Abstract
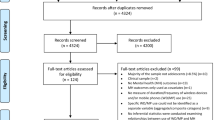
Sensors and wearables measure physiological and behavioral data in real time for behavioral health, using a variety of methods, interventions, and outcomes. A six-stage scoping review of 10 literature databases focused on keywords in four concept areas: (1) mobile technologies; (2) sensors, wearables, and remote monitoring; (3) mood and anxiety disorders, as well as stress; and (4) behavioral health care. Two authors independently screened results based on titles and abstracts, reviewed the full-text articles, and used inclusion/exclusion criteria to find research that studied self-report or management of symptoms and interventions. Out of a total of 5468 potential references, 76 papers were selected and an additional 16 studies were discovered in references. Of the 92 studies, 54 (58.7%) focused on mood (depressive, N = 28; bipolar, N = 26), 18 (19.6%) on anxiety disorders, and 20 (21.7%) on psychological stress/stress disorders. There were 7 (7.6%) randomized controlled trials, and 31 (33.7%) comparison studies. Research is shifting toward standardized methods, interventions, and evaluation measures, with longitudinal correlation, prediction, and/or biomarking/digital phenotyping of patients’ outcomes. These technologies pose several challenges for users, clinicians (e.g., selection, training, skills), healthcare systems (e.g., technology, integration into workflow, privacy), and organizations (e.g., training, creating a professional e-culture, change). Future research is needed on clinical health outcomes; human–computer interaction; medico-legal, professional, and privacy policy issues; models of service delivery; and effectiveness at a population level, across cultures, and related to economic costs. Clinician and institutional competencies could ensure quality of care, integration of missions, and institutional change.

Similar content being viewed by others
References
Abdullah, S., Matthews, M., Frank, E., Doherty, G., Gay, G., & Choudhury, T. (2016). Automatic detection of social rhythms in bipolar disorder. Journal of the American Medical Informatics Association, 23, 538–543.
Agarwal, S., LeFevre, A. E., Lee, J., L’Engle, K., Mehl, G., Sinha, C., Labrique, A., & WHO mHealth Technical Evidence Review Group. (2016). Guidelines for reporting of health interventions using mobile phones: mobile health (mHealth) evidence reporting and assessment (mERA) checklist. BMJ (Clinical Research Edition), 352, i1174. https://doi.org/10.1136/bmj.i1174
Agorastos, A., Boel, J. A., Heppner, P. S., Hager, T., Moeller-Bertram, T., Haji, U., et al. (2013). Diminished vagal activity and blunted diurnal variation of heart rate dynamics in posttraumatic stress disorder. Stress (Amsterdam, Netherlands), 16(3), 300–310. https://doi.org/10.3109/10253890.2012.7513692012.751369
Alvares, G. A., Quintana, D. S., Kemp, A. H., Van Zwieten, A., Balleine, B. W., Hickie, I. B., & Guastella, A. J. (2013). Reduced heart rate variability in social anxiety disorder: associations with gender and symptom severity. PLoS ONE, 8(7), e70468. https://doi.org/10.1371/journal.pone.0070468
Areàn, P. A., Ly, K. H., & Andersson, G. (2016). Mobile technology for mental health assessment. Dialogues in Clinical Neuroscience, 18(2), 163–169.
Ariga, K., Makita, T., Ito, M., Mori, T., Watanabe, S., & Takeya, J. (2019). Review of advanced sensor devices employing nanoarchitectonics concepts. Beilstein Journal of Nanotechnology, 10, 2014–2030.
Alvarez-Lozano, J., Osmani, V., Mayora-Ibarra, O., Frost, M., Bardram, J. E., Faurholt-Jepsen, M., & Kessing, L. V. (2014). Tell me your apps and I will tell you your mood: correlation of apps usage with bipolar disorder state. Pervasive Technologies Related to Assistive Environments, Article, 19, 1–7. https://doi.org/10.1145/2674396.2674408
Arksey, H., & O’Malley, L. (2005). Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32.
Armstrong, C., Blasko, K. A., Bush, N. E., Ciulla, R. Cooper, D. C., Edwards-Stewart, A., et al., & Skepp, N. A. (2018). DoD Mobile Health Practice Guide, 4th Edition.
Asselbergs, J., Ruwaard, J., Ejdys, M., Schrader, N., Sijbrandij, M., & Riper, H. (2016). Mobile phone-based unobtrusive ecological momentary assessment of day-to-day mood: an explorative study. Journal of Medical Internet Research, 18(3), e72. https://doi.org/10.2196/jmir.5505
Bandodkar, A. J., Jeerapan, I., & Wang, J. (2016). Wearable chemical sensors: present challenges and future prospects. ACS Sensors, 1, 464–482.
Bauer, M., Glenn, T., Geddes, J., Gitlin, M., Grof, P., Kessing, L. V., et al. (2020). Smartphones in mental health: a critical review of background issues, current status and future concerns. International Journal of Bipolar Disorders, 8(1), 2. https://doi.org/10.1186/s40345-019-0164-x
Bauer, M., Glenn, T., Monteith, S., Bauer, R., Whybrow, P. C., & Geddes, J. (2017). Ethical perspectives on recommending digital technology for patients with mental illness. International Journal of Bipolar Disorders, 5(1), 6. https://doi.org/10.1186/s40345-017-0073-9
Beer, R. D. (2000). Dynamical approaches to cognitive science. Trends in Cognitive Sciences, 4(3), 91–99. https://doi.org/10.1016/s1364-6613(99)01440-0
Beiwinkel, T., Kindermann, S., Maier, A., Kerl, C., Moock, J., Barbian, G., & Rössler, W. (2016). Using smartphones to monitor bipolar disorder symptoms: a pilot study. Journal of Medical Internet Research Mental Health, 3(1), e2. https://doi.org/10.2196/mental.4560
Bennett, C. C., Doub, T. W., & Selove, R. (2012). EHRs connect research and practice: where predictive modeling, artificial intelligence, and clinical decision support inter- sect. Health Policy and Technology, 1(2), 105–114.
