Abstract
Introduction
Emergency department visits for cutaneous abscesses are increasing. It is important for healthcare professionals to be proficient in identifying and treating abscesses. Loop drainage technique (LDT) is a newer technique which has been described in several articles but limited resources for teaching have been studied. The objective of this study was to compare 3 models for learning and teaching the LDT.
Methods
This was a prospective survey study of a convenience sample of emergency medicine residents at a large urban academic center. Residents volunteered to participate during a scheduled cadaver and simulation session. After a self-directed review of the LDT, each participant performed ultrasound visualization and then the LDT on 3 simulated abscesses: a cadaveric model, a commercial abscess pad, and a homemade phantom. Participants completed pre- and post-simulation surveys.
Results
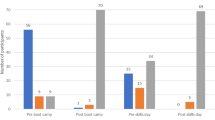
Of 57 residents, 28 participated in the 1-day simulation. The majority (57.1%, p < 0.009) preferred the cadaver model for learning the LDT, and 78.6% reported it to have the most realistic physical examination for an abscess (p = 0.001). Prior to participation, 0% of residents felt proficient performing LDT. After participation, 46.4% of residents felt proficient and 78.6% reported intent to use in clinical practice (p < 0.001).
Conclusions
Simulation is an effective educational tool for both learning new skills and improving procedural competency. Residents found cadavers provided the most realistic physical examination, and the majority preferred it for learning the LDT. However, cadavers are not always accessible, an important factor when considering various educational settings.


Similar content being viewed by others
Notes
The cling film keeps the brown sugar and gelatin from mixing and allows the mold to be used multiple times.
Abbreviations
- ED:
-
Emergency department
- EM/IM:
-
Emergency medicine/internal medicine
- EM/Peds:
-
Emergency medicine/pediatrics
- I&D:
-
Incision and drainage
- LDT:
-
Loop drainage technique
References
Taira BR, Singer AJ, Thode HC, Lee CC. National epidemiology of cutaneous abscesses: 1996 to 2005. Am J Emerg Med. 2009;27(3):289–92. https://doi.org/10.1016/j.ajem.2008.02.027.
Kaye KS, Petty LA, Shorr AF, Zilberberg MD. Current epidemiology, etiology, and burden of acute skin infections in the United States. Clin Infect Dis. 2019;68(Supplement_3):S193–9. https://doi.org/10.1093/cid/ciz002.
Fritz SA, Shapiro DJ, Hersh AL. National trends in incidence of purulent skin and soft tissue infections in patients presenting to ambulatory and emergency department settings, 2000–2015. Clin Infect Dis Off Publ Infect Dis Soc Am. 2020;70(12):2715–8. https://doi.org/10.1093/cid/ciz977.
Cairns C, Kang K, Santo L. National hospital ambulatory medical care survey: 2018 emergency department summary tables. https://www.cdc.gov/nchs/data/nhamcs/web_tables/2018-ed-web-tables-508.pdf.
Singer AJ, Talan DA. Management of skin abscesses in the era of methicillin-resistant Staphylococcus aureus. N Engl J Med. 2014;370(11):1039–47. https://doi.org/10.1056/NEJMra1212788.
Pallin DJ, Egan DJ, Pelletier AJ, Espinola JA, Hooper DC, Camargo CA. Increased US emergency department visits for skin and soft tissue infections, and changes in antibiotic choices, during the emergence of community-associated methicillin-resistant Staphylococcus aureus. Ann Emerg Med. 2008;51(3):291–8. https://doi.org/10.1016/j.annemergmed.2007.12.004.
Tsoraides SS, Pearl RH, Stanfill AB, Wallace LJ, Vegunta RK. Incision and loop drainage: a minimally invasive technique for subcutaneous abscess management in children. J Pediatr Surg. 2010;45(3):606–9. https://doi.org/10.1016/j.jpedsurg.2009.06.013.
Thompson DO. Loop drainage of cutaneous abscesses using a modified sterile glove: a promising technique. J Emerg Med. 2014;47(2):188–91. https://doi.org/10.1016/j.jemermed.2014.04.035.
Ladde J, Baker S, Lilburn N, Wan M, Papa L. A randomized controlled trial of novel loop drainage technique versus standard incision and drainage in the treatment of skin abscesses. Kuehl DR, ed. Acad Emerg Med. 2020;27(12):1229–40. https://doi.org/10.1111/acem.14106.
Passiment M, Sacks H, Huang G. Medical simulation in medical education: results of an AAMC Survey. https://www.aamc.org/system/files/c/2/259760-medicalsimulationinmedicaleducationanaamcsurvey.pdf.
Russell E, Hall AK, Hagel C, Petrosoniak A, Dagnone JD, Howes D. Simulation in Canadian postgraduate emergency medicine training - a national survey. CJEM. 2018;20(1):132–41. https://doi.org/10.1017/cem.2017.24.
Higgins M, Madan C, Patel R. Development and decay of procedural skills in surgery: a systematic review of the effectiveness of simulation-based medical education interventions. Surgeon. 2021;19(4):e67–77. https://doi.org/10.1016/j.surge.2020.07.013.
McMillan HJ, Writer H, Moreau KA, et al. Lumbar puncture simulation in pediatric residency training: Improving procedural competence and decreasing anxiety. BMC Med Educ. 2016;16:198. https://doi.org/10.1186/s12909-016-0722-1.
