Abstract
Introduction
The impact of coronavirus disease 2019 (COVID-19) on vulnerable populations with autoimmune inflammatory rheumatic diseases (AIIRDs) has been variable with variants and of great concern. Here we report the clinical features, outcomes, and risk factors for infection and hospitalization in patients with AIIRDs in the first wave of infection in China in December 2022.
Methods
A real-world survey was conducted in Chinese patients with AIIRDs from 8 December 2022 to 13 January 2023. The survey was distributed via internet nationwide, clinic consultation, and to inpatients at a tertiary hospital in Beijing. Clinical features, outcomes, and vaccination status were collected.
Results
A total of 2005 patients with AIIRDs completed the survey. There were 1690 (84.3%) patients infected and only 48.2% of patients received COVID-19 vaccination. Most of the fully vaccinated patients received inactivated COVID-19 vaccines, including Sinovac (55.6%) and Sinopharm (27.2%), followed by recombinant subunit vaccine from Zhifei Longcom (2.0%). The independent protecting factors for infection were a time interval of less than 3 months from last vaccination (OR 0.53, p = 0.037) and rheumatoid arthritis (RA) as the underlying AIIRD (OR 0.62, p = 0.041). A total of 57 out of 1690 patients (3.4%) were hospitalized for COVID, with 46 (2.7%) experiencing severe/critical course and 6 deaths (0.4%). In multivariable logistic regression analysis, independent risk factors for hospitalization were age over 60 years (OR 11.52, p < 0.001), with comorbidity (OR 1.83, p = 0.045) and systemic lupus erythematosus (SLE) as the AIIRDs (OR 2.59, p = 0.036). Receiving booster vaccine was an independent protective factor for hospitalization (OR 0.53, 95% CI 0.30–0.98; p = 0.018).
Conclusion
Hesitation for vaccination is common among Chinese patients with AIIRDs. The time from last vaccination of less than 3 months and having RA decreased the risk of COVID infection. Older age and having comorbidity or SLE increased the risk of hospitalization, while booster vaccination reduced the risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The impact of coronavirus disease 2019 (COVID-19) on vulnerable populations with autoimmune inflammatory rheumatic diseases (AIIRDs) has been variable with variants and of great concern. |
The Omicron pandemic in China several months ago was the first big wave and aroused great worry globally. |
This study reports on the clinical characteristics and outcomes of COVID-19 in Chinese patients with AIIRDs in this big wave of infection. |
What was learned from the study? |
Hesitation for vaccination is common among patients with AIIRDs. |
The time from last vaccination of less than 3 months decreased COVID-19 infection risk. |
Booster vaccination reduced hospitalization risk among patients with AIIRDs. |
Introduction
The coronavirus disease 2019 (COVID-19) pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) poses an ongoing challenge for public health worldwide [1, 2]. The prevention and control of COVID-19 in vulnerable populations with autoimmune inflammatory rheumatic diseases (AIIRDs) has brought extraordinary challenges [3, 4]. A meta-analysis of global data showed that patients with AIIRDs are more susceptible to SARS-CoV-2 infection and have more severe disease with poorer outcomes [5]. Nevertheless, the use of glucocorticoids and interleukin-6 (IL-6) receptor inhibitor has been shown to be associated with lower risk for developing severe acute respiratory distress syndrome (ARDS) [6, 7]. On the other hand, vaccination has been shown to be effective in controlling the global COVID pandemic and reducing severe cases, and therefore has been strongly recommended for patients with AIIRDs in all the guidance worldwide [8, 9]. Nevertheless, immunosuppressive treatments often hamper vaccine immunogenicity [10, 11]. Preliminary data show that breakthrough COVID-19 may occur in vaccinated patients with AIIRDs, occasionally leading to hospitalization and death [12, 13]. The clinical study on COVID in vaccinated patients with AIIRDs is limited so far.
There have been few COVID cases in China under the strict quarantine and control policy since the outbreak of infection in December 2019. The sudden and full release of control on 8 December 2022 followed an outburst of infection in the past month, which has aroused great attention globally. The rate of infection, clinical features, and outcomes of infected populations have not been disclosed. Here we most report these data based on a real-world survey in the patients with AIIRDs. The risk factors for infection and hospitalization were also analyzed in the study.
Methods
Study Population and Data Collection
Participants with definite AIIRDs were invited to complete an electronic nationwide survey by social media or printed questionnaire in Peking University First Hospital outpatient and inpatient department from 8 December 2022 to 13 January 2023.