Ben-Zeev, D., Scherer, E. A., Wang, R., Xie, H., & Campbell, A. T. (2015). Next-generation psychiatric assessment: using smartphone sensors to monitor behavior and mental health. Psychiatric Rehabilitation Journal, 38(3), 218–226. https://doi.org/10.1037/prj0000130
Berle, J. O., Hauge, E. R., Oedegaard, K. J., Holsten, F., & Fasmer, O. B. (2010). Actigraphic registration of motor activity reveals a more structured behavioural pattern in schizophrenia than in major depression. BMC Research Notes, 3, 149. https://doi.org/10.1186/1756-0500-3-149
Berrouiguet, S., Baca-García, E., Brandt, S., Walter, M., & Courtet, P. (2016). Fundamentals for future mobile-health (mHealth): a systematic review of mobile phone and web-based text messaging in mental health. Journal of Medical Internet Research, 18(6), e135. https://doi.org/10.2196/jmir.5066
Bogomolov, A., Lepri, B., Ferron, M., Pianesi, F., & Pentland, A. (2014). Daily stress recognition from mobile phone data, weather conditions and individual traits. MM 2014 - Proceedings of the 2014 ACM Conference on Multimedia. https://doi.org/10.1145/2647868.2654933
Bourla, A., Mouchabac, S., El Hage, W., & Ferreri, F. (2018). e-PTSD: an overview on how new technologies can improve prediction and assessment of posttraumatic stress disorder (PTSD). European Journal of Psychotraumatology, 9(sup1), 1424448. https://doi.org/10.1080/20008198.2018.14244482018.1424448
Burke, R. V., Andersen, M. N., Bowen, S. L., Howard, M. R., & Allen, K. D. (2010). Evaluation of two instruction methods to increase employment options for young adults with autism spectrum disorders. Research in Developmental Disabilities, 31(6), 1223–1233. https://doi.org/10.1016/j.ridd.2010.07.0232010.07.023
Burnham, J. P., Lu, C., Yaeger, L. H., Bailey, T. C., & Kollef, M. H. (2018). Using wearable technology to predict health outcomes: a literature review. Journal of the American Medical Informatics Association, 25(9), 1221–1227. https://doi.org/10.1093/jamia/ocy082
Burns, M. N., Begale, M., Duffecy, J., Gergle, D., Karr, C. J., Giangrande, E., & Mohr, D. C. (2011). Harnessing context sensing to develop a mobile intervention for depression. Journal of Medical Internet Research, 13(3), e55. https://doi.org/10.2196/jmir.18381838
Bush, N. E., Armstrong, C. M., & Hoyt, T. V. (2019). Smartphone apps for psychological health: a brief state of the science review. Psychological Services, 16(2), 188–195.
Canzian, L., & Musolesi, M. (2015). Trajectories of depression: unobtrusive monitoring of depressive states by means of smartphone mobility traces analysis. Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing.
Chan, S., Godwin, H., Gonzalez, A., Yellowlees, P. M., & Hilty, D. M. (2017). Review of use and integration of mobile apps into psychiatric treatments. Current Psychiatry Reports, 19(12), 96. https://doi.org/10.1007/s11920-017-0848-9
Chan, S., Li, L., Torous, J., Gratzer, D., & Yellowlees, P. M. (2018). Review of use of asynchronous technologies incorporated in mental health care. Current Psychiatry Reports, 20(10), 85. https://doi.org/10.1007/s11920-018-0954-3
Chang K. (2012). Speech analysis methodologies towards unobtrusive mental health monitoring (unpublished doctoral dissertation). University of California at Berkeley: USA. https://digitalassets.lib.berkeley.edu/techreports/ucb/text/EECS-2012-55.pdf2012-55.pdf2012-55.pdf
Chang, H. A., Chang, C. C., Tzeng, N. S., Kuo, T. B., Lu, R. B., & Huang, S. Y. (2013). Decreased cardiac vagal control in drug-naive patients with panic disorder: a case-control study in Taiwan. Asia-Pacific Psychiatry, 5(2), 80–89. https://doi.org/10.1111/appy.12032
Chow, P. I., Fua, K., Huang, Y., Bonelli, W., Xiong, H., Barnes, L. E., & Teachman, B. A. (2017). Using mobile sensing to test clinical models of depression, social anxiety, state affect, and social isolation among college students. Journal of Medical Internet Research, 19(3), e62. https://doi.org/10.2196/jmir.6820
Clark, A. (2013). Whatever next? Predictive brains, situated agents, and the future of cognitive science. Behavior Brain Science, 36(3), 181–204.
Cochran, A., Belman-Wells, L., & McInnis, M. (2018). Engagement strategies for self-monitoring symptoms of bipolar disorder with mobile and wearable technology: protocol for a randomized controlled trial. Journal of Medical Internet Research Research Protocols, 7(5), e130. https://doi.org/10.2196/resprot.9899
Cohen, H., Benjamin, J., Geva, A. B., Matar, M. A., Kaplan, Z., & Kotler, M. (2000). Autonomic dysregulation in panic disorder and in post-traumatic stress disorder: application of power spectrum analysis of heart rate variability at rest and in response to recollection of trauma or panic attacks. Psychiatry Research, 96(1), 1–13. https://doi.org/10.1016/s0165-1781(00)00195-5
Cohen, H., Kotler, M., Matar, M. A., Kaplan, Z., Miodownik, H., & Cassuto, Y. (1997). Power spectral analysis of heart rate variability in posttraumatic stress disorder patients. Biological Psychiatry, 41(5), 627–629. https://doi.org/10.1016/s0006-3223(96)00525-2
Coppersmith, G., Leary, R., Crutchley, P., & Fine, A. (2018). Natural language processing of social media as screening for suicide risk. Biomedical informatics insights, 10, 1178222618792860. https://doi.org/10.1177/1178222618792860
Cormack, F., McCue, M., Taptiklis, N., Skirrow, C., Glazer, E., Panagopoulos, E., et al. (2019). Wearable technology for high-frequency cognitive and mood assessment in major depressive disorder: longitudinal observational study. Journal of Medical Internet Research Mental Health, 6(11), e12814. https://doi.org/10.2196/12814
Cornet, V. P., & Holden, R. J. (2018). Systematic review of smartphone-based passive sensing for health and wellbeing. Journal of Biomedical Informatics, 77, 120–132. https://doi.org/10.1016/j.jbi.2017.12.0082017.12.008
Coronato, A., De Pietro, G., & Paragliola, G. (2014). A situation-aware system for the detection of motion disorders of patients with autism spectrum disorders. Expert Systems with Applications, 41, 7868–7877. https://doi.org/10.1016/j.eswa.2014.05.0112014.05.011
Cummins, N., Epps, J., & Ambikairajah, E. (2013). Spectro-temporal analysis of speech affected by depression and psychomotor retardation. 2013 IEEE International Conference on Acoustics, Speech and Signal Processing, Vancouver, BC, 2013, pp. 7542–7546, doi: https://doi.org/10.1109/ICASSP.2013.66391292013.6639129
Curran, G. M., Bauer, M., Mittman, B., Pyne, J. M., & Stetler, C. (2012). Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care, 50(3), 217–226. https://doi.org/10.1097/MLR.0b013e3182408812
Demasi, O., Aguilera, A., & Recht, B. (2016). Detecting change in depressive symptoms from daily wellbeing questions, personality, and activity. 2016 IEEE Wireless Health (WH). Bethesda, MD, 2016, 1–8. https://doi.org/10.1109/WH.2016.77645522016.7764552
Depp, C. A., Ceglowski, J., Wang, V. C., Yaghouti, F., Mausbach, B. T., Thompson, W. K., & Granholm, E. L. (2015). Augmenting psychoeducation with a mobile intervention for bipolar disorder: a randomized controlled trial. Journal of Affective Disorders, 174, 23–30. https://doi.org/10.1016/j.jad.2014.10.0532014.10.053
Depp, C., Torous, J., & Thompson, W. (2016). Technology-based early warning systems for bipolar disorder: a conceptual framework. Journal of Medical Internet Research Mental Health, 3(3), e42. https://doi.org/10.2196/mental.5798
Dibia V. (2016). FOQUS: A smartwatch application for individuals with ADHD and mental health challenges. Proceedings of the 18th International ACM SIGACCESS Conf Comp Accessibility – ASSETS. Pp. 311–312. https://doi.org/10.1145/2982142.2982207
Dickerson, F. B., Stallings, C., Origoni, A., Boronow, J. J., Sullens, A., & Yolken, R. (2008). Predictors of occupational status six months after hospitalization in persons with a recent onset of psychosis. Psychiatric Research, 160(3), 278–284. https://doi.org/10.1016/j.psychres.2007.07.0302007.07.030
Dillon, A., Kelly, M., Robertson, I. H., & Robertson, D. A. (2016). Smartphone applications utilizing biofeedback can aid stress reduction. Frontiers in Psychology, 7, 832. https://doi.org/10.3389/fpsyg.2016.008322016.00832
Dinh-Le, C., Chuang, R., Chokshi, S., & Mann, D. (2019). Wearable health technology and electronic health record integration: Scoping review and future directions. Journal of Medical Internet Research mhealth uhealth, 7(9), e12861. https://doi.org/10.2196/12861
Dogan, E., Sander, C., Wagner, X., et al. (2017). Smartphone-based monitoring of objective and subjective data in affective disorders: Where are we and where are we going? systematic review. Journal of Medical Internet Research, 19(7), e262. https://doi.org/10.2196/jmir.7006
Doryab, A., Min, J., Wiese, J., Zimmerman, J., & Hong, J.I. (2014). Detection of behavior change in people with depression. AAAI Workshop: Modern Artificial Intelligence for Health Analytics: Papers from the AAAI-14. Quebec, Canada, pp. 12.
