Abstract
Introduction
Sustained improvement of high degree in clinical outcomes have been demonstrated in phase 3 trials with secukinumab in both psoriatic arthritis (PsA) and ankylosing spondylitis (AS). The objective of the SERENA study was to evaluate the effectiveness, retention rates, and safety of secukinumab in patients with PsA and AS.
Methods
SERENA is an ongoing, longitudinal, real-world observational study involving patients with moderate-to-severe psoriasis, PsA, or AS. Patients had received at least 16 weeks of secukinumab treatment before recruitment to the study. Retention rate was defined as percentage of patients who continued secukinumab treatment over the course of study. Effectiveness of secukinumab in AS and PsA cohorts was assessed using descriptive statistics.
Results
The current interim analysis included 1004 patients with PsA or AS. Overall secukinumab retention rates at 2 years after enrolment were 74.9 and 78.9% in patients with PsA and AS, respectively. At baseline and at 2 years, swollen joint count [3.3 (5.8) vs. 2.9 (5.8)], tender joint count [6.3 (9.4) vs. 5.6 (7.2)] in patients with PsA and BASDAI scores [3.2 (2.3) vs. 2.9 (2.3)] in patients with AS, suggest sustained effectiveness for patients remaining on secukinumab for at least 2 years after enrolment. A total of 73 patients had treatment interruption; 78% of these patients reinitiated secukinumab without a loading dose. No new or unexpected safety signals were reported.
Conclusions
After more than 2 years since initiation, secukinumab demonstrated high retention rates and favorable safety profile as well as sustained effectiveness in patients who continued secukinumab treatment.
Similar content being viewed by others
Why carry out this study? |
Clinical trials have demonstrated a sustained efficacy and consistent safety profile of secukinumab in patients with psoriatic arthritis (PsA) and ankylosing spondylitis (AS). |
However, there is limited real-world evidence data reporting the long-term retention of secukinumab in patients with PsA and AS. |
What was learned from the study? |
High treatment retention rates of ~ 75% in patients with PsA and AS were shown for secukinumab after 2 years of enrollment in the study, consistent with those observed in phase III clinical trials of secukinumab. |
The study demonstrated that nearly two-thirds of the patients included in study were previously exposed to biologic therapy and nearly 90% of them had discontinued previous therapies due to lack of efficacy. The study demonstrated sustained effectiveness for patients who had interrupted treatment and a favorable safety profile following more than 2 years of secukinumab therapy. |
Treatment decision-making is guided not only by efficacy outcomes in the randomized controlled setting but also by long-term, real-world treatment outcomes. The 2-year data across different domains of PsA and AS further corroborates the long-term effectiveness, high retention rate, and favorable safety profile of secukinumab therapy in a real-world setting. |
Introduction
Psoriatic arthritis (PsA) and ankylosing spondylitis (AS) are chronic, immune-mediated disorders within the spectrum of spondyloarthritis (SpA) [1, 2]. The global prevalence of SpA ranges from ~ 0.20 to 1.61% with comparable rates in AS (0.02–0.35%) [3] and PsA (0.01–1%) patients [4]. There is considerable variation in the reported prevalence of SpA across geographical regions with < 0.9% in Asia and Middle Eastern countries and a range of 0.3–1.9% in the European countries [5].
The pathogenesis of AS and PsA is multifactorial with a complex interaction of genetic predisposition, environmental triggers, and immunological factors subsequently leading to immune system dysregulation [6,7,8]. Both PsA and AS are interrelated disorders with various shared clinical, genetic, and immunologic features [1, 8].
Psoriatic arthritis exhibits variability in disease activity and clinical presentation and is characterized by articular and extra-articular manifestations including peripheral arthritis, axial involvement, enthesitis, dactylitis, and skin or nail disease [9]. Ankylosing spondylitis primarily effects the axial skeleton and is characterized by sacroiliitis, enthesitis, and structural damage of sacroiliac joints and the spine [6, 10]. Approximately 50% of patients with AS report peripheral musculoskeletal manifestations of arthritis and enthesitis while 6–8% also have dactylitis [11]. Furthermore, patients with AS also report increased prevalence of extra-musculoskeletal manifestations including inflammatory bowel disease, psoriasis (PsO), and acute anterior uveitis varying from 6.8 to 25.8% [12].