Data were recorded by using a structured questionnaire with the following components: (1) Demographics (age, gender), telephone number, allergic history, comorbidities (cardiovascular disease, cerebrovascular disease, diabetes, hypertension, cancer, severe liver disease, chronic lung disease); (2) AIIRDs-related characteristics, including type and duration of disease, self-reported disease activity, and immunosuppressive/immunomodulatory treatment regimens before getting COVID; (3) COVID vaccine-related details, including vaccination status, number of shots, vaccinated time, side effects; (4) Characteristics of COVID, including manifestations, duration of symptoms, and coping styles which were classified as self-quarantined at home, emergency room visit, hospitalization, and death. For any information in the questionnaire that was unclear or uncertain, we contacted the patient via telephone to confirm it.
Patient approval was obtained before patients completed the survey. The ethics committee of Peking University First Hospital waived approval for this study as it was a retrospective internet-based survey.
Study Outcomes
Infection and hospitalization due to COVID-19 were taken as the main outcomes of the study. The severity of COVID was classified as asymptomatic, mild, moderate, and severe/critical.
Statistics
R software (Version 4.13) was used to for the data analysis. A Kolmogorov–Smirnov test of normality was performed for all variables. Quantitative data are presented as mean ± standard deviation (SD) if the data were normally distributed or expressed as median and interquartile range (IQR) if the data did not follow Gaussian distributions. Categorical variables were described as percentages. In addition, quantitative data were analyzed using independent Student’s t test (for parametric data) or Mann–Whitney U test (for nonparametric data). Categorical data were compared using chi-squared test and Fisher’s exact test. Factors associated with SARS-CoV-2 infection or hospitalization were analyzed by univariate and multivariate logistical regressions. For all statistical analyses, two-tailed p < 0.05 was considered as being statistically significant.
Results
Clinical Characteristics of Patients with AIIRDs and with Infection and Without
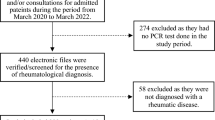
The flow diagram of this study is shown in Fig. 1. A total of 2005 patients with AIIRDs completed the survey and were included in the cross-sectional study between 8 December 2022 and 13 January 2023. The median age was 39 (IQR 31–51) years and most of them were women (n = 1579, 78.8%). The types of AIIRDs of participants in the survey were systemic lupus erythematosus (SLE) (1039, 51.8%), rheumatoid arthritis (RA) (290, 14.5%), Behcet’s disease (BD) (231, 11.5%), psoriasis/psoriatic arthritis (58, 2.9%), ankylosing spondylitis (58, 2.9%), primary Sjögren’s syndrome (55, 2.7%), and others (including ANCA-associated vasculitis, inflammatory myositis, mixed connective tissue disease, systemic sclerosis, etc.) (Fig. 2). The median duration of AIIRDs was 6 (IQR 3–12) years. There were 679 (33.9%) patients with a history of comorbidities, e.g., hypertension (225, 11.2%), chronic lung disease (88, 4.4%), diabetes mellitus (76, 3.8%), cardiovascular diseases (54, 2.7%), cerebrovascular diseases (33, 1.6%), cancer (37, 1.8%), etc. For medications when they experienced infection, glucocorticoids were taken by 1200 (59.9%) patients, hydroxychloroquine (HCQ) by 1021 (50.9%) patients, methotrexate by 315 (15.7%) patients, and JAK inhibitors/biologics by 397 (19.8%) patients. Most patients (n = 1727, 86.1%) self-reported that their AIIRDs were stable before getting COVID.
Among the patients, 1690 (84.3%) were infected (infected group hereafter) and 315 (15.7%) were not infected (non-infected group hereafter). The clinical characteristics of patients in these two group are shown in Table 1. The non-infected patients were older with longer disease duration compared with the infected group [40 (IQR 32–56) vs. 39 (IQR 31–50), p = 0.031; 7 (IQR 3–13) vs. 6 (IQR 3–11), p = 0.021].
In the infected group, there were 880 (52.1%) patients with SLE, 228 (13.5%) with RA, 196 (11.6%) with BD, and 50 (3.0%) with pSS, yielding the corresponding infection rates of 84.7%, 78.6%, 84.8%, and 90.9%, respectively. Interestingly, a lower rate of infection was observed in patients with RA than that in patients with other AIIRDs categories (78.6% vs 85.2%, p = 0.004). Moreover, there was a borderline higher rate of HCQ use in the infected group as compared to the non-infected group (51.9% vs. 45.7%, p = 0.044).