Doryab, A., Villalba, D. K., Chikersal, P., Dutcher, J. M., Tumminia, M., Liu, X., et al. (2019). Identifying behavioral phenotypes of loneliness and social isolation with passive sensing: statistical analysis, data mining and machine learning of smartphone and Fitbit data. Journal of Medical Internet Research mhealth uhealth, 7(7), e13209. https://doi.org/10.2196/13209
Eagle, N., Pentland, A. S., & Lazer, D. (2009). Inferring friendship network structure by using mobile phone data. Proceedings of the National Academy of Sciences of the United States of America, 106(36), 15274–15278. https://doi.org/10.1073/pnas.0900282106
Edwards, M. K., & Loprinzi, P. D. (2016). Effects of a sedentary behavior-inducing randomized controlled intervention on depression and mood profile in active young adults. Mayo Clinic Proceedings, 91(8), 984–998. https://doi.org/10.1016/j.mayocp.2016.03.0212016.03.021
Edwards-Stewart, A., Alexander, C., Armstrong, C. M., Hoyt, T., & O’Donohue, W. (2019). Mobile applications for client use: Ethical and legal considerations. Psychological Services, 16(2), 281–285. https://doi.org/10.1037/ser0000321
Elgendi, M., & Menon, C. (2019). Assessing anxiety disorders using wearable devices: challenges and future directions. Brain Sciences, 9(3), 50. https://doi.org/10.3390/brainsci9030050
Faurholt-Jepsen, M., Bauer, M., & Kessing, L. V. (2018). Smartphone-based objective monitoring in bipolar disorder: Status and considerations. International Journal of Bipolar Disorders, 6(1), 6. https://doi.org/10.1186/s40345-017-0110-8
Faurholt-Jepsen, M., Frost, M., Christensen, E. M., Bardram, J. E., Vinberg, M., & Kessing, L. V. (2020). The effect of smartphone-based monitoring on illness activity in bipolar disorder: The MONARCA II randomized controlled single-blinded trial. Psychological Medicine, 50(5), 838–848. https://doi.org/10.1017/S0033291719000710
Faurholt-Jepsen, M., Frost, M., Martiny, K., Tuxen, N., Rosenberg, N., Busk, J., et al. (2017). Reducing the rate and duration of Re-ADMISsions among patients with unipolar disorder and bipolar disorder using smartphone-based monitoring and treatment - The RADMIS trials: Study protocol for two randomized controlled trials. Trials, 18(1), 277. https://doi.org/10.1186/s13063-017-2015-32015-3
Faurholt-Jepsen, M., Frost, M., Vinberg, M., Christensen, E. M., Bardram, J. E., & Kessing, L. V. (2014). Smartphone data as objective measures of bipolar disorder symptoms. Psychiatry Research, 217(1–2), 124–127. https://doi.org/10.1016/j.psychres.2014.03.0092014.03.009
Faurholt-Jepsen, M., Munkholm, K., Frost, M., Bardram, J. E., & Kessing, L. V. (2016). Electronic self-monitoring of mood using IT platforms in adult patients with bipolar disorder: A systematic review of the validity and evidence. BMC Psychiatry, 16(1), 7. https://doi.org/10.1186/s12888-016-0713-0
Fraccaro, P., Beukenhorst, A., Sperrin, M., Harper, S., Palmier-Claus, J., Lewis, S., et al. (2019). Digital biomarkers from geolocation data in bipolar disorder and schizophrenia: a systematic review. Journal of the American Medical Informatics Association, 26(11), 1412–1420. https://doi.org/10.1093/jamia/ocz043
Gaggioli, A., Pallavicini, F., Morganti, L., Serino, S., Scaratti, C., Briguglio, M., et al. (2014). Experiential virtual scenarios with real-time monitoring (interreality) for the management of psychological stress: A block randomized controlled trial. Journal of Medical Internet Research, 16(7), e167. https://doi.org/10.2196/jmir.3235
Gaglani, S. M., & Topol, E. J. (2014). iMedEd: The role of mobile health technologies in medical education. Academic Medicine, 89(9), 1207–1209. https://doi.org/10.1097/ACM.0000000000000361
Galambos, C., Skubic, M., Wang, S., & Rantz, M. (2013). Management of dementia and depression utilizing in-home passive sensor data. Gerontechnology, 11(3), 457–468. https://doi.org/10.4017/gt.2013.11.3.004.002013.11.3.004.00
Garcia-Ceja, E., Riegler, M., Nordgreen, T., Jakobsen, P., Oedegaard, K. J., & Tørresen, J. (2018). Mental health monitoring with multimodal sensing and machine learning: A survey. Pervasive Mobile Computing, 51, 1–26.
Gargon, E., Gorst, S. L., & Williamson, P. R. (2019). Choosing important health outcomes for comparative effectiveness research: 5th annual update to a systematic review of core outcome sets for research. PLoS ONE, 14(12), e0225980. https://doi.org/10.1371/journal.pone.0225980
Gentry, T., Kriner, R., Sima, A., McDonough, J., & Wehman, P. (2015). Reducing the need for personal supports among workers with autism using an iPod Touch as an assistive technology: Delayed randomized control trial. Journal of Autism and Developmental Disorders, 45(3), 669–684. https://doi.org/10.1007/s10803-014-2221-8
Gershon, A., Ram, N., Johnson, S. L., Harvey, A. G., & Zeitzer, J. M. (2016). Daily actigraphy profiles distinguish depressive and interepisode states in bipolar disorder. Clinical Psychological Science, 4(4), 641–650. https://doi.org/10.1177/2167702615604613
Gideon, J., Provost, E. M., & McInnis, M. (2016). Mood state prediction from speech of varying acoustic quality for individuals with bipolar disorder. Proceedings of the IEEE International Conference on Acoustics, Speech, and Signal Processing. ICASSP (Conference), 2016, 2359–2363. https://doi.org/10.1109/ICASSP.2016.74720992016.7472099
Gonnermann, A., von Jan, U., & Albrecht, U. V. (2015). Draft guideline for the development of evidence based medicine-related apps. Studies in Health Technology and Informatics, 210, 637–641.