Patients with AS and PsA often complain of pain, impaired physical function, and fatigue, that significantly impact patients’ health-related quality of life (HR-QoL) leading to disease-related early retirement [13, 14]. Although the pathogenic mechanisms underlying AS and PsA are not fully elucidated, existing evidence suggests that immune responses mediated by interleukin 17A (IL-17A) play a pivotal role in both diseases [15,16,17]. The IL-17A pathway is critical to bone erosion in PsA [18] and promotes osteoblast differentiation and increased mineralization, which may lead to ankyloses progression in AS [19].
Secukinumab is a fully human monoclonal antibody that directly inhibits IL-17A and has been approved for the treatment of AS and PsA based on evidence from the clinical development program which demonstrated sustained efficacy and a favorable safety profile [20,21,22,23]. In recent years, real-world data have been published on the use of secukinumab in AS and PsA [24, 25]. Chimenti et al. reported retention rates of about 75% in patients treated with secukinumab after 6–12 months of therapy [24], and Lindström et al. reported similar treatment retention and comparable primary response rates between secukinumab and adalimumab in PsA patients [25]. Furthermore, data from 13 registries of the European Spondyloarthritis (EuroSpA) Research Collaboration Network have also reported high 12-month retention rates in patients with axSpA and PsA [26, 27].
However, there is still a need for long-term drug retention data, effectiveness and safety of secukinumab in patients with AS and PsA in routine clinical practice. In addition, there are limited data on retreatment after discontinuation of secukinumab in patients with AS and PsA. Here, we report the 2-years interim analysis of SERENA evaluating the effectiveness, retention rates and the safety of secukinumab in PsA and AS patients in a real-life clinical setting.
Methods
Study Design and Patients
SERENA is an ongoing, longitudinal, non-interventional study with prospective and retrospective collection of primary data on the retention, safety, and effectiveness of secukinumab in patients with moderate-to-severe chronic plaque-type PsO, active PsA, or active AS. This study is being conducted at 438 sites with PsA and AS patients being enrolled across Europe [Austria, Belgium, Bulgaria, Croatia, Czech Republic, Estonia, France, Germany, Greece, Hungary, Ireland, Italy, Netherlands, United Kingdom], Israel and Russia. The design, eligibility criteria, methodology, and statistical analysis of this study have been published previously [28].
Patients aged ≥ 18 years with moderate-to-severe plaque PsO, PsA, or AS who had received secukinumab for at least 16 weeks before study registration were included in the study. Patients with medical or psychological conditions preventing them from participation in the study, or patients participating in other interventional clinical trial or in any other Novartis-sponsored non-interventional study (NIS) generating data on secukinumab treatment were excluded. Real-world data are collected prospectively in visits every 6 months after enrolment. The study will end either when all enrolled patients complete at least 2 years of follow-up or when the 5-years visit has been documented, whichever occurs later. This interim analysis included both target set population and safety set population (Supplementary Fig. 1). The safety set consisted of patients who received at least one dose of secukinumab treatment after signing the informed consent and the target set included patients fulfilling all of the inclusion criteria and none of the exclusion criteria.
The study was approved for each participating site according to the local regulations. The trial was conducted in accordance with the Guidelines for Good Pharmacoepidemiology Practices of the International Society for Pharmacoepidemiology (2008), the Strengthening the Reporting of Observational Studies in Epidemiology guidelines, the Declaration of Helsinki and each country’s local regulations.
The 2-years interim results from patients with active PsA or AS from the target population fulfilling all eligibility criteria in the study are presented here. The results for the PsO cohort will be reported elsewhere.
Assessments
The primary objective of this study is to assess the long-term retention of secukinumab in routine clinical practice in patients with PsA or AS. The retention rate was assessed based on the first dose of secukinumab administered after enrolment in the study. Secondary objectives of the study were to describe the long-term effectiveness of secukinumab in routine clinical practice for the treatment of PsA and AS.
For PsA patients, 78 total joint count (TJC) and 76 swollen joint count (SJC), dactylitis [29, 30], Physician’s Global Assessment (PGA) [31], pain assessed using a visual analogue scale (VAS) [32], and enthesitis assessment (Leeds Enthesitis Index, LEI) [33] were evaluated in the target set population.
For AS patients, Bath AS Disease Activity Index (BASDAI) [34], patient’s global assessment of disease activity (PtGA) using numeric rating scale (NRS) [35], C-reactive protein (CRP) and/or high sensitivity C-reactive protein (hsCRP) [36], AS Disease Activity Score (ASDAS) [34], total spinal pain VAS [37], and enthesitis assessment (Maastricht Ankylosing Spondylitis Enthesitis Score, MASES) [38] were assessed in the target set. Long-term health status was evaluated based on patient reported outcomes routinely used for patients with PsA (such as Health Assessment Questionnaire -Disability Index [HAQ-DI] and Functional Assessment of Chronic Illness Therapy [FACIT-Fatigue]) and AS (such as FACIT-Fatigue).