Regarding vaccination for COVID, 966 out of 2005 (48.2%) patients received at least one-dose vaccine, with one shot in 66 (3.3%), two shots in 286 (14.3%), and three shots in 614 (30.6%) patients. Most of the fully vaccinated patients received inactivated COVID-19 vaccines, including Sinovac (55.6%) and Sinopharm (27.2%), followed by recombinant subunit vaccine from Zhifei Longcom (2.0%). The proportion of patients having at least one-dose vaccine was higher in the infected group than in the non-infected group (49.2% vs. 42.9%, p = 0.039). The time interval from the last vaccine shot to the questionnaire survey was generally long [12.8 (8.5, 14.9) months], and very close between the non-infected group and the infected group [12.5 (7.48, 14.5) vs. 13.0 (8.5, 15.0) months, p = 0.171]. Nevertheless, the proportion of patients with time interval of less than 3 months from last vaccination was higher in the non-infected group than in the infected group (7.0% vs. 4.3%, p = 0.016).
Risk Factors for COVID in Patients with AIIRDs
In univariable analysis, age older than 60 years, having two doses of vaccine, disease category as RA, and HCQ use were identified as factors associated with COVID infection in patients with AIIRDs. The multivariable logistic regression analysis showed that a time interval of less than 3 months from last vaccination (OR 0.43, 95% CI 0.21–0.88, p = 0.020) and having RA as the underlying AIIRD (OR 0.61, 95% CI 0.39–0.96, p = 0.035) were independent protective factors for infection. The exposure to either glucocorticoids or any immunosuppressants was not significantly associated with COVID infection in the univariate model (Table 2).
Outcomes and Clinical Features of COVID in Patients with AIIRDs
Among 1690 infected patients, 1577 (93.3%) were symptomatic. Fever and cough were reported as the predominant symptoms, in 77.2% and 75.1% of patients, respectively. Headache, sore throat, nasal congestion, myalgias, and fatigue were also common, being reported in 41.7–53.4% of patients. Furthmore, 22.5–30.6% patients reported shortness of breath, loss of taste/smell, and vomiting/diarrhea (Table 3).
As for severity of COVID, 1531 (90.6%) patients showed mild/moderate symptomatology, 46 (2.7%) patients developed severe/critical course, and 113 (6.7%) were asymptomatic. The majority of infected patients self-quarantined at home. In fact, 1595 (94.4%) patients stayed at home, in the manuscript, 57(3.4%) patients were hospitalized (including 6 deaths) as a result of COVID-19. The 51 (3.0%) hospitalization in Table 3 do not include 6 death. There were 6 deaths (0.4%), 4 with SLE and 2 with ANCA-associated vasculitis.
Risk Factors for Hospitalization due to COVID in Patients with AIIRDs
The clinical characteristics of patients with AIIRDs and COVID stratified by hospitalization status is shown in Table 4. Fifty-seven out of 1690 patients (3.4%) were hospitalized, 36 with SLE (63.2%), 5 with BD (8.8%), and 4 with RA (7.0%). The rates of hospitalization in patients with SLE, BD, and RA were 4.1%, 2.6%, and 1.8%, respectively. The rate of hospitalization seemed to be higher in patients with SLE than in patients with other AIIRDs categories (4.1% vs 2.6%, p = 0.088), although the difference was statistically insignificant. These inpatients were older [54 (39, 67) vs. 38 (31, 49), p < 0.001] and more likely to have comorbidities (59.6% vs. 32.2%, p < 0.001) and self-report active AIIRDs status (22.8% vs. 13.4%, p = 0.043) as compared with those who self-quarantined at home. Additionally, significantly higher proportions of hospitalized patients were taking glucocorticoid and cyclophosphamide compared with non-hospitalized patients (75.4% vs. 59.8%, p = 0.018; 7.0% vs. 2.1%, p = 0.013). The proportion of patients having at least one-dose vaccine and patients who were receiving booster vaccine was higher in non-hospitalized patients than hospitalized patients (50.0% vs. 24.6%, p < 0.001; 31.5% vs. 14.0%, p = 0.005).