Gonzalez, R., Tamminga, C. A., Tohen, M., & Suppes, T. (2014). The relationship between affective state and the rhythmicity of activity in bipolar disorder. The Journal of Clinical Psychiatry, 75(4), e317–e322. https://doi.org/10.4088/JCP.13m08506
Greenes, R. A., Bates, D. W., Kawamoto, K., Middleton, B., Osheroff, J., & Shahar, Y. (2018). Clinical decision support models and frameworks: seeking to address research issues underlying implementation successes and failures. Journal of Biomedical Informatics, 78, 134–143.
Grekin, E. R., Beatty, J. R., & Ondersma, S. J. (2019). Mobile health interventions: exploring the use of common relationship factors. Journal of Medical Internet Research mhealth uhealth, 7(4), e11245. https://doi.org/10.2196/11245
Grundy, Q. H., Wang, Z., & Bero, L. A. (2016). Challenges in assessing mobile health app quality: A systematic review of prevalent and innovative methods. American Journal of Preventive Medicine, 51(6), 1051–1059. https://doi.org/10.1016/j.amepre.2016.07.0092016.07.009
Grünerbl, A., Muaremi, A., Osmani, V., Bahle, G., Ohler, S., Tröster, G., et al. (2015). Smartphone-based recognition of states and state changes in bipolar disorder patients. IEEE Journal of Biomedical and Health Informatics, 19(1), 140–148.
Grünerbl, A., & Oleksy, P., & Bahle, G.,& Haring, C., & Weppner, J., & Lukowicz, P. (2012). Towards smart phone based monitoring of bipolar disorder. Proceedings of the Second ACM Workshop on Mobile Systems, Applications, and Services for HealthCare - mHealthSys '12. https://doi.org/10.1145/2396276.2396280
Grünerbl, A., Osmani, V., Bahle, G., Carrasco-Jiménez, J.C., Ohler, S., Mayora-Ibarra, O., Haring, C., & Lukowicz, P. (2014). Using smart phone mobility traces for the diagnosis of depressive and manic episodes in bipolar patients. AH '14.
Gu, Y., Zhang, T., Chen, H., Wang, F., Pu, Y., Gao, C., & Li, S. (2019). Mini review on flexible and wearable electronics for monitoring human health information. Nanoscale Research Letters, 14(1), 263. https://doi.org/10.1186/s11671-019-3084-x
Guidi, A., Schoentgen, J., Bertschy, G., Gentili, C., Landini, L., Scilingo, E. P., & Vanello, N. (2015). Voice quality in patients suffering from bipolar disease. Conference Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference, 2015, 6106–6109. https://doi.org/10.1109/EMBC.2015.73197852015.7319785
Gurchiek, R. D., Cheney, N., & McGinnis, R. S. (2019). Estimating biomechanical time-series with wearable sensors: a systematic review of machine learning techniques. Sensors (Basel), 19(23), 5227. https://doi.org/10.3390/s19235227
Harrison, R., Flood, D., & Duce, D. (2013). Usability of mobile applications: Literature review and rationale for a new usability model. Journal of Interactive Science, 1(1), 1–16.
Hartanto, D., Brinkman, W., Kampmann, I.L., Morina, N., Emmelkamp, P.G., & Neerincx, M.A. (2015). Home-based virtual reality exposure therapy with virtual health agent support. In S. Serino, A. Matic, D. Giakoumis, G. Lopez, P. Cipresso (Eds), Pervasive computing paradigms for mental health. mindcare 2015. communications in computer and information science, volume 604. Cham: Springer.
Hauge, E. R., Berle, J. Ø., Oedegaard, K. J., Holsten, F., & Fasmer, O. B. (2011). Nonlinear analysis of motor activity shows differences between schizophrenia and depression: A study using Fourier analysis and sample entropy. PLoS ONE, 6(1), e16291. https://doi.org/10.1371/journal.pone.0016291
Hauschildt, M., Peters, M. J., Moritz, S., & Jelinek, L. (2011). Heart rate variability in response to affective scenes in posttraumatic stress disorder. Biological Psychology, 88(2–3), 215–222. https://doi.org/10.1016/j.biopsycho.2011.08.0042011.08.004
Heikenfeld, J., Jajack, A., Rogers, J., Gutruf, P., Tian, L., Pan, T., et al. (2018). Wearable sensors: modalities, challenges, and prospects. Laboratory Chip, 18, 217–248.
Henriques, G., Keffer, S., Abrahamson, C., & Horst, S. J. (2011). Exploring the effectiveness of a computer-based heart rate variability biofeedback program in reducing anxiety in college students. Applied Psychophysiology and Biofeedback, 36(2), 101–112. https://doi.org/10.1007/s10484-011-9151-4
Hersh, W. R., Gorman, P. N., Biagioli, F. E., Mohan, V., Gold, J. A., & Mejicano, G. C. (2014). Beyond information retrieval and electronic health record use: competencies in clinical informatics for medical education. Advances in Medical Education and Practice, 5, 205–212. https://doi.org/10.2147/AMEP.S63903
Hilty, D. M., Chan, S., Torous, J., Mahautmr, J., & Mucic, D. M. (2015). New frontiers in healthcare and technology: Internet- and web-based mental options emerge to complement in-person and telepsychiatric care options. Journal of Health and Medical Informatics, 6(4), 1–14.
Hilty, D. M., Chan., S., Torous, J., Luo, J., Boland, R. (2019). A telehealth framework for mobile health, smartphones and apps: Competencies, training and faculty development. Journal of Technology in Behavioral Science, 4(2), 106–123. https://doi.org/10.1007/s41347-019-00091-0
Hilty, D. M., Chan, S., Torous, J., Luo, J., Boland, R. J. (2020). A framework for competencies for the use of mobile technologies in psychiatry and medicine. Journal of Medical Internet Research uhealth and mHealth, 2020; 8(2). http://mhealth.jmir.org/2020/2/e12229/2020/2/e12229/
Hilty, D. M., Crawford, A., Teshima, J., Chan, S., Sunderji, N., & Yellowlees, P. M. (2015). A framework for telepsychiatric training and e-health: Competency-based education, evaluation and implications. International Review of Psychiatry, 27(6), 569–592.