Safety assessments included: number of patients reporting adverse events (AEs), serious adverse events (SAEs), secukinumab exposure time, and AEs of special interest.
Statistical Analyses
Descriptive statistics were used to analyze the data presented as observed. Effectiveness data were assessed in all patients of the target set while safety data were analyzed in all patients who received at least one dose of secukinumab after providing written informed consent.
Quantitative data are presented by N, mean, standard deviation, and selected quantiles: minimum (0%), lower quartile (25%), median (50%), upper quartile (75%) and maximum (100%). Qualitative variables are presented as absolute and relative frequency distributions. Two-sided 95% confidence intervals (CI) were provided for all binary response rates. Retention rate was defined as the percentage of patients who have not discontinued secukinumab treatment, while a treatment break was defined as interruption of secukinumab therapy for at least 3 months after last injection.
Results
Baseline Characteristics and Patient Demographics
Of 1004 patients enrolled, 534 patients with active PsA and 470 patients with active AS were included in the current interim analysis. Nine patients who did not receive secukinumab for at least 16 weeks prior to the study or who did not take secukinumab according to the approved product information were excluded. PsA patients, with a mean (SD) age of 52.5 (11.9) years, were older than AS patients with a mean (SD) age of 46.6 (11.8) years. Nearly 45% of PsA and 60% of the AS patients were male with a mean (SD) duration of 1.00 (0.54) years and 0.91 (0.49) years of secukinumab treatment prior to inclusion in PsA and AS patients, respectively (Table 1). The mean time since diagnosis was longer in patients with AS [9.8 (9.5) years] compared to PsA patients [8.7 (7.5) years]. About 34.3% (n = 149) and 26.1% (n = 104) of patients with PsA and AS had BMI > 30 kg/m2at baseline. At least 40% of all patients were either current or former smokers and the number of patients with smoking history was similar in both the study groups.
At baseline, 6.4 and 19.4% of PsA patients had dactylitis and enthesitis, respectively, while the mean (SD) BASDAI score was 3.2 (2.3) in patients with AS (Table 2). Medications prior to study enrolment have been previously described [29]. The proportion of PsA and AS patients who had received biologic therapy prior to treatment with secukinumab were 67.4 and 62.8%, respectively. Approximately 23.2 and 18.3% patients were prescribed ≥ 3 biological therapies prior to the initiation of secukinumab and 89.2 and 87.1% discontinued the previous biologic therapy due to lack of efficacy in the AS and PsA patient groups, respectively. About 29.7% of patients with PsA and 10.4% of patients with AS were on concomitant methotrexate.
Retention Rate
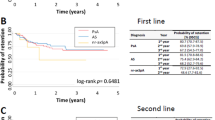
High retention rates of 85.2% for PsA and 85.8% for AS patients were observed after 1 year in the study while 74.9 and 78.9% of patients remained on secukinumab over 2 years, respectively (Fig. 1). The major reasons for drug discontinuation in the PsA and AS patients were lack of efficacy (38.7 and 33.6%) and patients’ decision to discontinue treatment (21.9 and 19.3%).
Effectiveness
In the PsA cohort, the mean SJC and TJC scores were sustained through 2 years after enrolment (Table 2). The proportion of patients with dactylitis and enthesitis was 6.4 and 19.4% at baseline, and 4.0 and 15.3% at year 2, respectively. Similar trends were also observed over 2 years for other efficacy outcomes including total pain, PGA 0/1 response and nail involvement, and QoL outcomes as measured through HAQ-DI and FACIT-Fatigue (Table 2).
In the AS cohort, mean BASDAI scores were sustained through 2 years after enrolment (Table 2). The disease activity status based on ASDAS-CRP also remained stable through 2 years after enrolment (Fig. 2). A similar trend was also observed across other efficacy outcomes including total and nocturnal back pain (Table 2).
Treatment Interruption
A total of 73 patients (PsA, n = 31 and AS, n = 42) interrupted secukinumab treatment with AEs being the most common reason in 58.1 and 45.2% of PsA and AS patients, respectively. The other reasons for treatment interruption in patients with PsA and AS included COVID-19 outbreak, possibly due to imposed lockdowns (3.2 and 14.3%), patients’ decision (9.7 and 7.1%) and unspecified reasons (19.4 and 11.9%%). The median (min, max) treatment break duration was approximately 125.0 (61, 461) days in PsA patients and 118.0 (61, 813) days in AS patients. The patients with PsA and AS had received secukinumab prior to treatment interruption for a mean (SD) duration of 607.5 (352.2) days and 631.5 (328.4) days, respectively..
