Abstract
Purpose
The purpose of this study was to evaluate and compare the effects of fixed prostheses placed on mandibles with different cortical bone thicknesses, achieved through different treatment plans, on the stress levels of the prosthesis substructures, surrounding and supporting bone tissues, and implants under masticatory forces using finite element analysis (FEA).
Methods
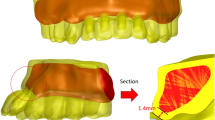
Four different implant-supported prosthesis models were designed (M1 = all-on-four, M2 = 4 vertical implants in parallel and straight configuration, M3 = trefoil, M4 = all-on-three). For each treatment plan, the cortical bone surrounding the implants was modeled with four different thicknesses. In all models, chewing forces (100 N total, 25 N per region) were applied bilaterally in the mandibular canine and second premolar regions using the foodstuff method. Von Mises stresses on the prosthesis bars and implants, as well as the minimum and maximum principal stresses in the surrounding bone, were compared using FEA.
Results
The highest stress values were observed in the M4 plan, where the cortical bone was modeled with a thickness of 0.5 mm (maximum stress value, for supporting bone: 5438 MPa; for implants: 22,783 MPa; for infrastructure material: 14,524 MPa).Increasing the cortical bone thickness in all treatment plans resulted in a decrease in stress values on the prostheses and supporting bone. When the treatment plans were evaluated based on stress values, the ranking from lowest to highest stress values was as follows M4 = all-on-three, M3 = trefoil system, M2 = 4 implants, and M1 = all-on-four system. (Minimum stress value, for supporting bone: − 0.085 MPa; for implants 3622 MPa; for infrastructure material: 5205 Mpa.
Conclusion
Cortical bone thickness is a crucial factor in preventing damaging stresses in the supporting tissues during the planning of implant-supported fixed prosthesis. The evaluation of cortical thicknesses in mandibular resorbed cases obtained comparable results to other protocols in both alfalfa and three-in-one systems. Nevertheless, the treatment plan with four implant support proved to be the most beneficial for tissue stress values. Further clinical studies are necessary on this subject within the constraints of FEA analysis.








Similar content being viewed by others
Data Availability
Data used to support the findings of this study are available from the corresponding author on request.
References
Adell, R., Lekholm, U., Rockler, B., & Brånemark, P. I. (1981). A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. International Journal of Oral Surgery, 10(6), 387–416. https://doi.org/10.1016/S0300-9785(81)80077-4
Brånemark, P. I., Engstrand, P., Öhrnell, L. O., Gröndahl, K., Nilsson, P., Hagberg, K., & Lekholm, U. (1999). Brånemark Novum®: A new treatment concept for rehabilitation of the edentulous mandible. Preliminary results from a prospective clinical follow-up study. Clinical Implant Dentistry and Related Research, 1(1), 2–16. https://doi.org/10.1111/j.1708-8208.1999.tb00086.x
Engstrand, P., Grondahl, K., Öhrnell, L. O., Nilsson, P., Nannmark, U., & Branemark, P. I. (2003). Prospective follow-up study of 95 patients with edentulous mandibles treated according to the Branemark Novum concept. Clinical Implant Dentistry and Related Research, 5(1), 3–10. https://doi.org/10.1111/j.1708-8208.2003.tb00176.x
Hatano, N., Yamaguchi, M., Yaita, T., Ishibashi, T., & Sennerby, L. (2011). New approach for immediate prosthetic rehabilitation of the edentulous mandible with three implants: A retrospective study. Clinical Oral Implants Research, 22(11), 1265–1269. https://doi.org/10.1111/j.1600-0501.2010.02101.x
Oliva, J., Oliva, X., & Oliva, J. D. (2012). All-on-three delayed implant loading concept for the completely edentulous maxilla and mandible: A retrospective 5-year follow-up study. International Journal of Oral & Maxillofacial Implants, 27(6), 1584–1592.