Hilty, D. M., Ferrer, D. C., Parish, M. B., Johnston, B., Callahan, E. J., & Yellowlees, P. M. (2013). The effectiveness of telemental health: a 2013 review. Telemedicine Journal and E-Health, 19(6), 444–454. https://doi.org/10.1089/tmj.2013.00752013.0075
Hilty, D. M., Gentry, M. T., McKean, A. J., Cowan, K. E., Lim, R. F., & Lu, F. G. (2020). Telehealth for rural diverse populations: Telebehavioral and cultural competencies, clinical outcomes and administrative approaches. mHealth, 6, 20. https://doi.org/10.21037/mhealth.2019.10.042019.10.04
Hilty, D. M., Liu, H. Y., Stubbe, D., & Teshima, J. (2019). Defining professional development in medicine, psychiatry, and allied fields. Psychiatric Clinics of North America, 42(3), 337–356. https://doi.org/10.1016/j.psc.2019.04.0012019.04.001
Hilty, D. M., Maheu, M. M., Drude, K. P., & Hertlein, K. M. (2018). The need to implement and evaluate telehealth competency frameworks to ensure quality care across behavioral health professions. Academic Psychiatry, 42(6), 818–824. https://doi.org/10.1007/s40596-018-0992-5
Hilty, D. M., Parish, M., Chan, S., Xiong, G., Scher, L., & Yellowlees, P. M. (2020). A comparison of in-person, synchronous and asynchronous telepsychiatry: Skills/competencies, teamwork and administrative workflow. Journal of Technology in Behavioral Science, 2020. https://doi.org/10.1007/s41347-020-00137-8
Hilty, D. M., Rabinowitz, T. R., McCarron, R. M., Katzelnick, D. J., Chang, B., A. M., & Fortney, J. , et al. (2018). Telepsychiatry and e-mental health models leverage stepped, collaborative, and integrated services to primary care. Psychosomatics, 59(3), 227–250.
Hilty, D. M., Torous, J., Parish, M., Chan, S., Xiong, G., Scher, L., & Yellowlees, P. M. (2020). A literature review comparing clinicians’ approaches and skills to in-person, synchronous and asynchronous care: Moving toward asynchronous competencies to ensure quality care. Telemedicine Journal and E-Health, 2020 https://doi.org/10.1089/tmj.2020.0054
Hilty, D. M., Uno, J., Chan, S., Torous, J., & Boland, R. J. (2019). Role of technology in faculty development in psychiatry. The Psychiatric Clinics of North America, 42(3), 493–512. https://doi.org/10.1016/j.psc.2019.05.0132019.05.013
Hilty, D. M., Unützer, J., Ko, D. G., Luo, J., Worley, L., & Yager, J. (2019). Approaches for departments, schools, and health systems to better implement technologies used for clinical care and education. Academic Psychiatry, 43(6), 611–616. https://doi.org/10.1007/s40596-019-01074-2
Hilty, D. M., Zalpuri, I., Stubbe, D., Snowdy, C. E., Shoemaker, E. Z., Joshi, S. V., et al. (2018). Social media/networking as part of e-behavioral health and psychiatric education: Competencies, teaching methods, and implications. Journal of Technology in Behavioral Science, 3(4), 268–293.
Hobson, G. R., Caffery, L. J., Neuhaus, M., & Langbecker, D. H. (2019). Mobile health for First Nations Populations: Systematic review. Journal of Medical Internet Research mHealth and uHealth, 7(10), e14877. https://doi.org/10.2196/14877
Huang, Y., Xiong, H., Leach, K., Zhang, Y., Chow, P.I., Fua, K.C., et al., & Barnes, L.E. (2016). Assessing social anxiety using GPS trajectories and point-of-interest data. Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing.
Insel, T. R. (2017). Digital phenotyping: Technology for a new science of behavior. Journal of the American Medical Association, 318(13), 1215–1216. https://doi.org/10.1001/jama.2017.112952017.11295
Kamišalić, A., Fister, I., Jr., Turkanović, M., & Karakatič, S. (2018). Sensors and functionalities of non-invasive wrist-wearable devices: A review. Sensors (Basel, Switzerland), 18(6), 1714. https://doi.org/10.3390/s18061714
Karam, Z. N., Provost, E. M., Singh, S., Montgomery, J., Archer, C., Harrington, G., & Mcinnis, M. G. (2014). Ecologically valid long-term mood monitoring of individuals with bipolar disorder using speech. Proceedings of the IEEE International Conference on Acoustics, Speech, and Signal Processing. ICASSP (Conference), 2014, 4858–4862. https://doi.org/10.1109/ICASSP.2014.68545252014.6854525
Kidholm, K., Jensen, L. K., Kjølhede, T., Nielsen, E., & Horup, M. B. (2018). Validity of the model for assessment of telemedicine: A Delphi study. Journal of Telemedicine and Telecare, 24(2), 118–125. https://doi.org/10.1177/1357633X16686553
Kirchner, T. R., & Shiffman, S. (2016). Spatio-temporal determinants of mental health and well-being: advances in geographically-explicit ecological momentary assessment (GEMA). Social Psychiatry and Psychiatric Epidemiology, 51(9), 1211–1223. https://doi.org/10.1007/s00127-016-1277-5
Knight, A., & Bidargaddi, N. (2018). Commonly available activity tracker apps and wearables as a mental health outcome indicator: A prospective observational cohort study among young adults with psychological distress. Journal of Affective Disorders, 236, 31–36. https://doi.org/10.1016/j.jad.2018.04.0992018.04.099
Kumari, P., Mathew, L., & Syal, P. (2017). Increasing trend of wearables and multimodal interface for human activity monitoring: A review. Biosensors and Bioelectronics, 90, 298–307.
Kvedar, J., Coye, M. J., & Everett, W. (2014). Connected health: A review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Affairs (Millwood), 33(2), 194–199.
Lavoie, K.L., Fleet, R.P., Laurin, C., Arsenault, A., Miller, S.B., Bacon, S.L. (2004). Heart rate variability in coronary artery disease patients with and without panic disorder. Psychiatry Research, 128, 289–299.
Levac, D., Colquhoun, H., & O’Brien, K. K. (2010). Scoping studies: Advancing the methodology. Implementation Science, 5, 69. https://doi.org/10.1186/1748-5908-5-69
Liddy, C., Drosinis, P., & Keely, E. (2016). Electronic consultation systems: Worldwide prevalence and their impact on patient care-a systematic review. Family Practice, 33(3), 274–285. https://doi.org/10.1093/fampra/cmw024
Lim, Y. H., Kim, H., Kim, J. H., Bae, S., Park, H. Y., & Hong, Y. C. (2012). Air pollution and symptoms of depression in elderly adults. Environmental Health Perspectives, 120(7), 1023–1028. https://doi.org/10.1289/ehp.1104100
Loncar-Turukalo, T., Zdravevski, E., Silva, J., Chouvarda, I., & Traijkovik, V. (2019). Literature on wearable technology for connected health: Scoping review of research trends, advances, and barriers. Journal of Medical Internet Research, 21(9), e14017. https://doi.org/10.2196/14017
Luxton, D. D. (2016). Artificial intelligence in behavioral health care. Boston, MA: Elsevier.
Luxton, D. D., June, J. D., & Chalker, S. A. (2015). Mobile health technologies for suicide prevention: Feature review and recommendations for use in clinical care. Current Treatment Options in Psychology, 2, 349–362. https://doi.org/10.1007/s40501-015-0057-2
Luxton, D. D., June, J. D., Sano, A., & Bickmore, T. (2016). Intelligent mobile, wearable, and ambient technologies for behavioral health care. In D. D. Luxton (Ed.), Artificial intelligence in behavioral and mental health care (pp. 137–162). Cambridge, MA: Elsevier Academic Press. https://doi.org/10.1016/B978-0-12-420248-1.00006-4
Luxton, D. D., Kayl, R. A., & Mishkind, M. C. (2012). mHealth data security: The need for HIPAA-compliant standardization. Telemedicine Journal and E-Health, 18(4), 284–288. https://doi.org/10.1089/tmj.2011.01802011.0180
Luxton, D. D., McCann, R. A., Bush, N. E., Mishkind, M. C., & Reger, G. M. (2011). mHealth for mental health: Integrating smartphone technology in behavioral healthcare. Professional Psychology: Research and Practice, 42(6), 505–512. https://doi.org/10.1037/a0024485
Ma, Y., Xu, B., Bai, Y., Sun, G., & Zhu, R. (2014). Infer daily mood using mobile phone sensing. Ad Hoc Sensor Wireless Network, 20, 133–152.