The results of univariable and multivariable logistic regression analysis for hospitalization among patients with AIIRDs and COVID are shown in Table 5. Age older than 60 years (OR 11.52, CI 4.18–34.18; p < 0.001), previous history of comorbidity (OR 1.83, CI 1.02–3.32; p = 0.045), and having SLE as the underlying AIIRD (OR 2.59, CI 1.08–6.39; p = 0.036) were independently associated with increased risk of hospitalization due to COVID. Booster vaccination was an independent protective factor for hospitalization (OR 0.34; 95% CI 0.13–0.74; p = 0.011). Other factors such as disease activity status or immunosuppressive drugs for AIIRDs were not identified in the logistic analysis.
Discussion
This is the first report on the clinical characteristics and outcomes of COVID in Chinese patients with AIIRDs in the big wave of infection in December 2022. This was also a large questionnaire survey with over 2000 participants with AIIRDs. We showed that among study participants, 84.3% of Chinese patients with AIIRDs had been infected by 13 January 2023. The rates of infection, hospitalization, and fatality were 84.3%, 3.4%, and 0.4%, respectively.
Patients with AIIRDs are believed to be more susceptible to pathogens because of the impairment of their immune system. The prevention and early identification of severe COVID cases in AIIRDs populations are extremely important. Vaccination has been an important way of reducing SARS-CoV-2 infection as well preventing severe disease. Danza et al. indicated that the incidence of COVID in the general population was the highest in unvaccinated persons and lowest among fully vaccinated persons with a booster during Omicron variant predominance [14]. But the poor immunogenicity in the immunocompromised population always threatens the effectiveness of the vaccine [15]. In this study, we found that a time interval of less than 3 months from last vaccination was an independent protective factor for infection in patients with AIIRDs, which may be correlated with the high titre of vaccine-induced antibody.
Several studies have proved the effect of vaccination in reducing severe cases. Our data also showed that booster vaccination was an independent protective factor for hospitalization due to COVID. Papagoras et al. found that the rates of hospitalization and mortality were higher in the unvaccinated group than partially vaccinated or fully vaccinated groups in patients with AIIRDs [12]. Widdifield et al. reported that two doses of vaccine was highly protective against both SARS-CoV-2 infection and poor outcomes in patients with immune-mediated inflammatory diseases [16]. Bakasis et al. revealed a significant inverse association of three-dose vaccination with severe/critical COVID in patients with AIIRDs [17]. Besides, our previous studies on inactivated COVID-19 vaccine in patients with AIIRDs have shown not only safety but also no impact on disease activity or increase in the risk of flare when their AIIRDs were stable [18, 19]. Taking all these pieces of evidence together, one should encourage patients with AIIRDs to receive vaccination, especially booster vaccination, to reduce the risk in the following waves of the COVID pandemic.
Additionally, our survey showed that patients with RA were less likely to have COVID and patients with SLE tended to have more severe COVID compared to other types of AIIRDs. These phenomena may be explained by relatively milder impairment of the immune system in RA compared to SLE, relating to both the disease itself and medications used [20]. Favalli et al. reported higher risk for infection in patients with RA than the general population [21]. Since the corresponding data of the COVID outbreak in December 2022 among the general Chinese population have not been released yet, we are not able to evaluate the risk of infection among patients with AIIRDs compared to the general population. But this will be answered when the data are available.
Among 3.4% hospitalized patients, we found that age over 60 years and a history of comorbidities are risk factors for hospitalization, which was in line with previous reports. Older age has been recognized as the most significant factor associated with severe COVID both in the general population and in patients with AIIRDs because of their poor immune defensive capability [22, 23]. It has also been confirmed that presence of comorbidity significantly contributes to the increased risk of hospitalization and poor outcomes for patients with COVID [23]. Moreover, the probability of hospitalization was also related to the type of AIIRD. Patients with systemic autoimmune diseases are more likely to have severe COVID compared to those with inflammatory arthritis [24]. Another study also showed the more significant association of severe COVID with having a connective tissue disease than inflammatory arthritis [25]. Mehta et al. demonstrated that patients with SLE have a greater risk of COVID-related hospitalization, severe disease, and death than the general population [26]. Our results again supported the findings.
It seemed that the patients exposed to glucocorticoid or immunosuppressants were not at higher risk of hospitalization due to COVID, probably owing to anti-inflammatory effect of these drugs and the complicated regimens used in these patients. Further study is needed to stratify the dosage and length of glucocorticoid or immunosuppressant treatment for AIIRDs to confirm the association or not.