Maló, P., Rangert, B., & Nobre, M. (2003). “All-on-Four” immediate-function concept with Brånemark System® implants for completely edentulous mandibles: A retrospective clinical study. Clinical Implant Dentistry and Related Research, 5, 2–9. https://doi.org/10.1111/j.1708-8208.2003.tb00010.x
Bedrossian, E., & Bedrossian, E. A. (2019). Treatment planning the edentulous mandible. Review of biomechanical and clinical considerations: An update. International Journal of Oral & Maxillofacial Implants, 34(3), 33–41.
Patzelt, S. B., Bahat, O., Reynolds, M. A., & Strub, J. R. (2014). The all-on-four concept may be a viable treatment option for edentulous rehabilitation. Clinical Implant Dentistry and Related Research, 16, 836–855. https://doi.org/10.1038/sj.ebd.6401173
Horita, S., Sugiura, T., Yamamoto, K., Murakami, K., Imai, Y., & Kirita, T. (2017). Biomechanical analysis of immediately loaded implants according to the “all-on-four” concept. Journal of Prosthodontic Research, 61(2), 123–132. https://doi.org/10.1016/j.jpor.2016.08.002
Borgonovo, A. E., Galbiati, S. L., & Re, D. (2020). Trefoil system for the treatment of mandibular Edentulism: A case report with 30 months follow-up. Case Reports in Dentistry, 2020, 8845649. https://doi.org/10.1155/2020/8845649
Higuchi, K., & Liddelow, G. (2019). An innovative implant-supported treatment for the edentulous mandible: Case report. International Journal of Oral & Maxillofacial Implants, 34(2), 13–16.
Takahashi, T., Shimamura, I., & Sakurai, K. (2010). Influence of number and inclination angle of implants on stress distribution in mandibular cortical bone with all-on-4 concept. Journal of Prosthodontic Research, 54(4), 179–184. https://doi.org/10.1016/j.jpor.2010.04.004
Nobel Biocare AG. Trefoil™ Procedure manual. Retrieved July, 2023, from https://www.eotdental.com/uploads/pdf/trefoil.pdf
Ashman, R. B., & Van Buskirk, W. C. (1987). The elastic properties of a human mandible. Advances in Dental Research, 1(1), 64–67. https://doi.org/10.1177/08959374870010011401
Albrektsson, T., Brånemark, P. I., & Zarb, G. A. (Eds.). (1985). Tissue-integrated prostheses: Osseointegration in clinical dentistry. Quintessence.
Sevimay, M., Turhan, F., Kiliçarslan, M. A., & Eskitascioglu, G. (2005). Three-dimensional finite element analysis of the effect of different bone quality on stress distribution in an implant-supported crown. The Journal of Prosthetic Dentistry, 93(3), 227–234. https://doi.org/10.1016/j.prosdent.2004.12.019
Misch, C. E. (1990). Density of bone: Effect on treatment plans, surgical approach, healing, and progressive boen loading. The International Journal of Oral Implantology: Implantologist, 6(2), 23–31.