Retreatment was started with maintenance dosing in 80.6% of PsA and 76.2% of AS patients. Only two patients (6.5%) with PsA and three patients (7.1%) with AS reinitiated secukinumab treatment with a loading regimen.
In PsA patients, the mean (SD) SJC and TJC were 1.3 (1.0) and 7.2 (11.4) prior to the treatment interruption and 0.4 (0.5) and 2.0 (0.7) at the assessment closest to 6 months after the treatment interruption (Supplementary Figure S2).
In AS patients, the mean (SD) PtGA and BASDAI were 4.4 (2.1) and 3.9 (2.4) prior to the treatment interruption, and 4.9 (2.3) and 3.9 (2.6) at the assessment closest to 6 months after the treatment interruption (Supplementary Figure S3).
Safety Assessments
Fifty-one percent of PsA and 51.3% AS patients had at least one AE. At least one serious adverse event (SAE) was reported by 8.3 and 10.4% of PsA and AS patients, respectively. Around 15 and 12% of patients with PsA and AS discontinued the study due to the occurrence of AEs. The commonly reported AEs leading to drug discontinuation included lack of efficacy (9.4 and 7.2%) and psoriasis (1.9 and 0.2%) in PsA and AS cohorts, respectively. No death was reported in PsA patients whereas there was one death in the AS cohort, which was not related to study drug (Table 3).
Treatment-emergent AEs of special interest included Candida infections (0.2 and 0.2%), malignancy (1.0 and 0.3%), major adverse cardiac events (MACE) (0.1 and 0.3%), injection site reactions (0 and 0.2%) and inflammatory bowel disease (0 and 0.1%) in PsA and AS patients, respectively (Table 3).
Discussion
SERENA provides real-world data across 17 European countries, Israel and Russia for PsO, PsA and AS patients treated with secukinumab. The interim results of the current study demonstrate high retention rates of 74.9 and 78.9% in PsA and AS patients, respectively, over 2 years comparable with results of the pivotal clinical trials of secukinumab. The 2-year data from the phase 3 FUTURE 5 study involving PsA patients has reported that 78.6% of patients completed the full 2-year treatment period [39]. Similarly, the 3-year data from the phase 3 MEASURE 2 trial reported high retention rates varying between 76 and 86% in patients with AS [40].
Furthermore, the EXCEED study evaluating the efficacy and safety of secukinumab versus adalimumab has also reported a high retention rate after 1 year treatment with secukinumab compared to adalimumab (86 vs. 76%) in patients with active PsA [41]. The EuroSpA research collaboration network has reported retention rates of 86%/76% and 82%/72% following 6/12 months of secukinumab treatment in patients with PsA and axSpA, respectively [26, 27]. The results of our study also demonstrated sustained effectiveness of secukinumab for dactylitis and enthesitis resolution, total pain, nail involvement, and QoL in PsA patients. These results are consistent with the FUTURE studies [23, 42,43,44,45] where secukinumab provided sustained improvements in the signs and symptoms across the six clinical manifestations of PsA throughout treatment.
AS patients often present with fluctuations in various outcome measures over time including BASDAI, and VAS pain [46]. In the current study, AS patients showed sustained effectiveness in terms of physical function and QoL over the course of the study in line with phase 3 secukinumab studies in AS patients [47, 48]. Another real-world evidence study evaluating the safety and efficacy of secukinumab in PsA and AS patients for 1 year also demonstrated a similar efficacy and safety profile as the interim results of this study [24].
In the current study, treatment interruptions were reported in a low number of patients. While adverse events were the main cause for treatment interruption, there were also a few cases where treatment was interrupted for unspecified reasons, which may include reasons such as surgery, travel, changes in healthcare coverage, or restrictions and lockdowns imposed owing to the ongoing pandemic situation. Interestingly, treatment was reinitiated at maintenance dose of secukinumab although secukinumab was interrupted for several months, indicating the sustained effectiveness of secukinumab despite drug interruption.
Similar to the results of the key clinical trials in PsA and AS, the interim results of the SERENA study suggest a favorable safety profile of secukinumab in a real-world setting with no unexpected AEs reported over at least 2 years after inclusion in the study in the real-world setting [23, 44, 47, 48].