Maddison, R., Cartledge, S., Rogerson, M., Goedhart, N. S., Ragbir Singh, T., Neil, & Ball, K. , et al. (2019). Usefulness of wearable cameras as a tool to enhance chronic disease self-management: Scoping review. Journal of Medical Internet Research mhealth uhealth, 7(1), e10371. https://doi.org/10.2196/10371
Mahendran, N., Vincent, D. R., Srinivasan, K., Chang, C. Y., Garg, A., Gao, L., & Reina, D. G. (2019). Sensor-assisted weighted average ensemble model for detecting major depressive disorder. Sensors (Basel, Switzerland), 19(22), 4822. https://doi.org/10.3390/s19224822
Maheu M., Drude, K., Hertlein, K., Lipschutz, R., Wall, K., Long, R., et al., & Hilty, D. M. (2019). An interdisciplinary framework for telebehavioral health competencies. Journal of Technology in Behavioral Science, 3(2), 108–40; correction 3(2):107. https://doi.org/10.1007/s41347-019-00113
Maheu, M., Drude, K., Hertlein, K. M., & Hilty, D. M. (2018). A framework for interprofessional telebehavioral health competencies: Implementation and challenges moving forward. Academic Psychiatry, 42(6), 825–833.
Maxhuni, A., Muñoz-Meléndez, A., Osmani, V., Perez, H., Mayora-Ibarra, O., & Morales, E. F. (2016). Classification of bipolar disorder episodes based on analysis of voice and motor activity of patients. Pervasive Mobile Computing, 31, 50–66.
Marcolino, M. S., Alkmim, M. B., Pessoa, C. G., Maia, J. X., & Cardoso, C. S. (2019). Development and implementation of a methodology for quality assessment of asynchronous teleconsultations. Telemedicine Journal & E-Health, 26(5). https://doi.org/10.1089/tmj.2019.00492019.0049
McCraty, R., Atkinson, M., Tomasino, D., & Stuppy, W. P. (2001). Analysis of twenty-four hour heart rate variability in patients with panic disorder. Biological Psychology, 56(2), 131–150. https://doi.org/10.1016/s0301-0511(01)00074-6
McIntyre, R. S., Cha, D. S., Jerrell, J. M., Swardfager, W., Kim, R. D., Costa, L. G., et al. (2014). Advancing biomarker research: utilizing ‘Big Data’ approaches for the characterization and prevention of bipolar disorder. Bipolar Disorders, 16(5), 531–547. https://doi.org/10.1111/bdi.12162
Mehrotra, A., Hendley, R.J., & Musolesi, M. (2016). Towards multi-modal anticipatory monitoring of depressive states through the analysis of human-smartphone interaction. Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing: Adjunct.
Miles, A., & Mezzich, J. (2011). The care of the patient and the soul of the clinic: Person-centered medicine as an emergent model of modern clinical practice. International Journal of Person Centered Medicine, 1, 207–222.
Mohr, D., Zhang, M., & Schueller, S. (2017). Personal sensing: understanding mental health using ubiquitous sensors and machine learning. Annual Review of Clinical Psychology, 13, 23–47.
Mostaghimi, A., Olszewski, A. E., Bell, S. K., Roberts, D. H., & Crotty, B. H. (2017). Erosion of digital professionalism during medical students’ core clinical clerkships. Journal of Medical Internet Research Medical Education, 3(1), e9. https://doi.org/10.2196/mededu.6879
Muaremi, A., Gravenhorst, F., Grünerbl, A., Arnrich, B., & Tröster, G. (2014). Assessing bipolar episodes using speech cues derived from phone calls. In P. Cipresso, G. Matic, & G. Lopez (Eds.), Pervasive computing paradigms for mental health (pp. 103–114). Cham: Springer.
Naslund, J. A., Aschbrenner, K. A., & Bartels, S. J. (2016). Wearable devices and smartphones for activity tracking among people with serious mental illness. Mental Health and Physical Activity, 10, 10–17.
Novák, D., Albert, F., & Španiel, F. (2014). Analysis of actigraph parameters for relapse prediction in bipolar disorder: a feasibility study. Conference Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference, 2014, 4972–4975. https://doi.org/10.1109/EMBC.2014.69447402014.6944740
O’Brien, J. T., Gallagher, P., Stow, D., Hammerla, N., Ploetz, T., Firbank, M., et al. (2017). A study of wrist-worn activity measurement as a potential real-world biomarker for late-life depression. Psychological Medicine, 47(1), 93–102. https://doi.org/10.1017/S0033291716002166
O'Keefe, M., White, K., & Jennings, J. C. (2019). Asynchronous telepsychiatry: A systematic review. Journal of Telemedicine and Telecare, 1357633X19867189. Advance online publication. https://doi.org/10.1177/1357633X19867189
Onnela, J. P., & Rauch, S. L. (2016). Harnessing smartphone-based digital phenotyping to enhance behavioral and mental health. Neuropsychopharmacology, 41(7), 1691–1696. https://doi.org/10.1038/npp.2016.72016.7
Osmani, V. (2015). Smartphones in mental health: Detecting depressive and manic episodes. IEEE Pervasive Computing, 14, 10–13.
Osmani, V., Maxhuni, A., Grünerbl, A., Lukowicz, P., Haring, C., & Mayora, O. (2013). Monitoring activity of patients with bipolar disorder using smart phones. ACM International Conference Proceeding Series., 85(85–85), 92. https://doi.org/10.1145/2536853.2536882.
Pallavicini, F., Algeri, D., Repetto, C., Gorini, A., & Riva, G. (2009). Biofeedback, virtual reality and mobile phones in the treatment of generalized anxiety disorder (gad): A phase-2 controlled clinical trial. Journal of Cyber Therapy and Rehabilitation, 2(4), 315–327.
Palmius, N., Tsanas, A., Saunders, K., Bilderbeck, A. C., Geddes, J. R., Goodwin, G. M., & De Vos, M. (2017). Detecting bipolar depression from geographic location data. IEEE Transactions on Bio-Medical Engineering, 64(8), 1761–1771. https://doi.org/10.1109/TBME.2016.2611862.
Patel, V. L., Kaufman, D. R., & Arocha, J. F. (2002). Emerging paradigms of cognition in medical decision-making. Journal of Biomedical Informatics, 35(1), 52–75.
de Peralta, A. M., Gillispie, M., Mobley, C., & Gibson, L. M. (2019). It’s all about trust and respect: Cultural competence and cultural humility in mobile health clinic services for underserved minority populations. Journal of Health Care for the Poor and Underserved, 30(3), 1103–1118. https://doi.org/10.1353/hpu.2019.0076.