Huang, H. L., Lin, T. W., Tsai, H. L., Wu, Y. L., & Wu, A. Y. J. (2022). Biomechanical effects of bone atrophy, implant design, and vertical or tilted of posterior implant on all-on-four concept implantation: finite element analysis. Journal of Medical and Biological Engineering, 42(4), 488–497. https://doi.org/10.1007/s40846-022-00725-4
Huang, H. L., Hsu, J. T., Fuh, L. J., Tu, M. G., Ko, C. C., & Shen, Y. W. (2008). Bone stress and interfacial sliding analysis of implant designs on an immediately loaded maxillary implant: A non-linear finite element study. Journal of Dentistry, 36(6), 409–417. https://doi.org/10.1016/j.jdent.2008.02.015
Okumura, N., Stegaroiu, R., Kitamura, E., Kurokawa, K., & Nomura, S. (2010). Influence of maxillary cortical bone thickness, implant design and implant diameter on stress around implants: A three-dimensional finite element analysis. Journal of Prosthodontic Research, 54(3), 133–142. https://doi.org/10.1016/j.jpor.2009.12.004
Özdemir Doğan, D., Polat, N. T., Polat, S., Şeker, E., & Gül, E. B. (2014). Evaluation of “all-on-four” concept and alternative designs with 3D finite element analysis method. Clinical Implant Dentistry and Related Research, 16(4), 501–510. https://doi.org/10.1111/cid.12024
Tükel, H. C., & Geçkil, N. (2023). Comparison of ımplant systems applied in the mental region in the prosthetic treatment of atrophic mandible: A 3D finite element analysis. European Annals of Dental Sciences, 50(1), 35–40. https://doi.org/10.52037/eads.2023.0008
Baggi, L., Cappelloni, I., Di Girolamo, M., Maceri, F., & Vairo, G. (2008). The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: A three-dimensional finite element analysis. The Journal of prosthetic dentistry, 100(6), 422–431. https://doi.org/10.1016/S0022-3913(08)60259-0
Baggi, L., Pastore, S., Di Girolamo, M., & Vairo, G. (2013). Implant-bone load transfer mechanisms in complete-arch prostheses supported by four implants: A three-dimensional finite element approach. The Journal of Prosthetic Dentistry, 109(1), 9–21. https://doi.org/10.1016/S0022-3913(13)60004-9
Liu, T., Mu, Z., Yu, T., Wang, C., & Huang, Y. (2019). Biomechanical comparison of implant inclinations and load times with the all-on-4 treatment concept: A three-dimensional finite element analysis. Computer Methods in Biomechanics and Biomedical Engineering, 22(6), 585–594. https://doi.org/10.1080/10255842.2019.1572120
Cheng, K. C., Liu, P. H., Chen, H. S., & Lan, T. H. (2022). Stress distribution of four-unit implant-supported fixed partial prosthesis with different numbers and positions of fixtures in maxilla anterior region-3D FEA. Journal of Medical and Biological Engineering, 42(4), 526–533. https://doi.org/10.1007/s40846-022-00729-0
Nobel Biocare AG. Implants with Conical Connection Overview. Retrieved 2023, from https://www.nobelbiocare.com/en-us/catalogs
Wheeler, R. C. (1969). An atlas of tooth form (Forth edition). Saunders (W.B.) Co Ltd.
Bonnet, A. S., Postaire, M., & Lipinski, P. (2009). Biomechanical study of mandible bone supporting a four-implant retained bridge: Finite element analysis of the influence of bone anisotropy and foodstuff position. Medical Engineering & Physics, 31(7), 806–815. https://doi.org/10.1016/j.medengphy.2009.03.004
Baldwin, D. K., King, G., Ramsay, D. S., Huang, G., & Bollen, A. M. (2008). Activation time and material stiffness of sequential removable orthodontic appliances. Part 3: Premolar extraction patients. American Journal of Orthodontics and Dentofacial Orthopedics, 133(6), 837–845. https://doi.org/10.1016/j.ajodo.2006.06.025
I-Chiang, C., Shyh-Yuan, L., Ming-Chang, W., Sun, C. W., & Jiang, C. P. (2014). Finite element modelling of implant designs and cortical bone thickness on stress distribution in maxillary type IV bone. Computer Methods in Biomechanics and Biomedical Engineering, 17(5), 516–526. https://doi.org/10.1080/10255842.2012.697556
Wong, R. C., Tideman, H., Kin, L., & Merkx, M. A. (2010). Biomechanics of mandibular reconstruction: A review. International Journal of Oral and Maxillofacial Surgery, 39(4), 313–319.