SERENA is a large-scale, multinational study investigating long-term retention, effectiveness, and safety outcomes in patients treated with secukinumab in everyday clinical practice and provides real-world data across the SpA spectrum under the same setting, time frame, and data collection standards. The limitations of this study have been previously reported [28]. These result from the observational nature of the study including absence of control group, incomplete data, and selection bias. As the main objective of this study is to focus on the long-term drug retention and safety rather than initial effectiveness of secukinumab treatment, selection bias was inevitably introduced as patients were treated for at least 16 weeks with secukinumab prior to enrolment. It is also worth noting that the reported data reflect the effectiveness of secukinumab only for patients who remained on treatment at the follow-up visits. As the SERENA study was conducted in 15 countries in Europe, Israel, and Russia, findings cannot be generalized to all patients with PsA and AS worldwide. In addition, there was an imbalance between the numbers of patients enrolled in countries. Since the data have been collected retrospectively for up to 6 years for some individuals, underreporting of prior medications and more importantly of adverse events cannot be ruled out. Incomplete data due to lack of rigorous monitoring is an intrinsic weakness of observational studies and must be considered while interpreting findings in a real-world setting. It should also be noted that in the current analysis, more stringent treatment goals such as minimal disease activity (MDA) were not assessed. Further studies assessing the effect of treatment on treat-to-target goals, and the impact of confounding variables such as comorbidities on treatment outcomes in PsA and AS patients, are warranted.
Conclusions
The present analysis reports for the first time, retention rates and effectiveness of secukinumab for at least 2 years after initiation and treatment interruption data. Secukinumab demonstrated high retention rates and sustained effectiveness for over at least 2 years after inclusion in the study in PsA and AS patients in the real-world setting. Treatment interruptions may occur in clinical practice due to a variety of safety-related, personal, and circumstantial reasons. No impact on the effectiveness of secukinumab over the intermediate treatment breaks was observed. Safety data collected prospectively for up to 2 years confirm the favorable safety profile of secukinumab and do not reveal any new signals.
References
Feld J, Chandran V, Haroon N, Inman R, Gladman D. Axial disease in psoriatic arthritis and ankylosing spondylitis: a critical comparison. Nat Rev Rheumatol. 2018;14(6):363–71.
Schreiber S, Colombel J-F, Feagan BG, et al. Incidence rates of inflammatory bowel disease in patients with psoriasis, psoriatic arthritis and ankylosing spondylitis treated with secukinumab: a retrospective analysis of pooled data from 21 clinical trials. Ann Rheum Dis. 2019;78(4):473–9.
Stolwijk C, van Onna M, Boonen A, van Tubergen A. Global prevalence of spondyloarthritis: a systematic review and meta-regression analysis. Arthritis Care Res (Hoboken). 2016;68(9):1320–31.
Coates LC, Orbai AM, Azevedo VF, et al. Results of a global, patient-based survey assessing the impact of psoriatic arthritis discussed in the context of the Psoriatic Arthritis Impact of Disease (PsAID) questionnaire. Health Qual Life Outcomes. 2020;18(1):173.
Raychaudhuri SP, Raychaudhuri SK. Mechanistic rationales for targeting interleukin-17A in spondyloarthritis. Arthritis Res Ther. 2017;19(1):51.
Zhu W, He X, Cheng K, et al. Ankylosing spondylitis: etiology, pathogenesis, and treatments. Bone Res. 2019;7:22.
Talotta R, Atzeni F, Sarzi-Puttini P, Masala IF. Psoriatic arthritis: from pathogenesis to pharmacologic management. Pharmacol Res. 2019;148: 104394.
Sharip A, Kunz J. Understanding the pathogenesis of spondyloarthritis. Biomolecules. 2020;10(10):1461.
Coates LC, Helliwell PS. Psoriatic arthritis: state of the art review. Clin Med (Lond). 2017;17(1):65–70.
Garcia-Montoya L, Gul H, Emery P. Recent advances in ankylosing spondylitis: understanding the disease and management. F1000Res. 2018;7:1000 (Faculty Rev-512).
de Winter JJ, van Mens LJ, van der Heijde D, Landewé R, Baeten DL. Prevalence of peripheral and extra-articular disease in ankylosing spondylitis versus non-radiographic axial spondyloarthritis: a meta-analysis. Arthritis Res Ther. 2016;18(1):196.
Stolwijk C, van Tubergen A, Castillo-Ortiz JD, Boonen A. Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: a systematic review and meta-analysis. Ann Rheum Dis. 2015;74(1):65–73.