Petrowski, K., Herold, U., Joraschky, P., Mück-Weymann, M., Siepmann, M. (2010). The effects of psychosocial stress on heart rate variability in panic disorder. Geriatric Journal of Psychiatry, 13, 66–73.
Pittig, A., Arch, J. J., Lam, C. W., & Craske, M. G. (2013). Heart rate and heart rate variability in panic, social anxiety, obsessive-compulsive, and generalized anxiety disorders at baseline and in response to relaxation and hyperventilation. International Journal of Psychophysiology, 87(1), 19–27. https://doi.org/10.1016/j.ijpsycho.2012.10.0122012.10.012
Place, S., Blanch-Hartigan, D., Rubin, C., Gorrostieta, C., Mead, C., Kane, J., et al. (2017). Behavioral indicators on a mobile sensing platform predict clinically validated psychiatric symptoms of mood and anxiety disorders. Journal of Medical Internet Research, 19(3), e75. https://doi.org/10.2196/jmir.6678
Ponzo, S., Morelli, D., Kawadler, J. M., Hemmings, N. R., Bird, G., & Plans, D. (2020). Efficacy of the digital therapeutic mobile app biobase to reduce stress and improve mental well-being among university students: randomized controlled trial. Journal of Medical Internet Research mhealth uhealth, 8(4), e17767. https://doi.org/10.2196/17767
Pratap, A., Renn, B. N., Volponi, J., Mooney, S. D., Gazzaley, A., Arean, P. A., & Anguera, J. A. (2018). Using mobile apps to assess and treat depression in hispanic and latino populations: Fully remote randomized clinical trial. Journal of Medical Internet Research, 20(8), e10130. https://doi.org/10.2196/10130
Prociow, P. A., & Crowe, J. A. (2010). Towards personalised ambient monitoring of mental health via mobile technologies. Technology and Health Care, 18(4–5), 275–284. https://doi.org/10.3233/THC-2010-05902010-0590
Proctor, E., Silmere, H., Raghavan, R., Raghavan, R., Hovmand, P., Aarons, G., et al. (2010). Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administrative Policy in Mental Health, 38(2), 65–76.
Quiroz, J. C., Geangu, E., & Yong, M. H. (2018). Emotion recognition using smart watch sensor data: Mixed-design study. Journal of Medical Internet Research Mental Health, 5(3), e10153. https://doi.org/10.2196/10153
Ravizza, A., De Maria, C., Di Pietro, L., Sternini, F., Audenino, A. L., & Bignardi, C. (2019). Comprehensive review on current and future regulatory requirements on wearable sensors in preclinical and clinical testing. Frontiers in Bioengineering and Biotechnology, 7, 313. https://doi.org/10.3389/fbioe.2019.003132019.00313
Ray, G., Muhanna, W. A., & Barney, J. B. (2007). Competing with IT: the role of shared IT-business understanding. Communications of the ACM, 50, 87–91.
Reichert, M., Lutz, A., Deuschle, M., Gilles, M., Hill, H., Limberger, M. F., & Ebner-Priemer, U. W. (2015). Improving motor activity assessment in depression: which sensor placement, analytic strategy and diurnal time frame are most powerful in distinguishing patients from controls and monitoring treatment effects. PLoS ONE, 10(4), e0124231. https://doi.org/10.1371/journal.pone.0124231
Renn, B. N., Pratap, A., Atkins, D. C., Mooney, S. D., & Areán, P. A. (2018). Smartphone-based passive assessment of mobility in depression: Challenges and opportunities. Mental Health and Physical Activity, 14, 136–139. https://doi.org/10.1016/j.mhpa.2018.04.0032018.04.003
Rogers, E. M. (1998). Diffusion of innovations (5th ed.). New York, NY: Free Press.
Rohani, D. A., Faurholt-Jepsen, M., Kessing, L. V., & Bardram, J. E. (2018). Correlations between objective behavioral features collected from mobile and wearable devices and depressive mood symptoms in patients with affective disorders: Systematic review. Journal of Medical Internet Research mhealth uhealth, 6(8), e165. https://doi.org/10.2196/mhealth.9691
Saeb, S., Lattie, E. G., Schueller, S. M., Kording, K. P., & Mohr, D. C. (2016). The relationship between mobile phone location sensor data and depressive symptom severity. Peer Journal, 4, e2537. https://doi.org/10.7717/peerj.2537
Saeb, S., Zhang, M., Kwasny, M. M., Karr, C. J., Kording, K., & Mohr, D. C. (2015). The relationship between clinical, momentary, and sensor-based assessment of depression. International Conference on Pervasive Computing Technologies for Healthcare : [proceedings]. International Conference on Pervasive Computing Technologies for Healthcare, 2015, https://doi.org/10.4108/icst.pervasivehealth.2015.2590342015.259034
Sano, A., Phillips, A. J., Yu, A. Z., McHill, A. W., Taylor, S., Jaques, N., et al. (2015). Recognizing academic performance, sleep quality, stress level, and mental health using personality traits, wearable sensors and mobile phones. International Conference on Wearable and Implantable Body Sensor Networks. https://doi.org/10.1109/BSN.2015.72994202015.7299420
Sano, A., Taylor, S., McHill, A. W., Phillips, A. J., Barger, L. K., Klerman, E., & Picard, R. (2018). Identifying objective physiological markers and modifiable behaviors for self-reported stress and mental health status using wearable sensors and mobile phones: Observational Study. Journal of Medical Internet Research, 20(6), e210. https://doi.org/10.2196/jmir.9410
Sanchez, W., Rebollar, A. M., Campos, W., Estrada-Esquivel, H., & Pelechano, V. (2015). Inferring loneliness levels in older adults from smartphones. Journal of Ambient Intelligence & Smart Environment, 7, 85–98.
Schueller, S. M., Armstrong, C. M., & Neary, M. (2020). Identifying and using mobile apps in clinical practice article type: Special series ABCT digital intervention. Cognitive Behavioral Practice: In Press.
Seko, Y., Kidd, S., Wiljer, D., & McKenzie, K. (2014). Youth mental health interventions via mobile phones: A scoping review. Cyberpsycholology Behavioral and Social Networking, 17(9), 591–602.
Seoane, F., Mohino-Herranz, I., Ferreira, J., Alvarez, L., Buendia, R., Ayllón, D., et al. (2014). Wearable biomedical measurement systems for assessment of mental stress of combatants in real time. Sensors (Basel, Switzerland), 14(4), 7120–7141. https://doi.org/10.3390/s140407120
Seppälä, J., De Vita, I., Jämsä, T., Miettunen, J., Isohanni, M., Rubinsten, K., et al. (2019). Mobile phone and wearable sensor-based mhealth approaches for psychiatric disorders and symptoms: systematic review. Journal of Medical Internet Research Mental Health, 6(2), e9819. https://doi.org/10.2196/mental.9819
Shah, A. J., Lampert, R., Goldberg, J., Veledar, E., Bremner, J. D., & Vaccarino, V. (2013). Posttraumatic stress disorder and impaired autonomic modulation in male twins. Biological Psychiatry, 73(11), 1103–1110. https://doi.org/10.1016/j.biopsych.2013.01.0192013.01.019
Silva, B., Rodrigues, J., Diez, I., Lopez-Coronado, M., & Saleem, K. (2015). Mobile-health: a review of current state in 2015. Journal of Biomed Informatics, 56, 265–272.