Balshi, T. J., Wolfinger, G. J., Balshi, S. F., & Bidra, A. S. (2019). A 30-year follow-up of a patient with mandibular complete-arch fixed implant-supported prosthesis on 4 implants: A clinical report. Journal of Prosthodontics, 28(2), 97–102. https://doi.org/10.1016/j.ijom.2009.11.003
Misch, C. E., Qu, Z., & Bidez, M. W. (1999). Mechanical properties of trabecular bone in the human mandible: Implications for dental implant treatment planning and surgical placement. Journal of Oral and Maxillofacial Surgery, 57(6), 700–706.
Elsayyad, A. A., Abbas, N. A., AbdelNabi, N. M., & Osman, R. B. (2020). Biomechanics of 3-implant-supported and 4-implant-supported mandibular screw-retained prostheses: A 3D finite element analysis study. The Journal of Prosthetic Dentistry, 124(1), 68-e1. https://doi.org/10.1016/s0278-2391(99)90437-8
Hatano, N., Yamaguchi, M., Suwa, T., & Watanabe, K. (2003). A modified method of immediate loading using Brånemark implants in edentulous mandibles. Odontology, 91(1), 37–42. https://doi.org/10.1007/s10266-003-0027-9
Murugaian, J., Ganesan, L., Shankar, M. S., & Annapoorni, H. (2022). A comparative evaluation of stress distribution between an all-on-four implant-supported prosthesis and the Trefoil implant-supported prosthesis: A three-dimensional finite element analysis study. The Journal of the Indian Prosthodontic Society, 22(1), 56–64. https://doi.org/10.4103/jips.jips_203_21
Sousa, R. M., Simamoto-Junior, P. C., Fernandes-Neto, A. J., Sloten, J. V., Jaecques, S. V., & Pessoa, R. S. (2016). Influence of connection types and ımplant number on the biomechanical behavior of mandibular full-arch rehabilitation. The International Journal of Oral & Maxillofacial Implants, 31(4), 750–760. https://doi.org/10.11607/jomi.4785
Bassi-Junior, L., de Souza Silva, R. O., Dos Santos, V. H. D., da Rocha Lourenço, A., Trevizoli, P. V., Gaêta-Araujo, H., & Gottardo, V. D. (2021). Mechanical analysis of prosthetic bars and dental implants in 3 and 4 implant-supported overdenture protocols using finite element analysis. Journal of Oral Biology and Craniofacial Research, 11(3), 438–441. https://doi.org/10.1016/j.jobcr.2021.05.007
Branemark, P. I. (1977). Osseointegrated implants in the treatment of the edentulous jaw: Experience from a 10-year period. Scandinavian Journal of Plastic and Reconstructive Surgery, 16, 1–132.
Krennmair, G., Seemann, R., Weinländer, M., Krennmair, S., & Piehslinger, E. (2013). Clinical outcome and peri-implant findings of four-implant-supported distal cantilevered fixed mandibular prostheses: Five-year results. International Journal of Oral & Maxillofacial Implants, 28(3), 831–840. https://doi.org/10.11607/jomi.3024
Maló, P., de Araújo Nobre, M., & Lopes, A. (2013). The prognosis of partial implant-supported fixed dental prostheses with cantilevers. A 5-year retrospective cohort study. European Journal of Oral Implantology, 6(1), 51–59. https://doi.org/10.1016/j.jpor.2019.02.001
Correa, S., Ivancik, J., Isaza, J. F., & Naranjo, M. (2012). Evaluation of the structural behavior of three and four implant-supported fixed prosthetic restorations by finite element analysis. Journal of Prosthodontic Research, 56(2), 110–119. https://doi.org/10.1016/j.jpor.2011.07.001
Bellini, C. M., Romeo, D., Galbusera, F., Taschieri, S., Raimondi, M. T., Zampelis, A., & Francetti, L. (2009). Comparison of tilted versus nontilted implant-supported prosthetic designs for the restoration of the edentuous mandible: A biomechanical study. International Journal of Oral & Maxillofacial Implants, 24(3), 511–517. https://doi.org/10.1299/jbse.5.526
Rubo, J. H., & Capello Souza, E. A. (2010). Finite-element analysis of stress on dental implant prosthesis. Clinical Implant Dentistry and Related Research, 12(2), 105–113. https://doi.org/10.5577/intdentres.2021.vol11.suppl1.27
Torrecillas-Martínez, L., Monje, A., Lin, G. H., Suarez, F., Ortega-Oller, I., Galindo-Moreno, P., & Wang, H. L. (2014). Effect of cantilevers for implant-supported prostheses on marginal bone loss and prosthetic complications: Systematic review and meta-analysis. International Journal of Oral & Maxillofacial Implants, 29(6), 1315–1321. https://doi.org/10.11607/jomi.3660
Begg, T., Geerts, G. A. V. M., & Gryzagoridis, J. (2009). Stress patterns around distal angled implants in the all-on-four concept configuration. International Journal of Oral & Maxillofacial Implants, 24, 663–671.