Rodrigues J, Rodrigues AM, Dias SS, Sousa RD, Branco JC, Canhao H. Psoriatic arthritis and ankylosing spondylitis impact on health-related quality of life and working life: a comparative population-based study. Acta Reumatol Port. 2019;44(4):254–65.
Sallam RA, Elbahnasawy AS. Health related quality of life (HRQoL) in ankylosing spondylitis patients: relation to clinical features, disease activity and radiographic damage. Egypt Rheumatol. 2020;42(4):287–90.
Deodhar A, Mease PJ, McInnes IB, et al. Long-term safety of secukinumab in patients with moderate-to-severe plaque psoriasis, psoriatic arthritis, and ankylosing spondylitis: integrated pooled clinical trial and post-marketing surveillance data. Arthritis Res Ther. 2019;21(1):111.
Blauvelt A, Chiricozzi A. The immunologic role of IL-17 in psoriasis and psoriatic arthritis pathogenesis. Clin Rev Allergy Immunol. 2018;55(3):379–90.
McGonagle DG, McInnes IB, Kirkham BW, Sherlock J, Moots R. The role of IL-17A in axial spondyloarthritis and psoriatic arthritis: recent advances and controversies. Ann Rheum Dis. 2019;78(9):1167–78.
Le Goff B, Bouvard B, Lequerre T, et al. Implication of IL-17 in bone loss and structural damage in inflammatory rheumatic diseases. Mediators Inflamm. 2019;2019:8659302.
Tang M, Lingyun L, Xijie Y. Interleukin-17A interweaves the skeletal and immune systems. Front Immunol. 2021. https://doi.org/10.3389/fimmu.2020.625034 (Article 625034).
McInnes IB, Mease PJ, Kirkham B, et al. Secukinumab, a human anti-interleukin-17A monoclonal antibody, in patients with psoriatic arthritis (FUTURE 2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2015;386(9999):1137–46.
Baeten D, Baraliakos X, Braun J, et al. Anti-interleukin-17A monoclonal antibody secukinumab in treatment of ankylosing spondylitis: a randomised, double-blind, placebo-controlled trial. Lancet. 2013;382(9906):1705–13.
Pavelka K, Kivitz A, Dokoupilova E, et al. Efficacy, safety, and tolerability of secukinumab in patients with active ankylosing spondylitis: a randomized, double-blind phase 3 study, MEASURE 3. Arthritis Res Ther. 2017;19(1):285.
Nash P, Mease PJ, McInnes IB, et al. Efficacy and safety of secukinumab administration by autoinjector in patients with psoriatic arthritis: results from a randomized, placebo-controlled trial (FUTURE 3). Arthritis Res Ther. 2018;20(1):47.
Chimenti MS, Fonti GL, Conigliaro P, et al. One-year effectiveness, retention rate, and safety of secukinumab in ankylosing spondylitis and psoriatic arthritis: a real-life multicenter study. Expert Opin Biol Ther. 2020;20(7):813–21.
Lindström U, Glintborg B, Di Giuseppe D, et al. Comparison of treatment retention and response to secukinumab versus tumour necrosis factor inhibitors in psoriatic arthritis. Rheumatology (Oxford). 2021;60(8):3635–45.
Michelsen B, Lindström U, Codreanu C, et al. Drug retention, inactive disease and response rates in 1860 patients with axial spondyloarthritis initiating secukinumab treatment: routine care data from 13 registries in the EuroSpA collaboration. RMD Open. 2020;6(3): e001280.
Michelsen B, Georgiadis S, Di Giuseppe D, et al. Real-world 6 and 12-month drug retention, remission and response rates of secukinumab in 2017 psoriatic arthritis patients in 13 European countries. Arthritis Care Res (Hoboken). 2021. (Online ahead of print)
Kiltz U, Sfikakis PP, Gaffney K, et al. Secukinumab use in patients with moderate to severe psoriasis, psoriatic arthritis and ankylosing spondylitis in real-world setting in Europe: baseline data from SERENA Study. Adv Ther. 2020;37(6):2865–83.
Gladman DD, Mease PJ, Krueger G, et al. Outcome measures in psoriatic arthritis. J Rheumatol. 2005;32(11):2262–9.