This report shows the clinical manifestations and outcomes of patients with AIIRDs during the Omicron pandemic in China in December 2022. The survey in over 2000 participants provided a real-world picture of COVID among patients with AIIRDs. We are aware of some limitations. First, some selection bias may exist. For instance, many patients with lupus responded, but some patients with severe COVID and AIIRDs might not have been able to respond to the survey. Second, use of antiviral medications was not included in the survey because most of these medications were unavailable at the time of designing the questionnaire. But in fact, very few patients with COVID ever used antiviral drugs during the pandemic in December 2022. Third, we are not able to conclude the risk and severity of COVID infection in patients with AIIRDs compared to the general population because of the unavailability of data in the general population.
Conclusions
The time from last vaccination of less than 3 months and having RA decreased the risk of COVID infection. Older age and having comorbidity or SLE as underlying AIIRD increased the risk for hospitalization, while booster vaccination reduced the risk in patients with AIIRDs. These results provide evidence for recommending management for patients with AIIRDs in the following waves of the COVID pandemic.
References
Fernandez-Gutierrez B. COVID-19 with pulmonary involvement. An autoimmune disease of known cause. Reumatol Clin (Engl Ed). 2020;16(4):253–4.
Gates B. Responding to Covid-19—a once-in-a-century pandemic? N Engl J Med. 2020;382(18):1677–9.
Figueroa-Parra G, Aguirre-Garcia GM, Gamboa-Alonso CM, Camacho-Ortiz A, Galarza-Delgado DA. Are my patients with rheumatic diseases at higher risk of COVID-19? Ann Rheum Dis. 2020;79(6):839–40.
Ehrenfeld M, Tincani A, Andreoli L, et al. Covid-19 and autoimmunity. Autoimmun Rev. 2020;19(8):102597.
Xu C, Yi Z, Cai R, Chen R, Thong BY, Mu R. Clinical outcomes of COVID-19 in patients with rheumatic diseases: a systematic review and meta-analysis of global data. Autoimmun Rev. 2021;20(4):102778.
Shang L, Zhao J, Hu Y, Du R, Cao B. On the use of corticosteroids for 2019-nCoV pneumonia. Lancet (London, England). 2020;395(10225):683–4.
Toniati P, Piva S, Cattalini M, et al. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: a single center study of 100 patients in Brescia, Italy. Autoimmun Rev. 2020;19(7):102568.
Bijlsma JW, Force EC-T. EULAR 2021 updated viewpoints on SARS-CoV-2 vaccination in patients with RMDs: a guidance to answer patients’ questions. Ann Rheum Dis. 2022;81(6):786–8.
Curtis JR, Johnson SR, Anthony DD, et al. American College of Rheumatology Guidance for COVID-19 vaccination in patients with rheumatic and musculoskeletal diseases: version 5. Arthritis Rheumatol. 2023;75(1):e1–16.
Furer V, Eviatar T, Zisman D, et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: a multicentre study. Ann Rheum Dis. 2021;80(10):1330–8.
Kim WJ, Choi SH, Park JY, Song JS, Chung JW, Choi ST. SARS-CoV-2 Omicron escapes mRNA vaccine booster-induced antibody neutralisation in patients with autoimmune rheumatic diseases: an observational cohort study. Ann Rheum Dis. 2022;81(11):1585–93.
Papagoras C, Fragoulis GE, Zioga N, et al. Better outcomes of COVID-19 in vaccinated compared to unvaccinated patients with systemic rheumatic diseases. Ann Rheum Dis. 2022;81(7):1013–6.
Singson JRC, Kirley PD, Pham H, et al. Factors associated with severe outcomes among immunocompromised adults hospitalized for COVID-19-COVID-NET, 10 states, March 2020-February 2022. MMWR Morb Mortal Wkly Rep. 2022;71(27):878–84.
Danza P, Koo TH, Haddix M, et al. SARS-CoV-2 infection and hospitalization among adults aged >/=18 years, by vaccination status, before and during SARS-CoV-2 B.1.1.529 (Omicron) variant predominance-Los Angeles County, California, November 7, 2021-January 8, 2022. MMWR Morb Mortal Wkly Rep. 2022;71(5):177–81.
Liew J, Gianfrancesco M, Harrison C, et al. SARS-CoV-2 breakthrough infections among vaccinated individuals with rheumatic disease: results from the COVID-19 Global Rheumatology Alliance provider registry. RMD Open. 2022;8(1):e002187.