Naini, R. B., Nokar, S., Borghei, H., & Alikhasi, M. (2011). Tilted or parallel implant placement in the completely edentulous mandible? A three-dimensional finite element analysis. International Journal of Oral & Maxillofacial Implants, 26(4), 776–781.
Zampelis, A., Rangert, B., & Heijl, L. (2007). Tilting of splinted implants for improved prosthodontic support: A two-dimensional finite element analysis. The Journal of Prosthetic Dentistry, 97(6), 35–43. https://doi.org/10.1016/S0022-3913(07)60006-7
Weinstein, A. M., Klawitter, J. J., Anand, S. C., & Schuessler, R. (1976). Stress analysis of porous rooted dental implants. Journal of Dental Research, 55(5), 772–777. https://doi.org/10.1177/00220345760550051001
Karl, M., & Taylor, T. D. (2016). Bone adaptation ınduced by non-passively fitting ımplant superstructures: A randomized clinical trial. International Journal of Oral & Maxillofacial Implants, 31(2), 369–375. https://doi.org/10.11607/jomi.4331
Sakaguchi, R. L., & Powers, J. M. (2011). Craig’s restorative dental materials-e-book. Elsevier Health Sciences.
Aydin, C., Özen, J., Yilmaz, C., & Korkmaz, T. (2006). Effects of mesiodistal inclination of implants on stress distribution in implant-supported fixed prostheses. International Journal of Oral & Maxillofacial Implants, 21(1), 36–44.
Tseng, B. T., Yen, Y. C., Cheng, C. S., Wang, C. H., Lien, K. H., Huang, C. M., & Su, K. C. (2022). Biomechanical effects of different miniplate thicknesses and fixation methods applied in BSSO surgery under two occlusal conditions. Journal of Medical and Biological Engineering, 42(4), 445–458. https://doi.org/10.1007/s40846-022-00733-4
Liu, J., Pan, S., Dong, J., Mo, Z., Fan, Y., & Feng, H. (2013). Influence of implant number on the biomechanical behaviour of mandibular implant-retained/supported overdentures: A three-dimensional finite element analysis. Journal of Dentistry, 41(3), 241–249. https://doi.org/10.1016/j.jdent.2012.11.008
Acknowledgements
Thanks to Başak Kızıltan Eliçık for her contribution to the publication.
Funding
This research was financial support by 2022/071 number of scientific research projects of the University of Health Sciences.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by EGS, ET, ZBÖ and AÇŞ. The first draft of the manuscript was written by EGS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
No conflicts of interest in this study.
Ethical Approval
No human or animal data were used in this study. All study was done in computer environment. Ethical approval is not required.
Consent to Participate
Not required.
Consent to Publish
Not required.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Güzelce Sultanoğlu, E., Özsağir, Z.B., Çiftçi Şişman, A. et al. Evaluation of the Effect of Cortical Bone Thickness on Stress Distribution in Implant-Supported Fixed Prostheses. J. Med. Biol. Eng. 43, 633–647 (2023). https://doi.org/10.1007/s40846-023-00830-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-023-00830-y