Mease PJ. Measures of psoriatic arthritis: tender and swollen joint assessment, psoriasis area and severity index (PASI), nail psoriasis severity index (NAPSI), modified nail psoriasis severity index (mNAPSI), Mander/Newcastle enthesitis index (MEI), Leeds enthesitis index (LEI), Spondyloarthritis Research Consortium of Canada (SPARCC), Maastricht ankylosing spondylitis enthesis score (MASES), Leeds dactylitis index (LDI), patient global for psoriatic arthritis, dermatology life quality index (DLQI), psoriatic arthritis quality of life (PsAQOL), functional assessment of chronic illness therapy-fatigue (FACIT-F), psoriatic arthritis response criteria (PsARC), psoriatic arthritis joint activity index (PsAJAI), disease activity in psoriatic arthritis (DAPSA), and composite psoriatic disease activity index (CPDAI). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S64-85.
Weisman S, Pollack CR, Gottschalk RW. Psoriasis disease severity measures: comparing efficacy of treatments for severe psoriasis. J Dermatol Treat. 2003;14(3):158–65.
Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S240–52.
Healy PJ, Helliwell PS. Measuring clinical enthesitis in psoriatic arthritis: assessment of existing measures and development of an instrument specific to psoriatic arthritis. Arthritis Rheum. 2008;59(5):686–91.
Zochling J. Measures of symptoms and disease status in ankylosing spondylitis: ankylosing spondylitis disease activity score (ASDAS), ankylosing spondylitis quality of life scale (ASQoL), Bath ankylosing spondylitis disease activity index (BASDAI), Bath ankylosing spondylitis functional index (BASFI), Bath ankylosing spondylitis global score (BAS-G), Bath ankylosing spondylitis metrology index (BASMI), Dougados functional index (DFI), and health assessment questionnaire for the spondylarthropathies (HAQ-S). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S47-58.
Sieper J, Rudwaleit M, Baraliakos X, Brandt J, Braun J, Burgos-Vargas R, et al. The assessment of spondyloarthritis international society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis. 2009;68(Suppl 2):ii1–44.
Machado PM, Landewé RB, van der Heijde DM. Endorsement of definitions of disease activity states and improvement scores for the ankylosing spondylitis disease activity score: results from OMERACT 10. J Rheumatol. 2011;38(7):1502–6.
Knop C, Oeser M, Bastian L, Lange U, Zdichavsky M, Blauth M. Development and validation of the visual analogue scale (VAS) Spine Score. Unfallchirurg. 2001;104(6):488–97.
Heuft-Dorenbosch L, Spoorenberg A, van Tubergen A, et al. Assessment of enthesitis in ankylosing spondylitis. Ann Rheum Dis. 2003;62(2):127–32.
Mease PJ, Landewé R, Rahman P, et al. Secukinumab provides sustained improvement in signs and symptoms and low radiographic progression in patients with psoriatic arthritis: 2-year (end-of-study) results from the FUTURE 5 study. RMD Open. 2021;7(2): e001600.
Marzo-Ortega H, Sieper J, Kivitz A, et al. Secukinumab provides sustained improvements in the signs and symptoms of active ankylosing spondylitis with high retention rate: 3-year results from the phase III trial, MEASURE 2. RMD Open. 2017;3(2): e000592.
McInnes IB, Behrens F, Mease PJ, et al. Secukinumab versus adalimumab for treatment of active psoriatic arthritis (EXCEED): a double-blind, parallel-group, randomised, active-controlled, phase 3b trial. Lancet. 2020;395(10235):1496–505.
Mease PJ, Kavanaugh A, Reimold A, et al. Secukinumab provides sustained improvements in the signs and symptoms of psoriatic arthritis: final 5-year results from the phase 3 FUTURE 1 study. ACR Open Rheumatol. 2020;2(1):18–25.
McInnes IBM, Mease PJM, Kivitz AJM, Peter Nash M, Proton Rahman M, Jürgen Rech M, et al. Long-term efficacy and safety of secukinumab in patients with psoriatic arthritis: 5-year (end-of-study) results from the phase 3 FUTURE 2 study. Lancet Rheumatol. 2020;2(4):e227–35.
Kivitz AJ, Nash P, Tahir H, et al. Efficacy and safety of subcutaneous secukinumab 150 mg with or without loading regimen in psoriatic arthritis: results from the FUTURE 4 study. Rheumatol Ther. 2019;6(3):393–407.
van der Heijde D, Mease PJ, Landewé RBM, et al. Secukinumab provides sustained low rates of radiographic progression in psoriatic arthritis: 52-week results from a phase 3 study, FUTURE 5. Rheumatology (Oxford). 2020;59(6):1325–34.
Essers I, Boonen A, Busch M, et al. Fluctuations in patient reported disease activity, pain and global being in patients with ankylosing spondylitis. Rheumatology (Oxford). 2016;55(11):2014–22.