Steinhubl, S. R., Muse, E. D., & Topol, E. J. (2013). Can mobile health technologies transform health care? Journal of the American Medical Association, 310(22), 2395–2396.
Sterelny, K. (2007). Social intelligence, human intelligence and niche construction. Philosophical transactions of the Royal Society of London. Series B, Biological Sciences, 362(1480), 719–730. https://doi.org/10.1098/rstb.2006.20062006.2006
Sturim, D.E., Torres-Carrasquillo, P.A., Quatieri, T.F., Malyska, N., & McCree, A. (2011). Automatic detection of depression in speech using Gaussian mixture modeling with factor analysis. INTERSPEECH. 12th Annual Conference of the International Speech Communication Association, Vols 1–5, 2992–5. https://www.isca-speech.org/archive/interspeech_2011/i11_2981.html
Stutz, T., Kowar, T., Kager, M., Tiefengrabner, M., Stuppner, M., Blechert, J., et al. (2015). Smartphone based stress prediction. In F. Ricci, K. Bontcheva, O. Conlan, & S. Lawless (Eds.), International Conference on User Modeling, Adaptation, and Personalization (pp. 240–251). Berlin: Springer-Verlag.
Swanson, L. M., Burgess, H. J., Zollars, J., & Todd Arnedt, J. (2018). An open-label pilot study of a home wearable light therapy device for postpartum depression. Archives of Women’s Mental Health, 21(5), 583–586. https://doi.org/10.1007/s00737-018-0836-z
Szydlo, T., & Konieczny, M. (2016). Mobile and wearable devices in an open and universal system for remote patient monitoring. Microprocessors and Microsystems, 46. https://doi.org/10.1016/j.micpro.2016.07.006
Tachakra, S., Wang, X. H., Istepanian, R. S., & Song, Y. H. (2003). Mobile e-health: The unwired evolution of telemedicine. Telemedicine Journal and E-Health, 9(3), 247–257.
The National Academy of Sciences, Engineering, and Medicine. (2020). Health and Medicine Division. Retrieved from: http://www.nationalacademies.org/hmd/Global/Meetings.aspx
Torous, J., & Baker, J. T. (2016). Why psychiatry needs data science and data science needs psychiatry: Connecting with technology. Journal of the American Medical Association Psychiatry, 73(1), 3–4. https://doi.org/10.1001/jamapsychiatry.2015.26222015.2622
Torous, J., & Roberts, L. W. (2017). The ethical use of mobile health technology in clinical psychiatry. Journal of Nervous and Mental Disorders, 205(1), 4–8. https://doi.org/10.1097/nmd.0000000000000596
Uphold, Nicole & Douglas, Karen & Loseke, Dannell. (2014). Effects of using an iPod app to manage recreation tasks. Career Development and Transition for Exceptional Individuals, 39. https://doi.org/10.1177/2165143414548572
Valenza, G., Nardelli, M., Lanatà, A., Gentili, C., Bertschy, G., Paradiso, R., & Scilingo, E. P. (2014). Wearable monitoring for mood recognition in bipolar disorder based on history-dependent long-term heart rate variability analysis. IEEE Journal of Biomedical and Health Informatics, 18(5), 1625–1635. https://doi.org/10.1109/JBHI.2013.22903822013.2290382
Wahle, F., Kowatsch, T., Fleisch, E., Rufer, M., & Weidt, S. (2016). Mobile sensing and support for people with depression: A pilot trial in the wild. Journal of Medical Internet Research mhealth uhealth, 4(3), e111. https://doi.org/10.2196/mhealth.5960
Wang, R., Aung, M. S. H., Abdullah, S., Brian, R., Campbell, A. T., Choudhury, T., et al., & Ben-Zeev, D. (2016). CrossCheck: Toward passive sensing and detection of mental health changes in people with schizophrenia. UbiComp 2016 - Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing, pp. 886–897.
Wang, R., Chen, F., Chen, Z., Li, T., Harari, G. M., Tignor, S., Zhou, X., Ben-Zeev, D., & Campbell, A. T. (2014). StudentLife: Assessing mental health, academic performance and behavioral trends of college students using smartphones. Proceedings of the 2014 ACM International Joint Conference on Pervasive and Ubiquitous Computing, pp. 3–14.
Wang, Q. E., Myers, M. D., & Sundaram, D. (2013). Digital natives and digital immigrants towards a model of digital fluency. Business and Information Systems Engineering, 5(6), 409–419.
Wang, Q., & Yang, Z. (2018). Does chronic disease influence susceptibility to the effects of air pollution on depressive symptoms in China? International Journal of Mental Health Systems, 12, 33. https://doi.org/10.1186/s13033-018-0212-4
Witt, D. R., Kellogg, R. A., Snyder, M. P., & Dunn, J. (2019). Windows into human health through wearables data analytics. Current Opinion in Biomedical Engineering, 9, 28–46.
Wootton, R., Liu, J., & Bonnardot, L. (2014). Assessing the quality of teleconsultations in a store-and-forward telemedicine network - Long-term monitoring taking into account differences between cases. Frontiers in Public Health, 2, 211. https://doi.org/10.3389/fpubh.2014.00211
World Health Organization. (2013). Mental Health Action Plan 2013–2020. Retrieved from: https://www.who.int/mental_health/action_plan_2013/en/2013/en/
World Health Organization. (2017). Technology report on scalable psychological interventions for people in communities affected by adversity. Retrieved from: https://www.who.int/mental_health/management/scalable_psychological_interventions/en/
Yellowlees, P., Parish, M. B., González, Á., Chan, S., Hilty, D., Iosif, A., et al. (2018). Asynchronous telepsychiatry: A component of stepped integrated care. Telemedicine Journal and E-Health, 24(5), 375–378.
Zalpuri, I., Liu, H., Stubbe, D., Wrzosek, M., Sadhu, J., & Hilty, D. (2018). A competency-based framework for social media for trainees, faculty and others. Academic Psychiatry, 42(6), 808–817. https://doi.org/10.1007/s40596-018-0983-6
Zulueta, J., Piscitello, A., Rasic, M., Easter, R., Babu, P., Langenecker, S. A., et al. (2018). Predicting mood disturbance severity with mobile phone keystroke metadata: A biaffect digital phenotyping study. Journal of Medical Internet Research, 20(7), e241. https://doi.org/10.2196/jmir.9775
Acknowledgements
American Telemedicine Association and the Telemental Health Interest Group. Department of Pschiatry and Behavioral Sciences, University of California, Davis School of Medicine. Veteran Affairs Northern California Health Care System and Mental Health Service. Office of Connected Care, Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hilty, D.M., Armstrong, C.M., Luxton, D.D. et al. A Scoping Review of Sensors, Wearables, and Remote Monitoring For Behavioral Health: Uses, Outcomes, Clinical Competencies, and Research Directions. J. technol. behav. sci. 6, 278–313 (2021). https://doi.org/10.1007/s41347-021-00199-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41347-021-00199-2