]. 2018. https://doi.org/10.3171/2017.12.JNS172318.
Newman CB, Melmed S, Snyder PJ, Young WF, Boyaiy LD, Levy R, et al. Safety and efficacy of long-term octreotide therapy of acromegaly: results of a multicenter trial in 103 patients—a clinical research center study. J Clin Endocrinol Metab. 1995;80:2768–75.
Acknowledgements
The authors acknowledge Dr Oswaldo Ribeiro Marquez Neto, Dr Luis Augusto Miranda Dias, Dr Jackson A. Gondim, Dr Luiz Augusto Casulari, Marcelo Neves, Ricardo Moreira, the Department of Health Costs of the Secretariat of Health of the Federal District and the Tribunal de Contas da União (TCU) for providing encouragement and support for this work.
Author information
Authors and Affiliations
Contributions
LBP contributed to the conceptualization of the study, data collection and writing of the manuscript. IRZ was responsible for the economic analysis and writing and reviewing the report. LAN contributed to the study design, clinical responsibilities, and writing and reviewing the report. All authors approved the manuscript.
Corresponding author
Ethics declarations
Porto LB, Zimmermann IR and Naves LA declare that they have no conflicts of interest. No funding was received for this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Porto, L.B., Zimmermann, I.R. & Naves, L.A. Economics of Acromegaly Treatment in Brazil: A Budget Impact Analysis of Pituitary Surgery Compared with Long-Term Octreotide LAR. PharmacoEconomics Open 3, 247–254 (2019). https://doi.org/10.1007/s41669-018-0103-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-018-0103-2