Baraliakos X, Braun J, Deodhar A, et al. Long-term efficacy and safety of secukinumab 150 mg in ankylosing spondylitis: 5-year results from the phase III MEASURE 1 extension study. RMD Open. 2019;5(2): e001005.
Marzo-Ortega H, Sieper J, Kivitz AJ, et al. 5-year efficacy and safety of secukinumab in patients with ankylosing spondylitis: end-of-study results from the phase 3 MEASURE 2 trial. Lancet Rheumatol. 2020;2(6):e339–46.
Acknowledgements
This study was designed by the scientific steering committee and Novartis personnel. The authors thank the patients who participated in this study; the study investigators; John Gallagher, Novartis Pharmaceuticals UK Limited, London, UK, for medical guidance and valuable review.
Funding
This study and the journal’s Rapid Service Fee were funded by Novartis Pharma AG, Basel, Switzerland.
Medical Writing, Editorial, and Other Assistance
Medical writing support, under the guidance of the authors, was provided by Dhanya Mukundan, Novartis Healthcare Private Limited, Hyderabad, India. Medical writing support was funded by Novartis.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICJME) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
U Kiltz, P Sfikakis, K Gaffney, A Bounas, N Gullick, E Lespessailles, J Brandt-Juergens, and R Rashkov were involved in conception or design of the work, acquisition of data, and interpretation of the results. B Schulz, E Pournara, and P Jagiello were involved in the analysis plan of the study, analysis of the data, and interpretation of the results. All authors were responsible for critically revising the work for important intellectual content and for making all content and editorial decisions. All authors had final approval of the manuscript version to be published and are accountable for all aspects of the work in ensuring the accuracy and integrity of this manuscript.
List of Investigators
The full list of investigators for the SERENA study not included as authors is shown in Supplementary Table 1.
Prior Publication
The data from this study were partially presented at ACR 2021.
Disclosures
Uta Klitz: Research grants, support and/or consultancy fees from AbbVie, Biocad, Biogen, Chugai, Eli Lilly, Grünenthal, Hexal, Janssen, MSD, Novartis, Pfizer, Roche and UCB; Petros P. Sfikakis: Research grants, support and consultancy fees from AbbVie, Amgen, Boehringer Ingelheim, Celgene, Eli-Lilly, Janssen, Novartis and Pfizer; Karl Gaffney: Research grants, consultancy fees and/or speaker fees from AbbVie, Celgene, Lilly, Pfizer, Gilead, MSD, Novartis and UCB; Andreas Bounas: None to disclose; Nicola Gullick: Research support, consultancy fees and/or speakers fees from AbbVie, Celgene, Eli Lilly, Izana, Janssen, Novartis, UCB; Eric Lespessailles: Received speaker and consultant fees from Amgen, Expanscience, Lilly and MSD, and research grants from AbbVie, Amgen, Lilly, MSD and UCB; Jan Brandt-Juergens: Consultancy fees and speaker honoraria from AbbVie, Pfizer, Roche, Sanofi-Aventis, Novartis, Lilly, MSD, UCB, BMS, Janssen, and Medac; Rasho Rashkov: Consultancy fees and speaker honoraria from AbbVie, Amgen, Pfizer, Novartis, MSD, UCB, Roche and Janssen; Barbara Schulz: Employee of Novartis; Effie Pournara: Employee of Novartis with Novartis stock; Piotr Jagiello: Employee of Novartis.
Compliance with Ethics Guidelines
This study was conducted in accordance with Good Clinical Practice and the Declaration of Helsinki of 1964 and its later amendments. The study was approved by independent ethics committees or institutional review boards of participating centers (Supplementary Table 2). All patients provided written informed consent before any study-related procedures were undertaken.
Data Availability
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as Supplementary Material. The data sets generated during and/or analyzed during the current study are not publicly available. Novartis is committed to sharing with qualified external researchers’ access to patient-level data and supporting clinical documents from eligible studies. These requests are reviewed and approved on the basis of scientific merit. All data provided is anonymized to respect the privacy of patients who have participated in the study in line with applicable laws and regulations. The data may be requested by writing to the corresponding author.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kiltz, U., Sfikakis, P.P., Gaffney, K. et al. Interim 2-Year Analysis from SERENA: A Real-World Study in Patients with Psoriatic Arthritis or Ankylosing Spondylitis Treated with Secukinumab. Rheumatol Ther 9, 1129–1142 (2022). https://doi.org/10.1007/s40744-022-00460-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-022-00460-x