Widdifield J, Kwong JC, Chen S, et al. Vaccine effectiveness against SARS-CoV-2 infection and severe outcomes among individuals with immune-mediated inflammatory diseases tested between March 1 and Nov 22, 2021, in Ontario, Canada: a population-based analysis. Lancet Rheumatol. 2022;4(6):e430–40.
Bakasis AD, Mavragani CP, Voulgari PV, et al. COVID-19: Clinical features and outcomes in unvaccinated 2-dose and 3-dose vaccinated against SARS-CoV-2 patients with systemic autoimmune and autoinflammatory rheumatic diseases. J Autoimmun. 2022;131: 102846.
Fan Y, Geng Y, Wang Y, et al. Safety and disease flare of autoimmune inflammatory rheumatic diseases: a large real-world survey on inactivated COVID-19 vaccines. Ann Rheum Dis. 2022;81(3):443–5.
Geng Y, Fan Y, Wang Y, et al. Flare and change in disease activity among patients with stable rheumatoid arthritis following coronavirus disease 2019 vaccination: a prospective Chinese cohort study. Chin Med J (Engl). 2023 Mar 15. https://doi.org/10.1097/CM9.0000000000002562.
Fagni F, Simon D, Tascilar K, et al. COVID-19 and immune-mediated inflammatory diseases: effect of disease and treatment on COVID-19 outcomes and vaccine responses. Lancet Rheumatol. 2021;3(10):e724–36.
Favalli EG, Ingegnoli F, De Lucia O, Cincinelli G, Cimaz R, Caporali R. COVID-19 infection and rheumatoid arthritis: faraway, so close! Autoimmun Rev. 2020;19(5):102523.
Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020;81(2):e16–25.
Wang Q, Liu J, Shao R, Han X, Su C, Lu W. Risk and clinical outcomes of COVID-19 in patients with rheumatic diseases compared with the general population: a systematic review and meta-analysis. Rheumatol Int. 2021;41(5):851–61.
Freites Nunez DD, Leon L, Mucientes A, et al. Risk factors for hospital admissions related to COVID-19 in patients with autoimmune inflammatory rheumatic diseases. Ann Rheum Dis. 2020;79(11):1393–9.
Pablos JL, Galindo M, Carmona L, et al. Clinical outcomes of hospitalised patients with COVID-19 and chronic inflammatory and autoimmune rheumatic diseases: a multicentric matched cohort study. Ann Rheum Dis. 2020;79(12):1544–9.
Mehta P, Gasparyan AY, Zimba O, Kitas GD. Systemic lupus erythematosus in the light of the COVID-19 pandemic: infection, vaccination, and impact on disease management. Clin Rheumatol. 2022;41(9):2893–910.
Acknowledgements
The authors would like to thank all the staff and patients who participated in this study, especially the Chinese Alliance of Behcet’s disease, and MiJian Lupus Management Platform.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81771740, 81901646, 82000060), Peking University Medicine Seed Fund for Interdisciplinary Research supported by the Fundamental Research Funds for the Central Universities (BMU2022MX003) and Interdisciplinary clinical research project of Peking University First Hospital (2021CR30). No funding was received for publication of this article, the journal’s Rapid Service Fee was funded by the authors.
Author Contributions
Zhuoli Zhang contributed to study design and critically revised the manuscript. Yan Geng and Yong Fan had full access to all the data collection, analysis, interpretation, and drafted the manuscript. Xuerong Deng, Yu Wang, Juan Zhao, Lanlan Ji, Zhibo Song, Guangtao Li, Xiaohui Zhang, Xiaoying Sun, Hong Huang and Wenhui Xie contributed to the survey and questionnaire collection. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work, and have provided their approval for this version to be published.
Disclosures
Yan Geng, Yong Fan, Xuerong Deng, Yu Wang, Juan Zhao, Lanlan Ji, Zhibo Song, Guangtao Li, Xiaohui Zhang, Xiaoying Sun, Hong Huang, Wenhui Xie and Zhuoli Zhang declare that they have no conflict of interest.
Compliance with Ethics Guidelines
The ethics committee of Peking University First Hospital waived approval for this study as it was a retrospective internet-based survey. Patient approval was obtained before they completed the survey.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Geng, Y., Fan, Y., Deng, X. et al. The Recent Outbreak of COVID-19 in China During the Omicron Variant Predominance: Clinical Features and Outcomes in Patients with Autoimmune Inflammatory Rheumatic Diseases. Rheumatol Ther 10, 1039–1053 (2023). https://doi.org/10.1007/s40744-023-00569-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-023-00569-7