Fitch MT, Manthey DE, McGinnis HD, Nicks BA, Pariyadath M. A skin abscess model for teaching incision and drainage procedures. BMC Med Educ. 2008;8(1):38. https://doi.org/10.1186/1472-6920-8-38.
Yang JH, Kim YM, Chung HS, et al. Comparison of four manikins and fresh frozen cadaver models for direct laryngoscopic orotracheal intubation training. Emerg Med J EMJ. 2010;27(1):13–6. https://doi.org/10.1136/emj.2008.066456.
Takayesu JK, Peak D, Stearns D. Cadaver-based training is superior to simulation training for cricothyrotomy and tube thoracostomy. Intern Emerg Med. 2017;12(1):99–102. https://doi.org/10.1007/s11739-016-1439-1.
Acknowledgements
The authors acknowledge the University of Maryland MASTRI Simulation Center, Maryland State Anatomy Board, for use of their respective spaces. Deborah M. Stein, ELS, provided language and technical editing of the manuscript.
Funding
This study received funding from the University of Maryland School of Medicine, Department of Emergency Medicine Resident Research Grant; the funder had no involvement in study design, collection/analysis/interpretation of data, writing of report, and decision for submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
NA.
Informed Consent
Waiver of informed consent was obtained by the institutional review board.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A The Who, What, When, Where, Why, and How of Loop Drainage Technique
Who can do it?
You can do it!
What is it?
A method for draining abscess.
When can you do it?
Loop drainage technique has predominantly been studied in pediatric populations but there has been push to perform and evaluate the technique in adult populations with abscesses, which can be treated by simple incision and drainage.
Where can you do it?
In the office, clinic, emergency department, operating room, or any setting as you see fit.
Why should you do it?
The loop drainage method (LDM) was first introduced by Tsoraides et al. in 2010. This method has the potential to successfully treat these conditions in a less painful manner with better cosmetic outcomes and decreases the frequency for return evaluation for repacking. Thompson et al. conducted a literature review in 2014. He concluded that based on these research studies and their findings, loop drainage may be a better alternative to packing material for the following reasons: it is less painful, there is no need for packing changes, there are fewer follow-up visits required, and there is less treatment failure.
How do you do it?
You should start by evaluating and diagnosing an abscess just like you would in any other patient presenting with such a concern on exam. Once the abscess and its borders have been identified, you should clean, prep, and anesthetize the area in typical fashion. You will then make an incision at the apex of the area of fluctuance. Then, insert your hemostat and break up loculations within the abscess. You will then need to make a small additional incision at another site along the abscess which can be reached with the hemostat from inside the initial incision. You should next express and flush the abscess to remove purulent material. You will then pull through a sterile “loop” (penrose drain, end loop from sterile glove, vessel loop, other sterile loops) from the 2nd incision through the abscess area and out the initial incision. Next, loosely tie the two ends together to create the “loop.” You can tie the ends like you would on the ends of a suture, with a hand tie or instrument tie. It is important to keep some space within the loop, and not cause too much tension on the skin. A loop too tight can cause skin breakdown and necrosis. This loop should remain in place until the abscess has resolved and it can then be removed, typically around 7–14 days later. (Thompson).
References
Here we reproduced a copyrighted image showing participants an example of the loop drainage technique.
-
Tsoraides SS, Pearl RH, Stanfill AB, Wallace LJ, Vegunta RK. Incision and loop drainage: a minimally invasive technique for subcutaneous abscess management in children. J Pediatr Surg [Internet] 2010;45(3):606–9. Available from: https://doi.org/10.1016/j.jpedsurg.2009.06.013
-
Thompson DO. Loop drainage of cutaneous abscesses using a modified sterile glove: a promising technique. J Emerg Med [Internet] 2014;47(2):188–91. Available from: https://doi.org/10.1016/j.jemermed.2014.04.035
-
Picture: https://pubmed.ncbi.nlm.nih.gov/24305529/ per https://www.semanticscholar.org/paper/Loop-and-drain-technique-for-subcutaneous-abscess%3A-Gaszynski-Punch/2fd9481f6697e7019910e2158c0a42a800e700f5/figure/0
Appendix B Pre- and Post-Simulation Surveys



Appendix C Instructions for Making 12 Homemade Gelatin Abscess Phantoms
Materials Needed
Purulent material
-
2 tablespoons maple syrup
-
½ cup mayonnaise
-
Twelve 7-in. rubber balloons
-
Piping bag or syringe
Gelatin mixture
-
7 cups water
-
1 cup gelatin
-
1¼ tablespoons blue food coloring
-
½ cup iodine
-
\(\textstyle{\raisebox{1ex}{1}\!\left/ \!\raisebox{-1ex}{3}\right.}\) cup psyllium powder
Phantoms
-
6 kidney basins
-
Brown sugar
-
Roll of cling film
Steps
Create purulent material
-
1.
Mix maple syrup with mayonnaise
-
2.
Fill each balloon with approximately 10 mL of mixture until full using piping bag or syringe
-
3.
Tie balloons closed and cut off excess balloon material below knot
Create gelatin mixture
-
1.
Bring water to boil
-
2.
To boiling water, slowly add gelatin while stirring until dissolved
-
3.
Add food coloring and iodine to darken
-
4.
Add psyllium powder and stir until thoroughly mixed
-
5.
Allow mixture to cool until it is no longer steaming
Assemble the phantoms
-
1.
Prepare kidney basins by packing the bottom of each with brown sugar and forming 2 small indentations; cover tightly with cling filmFootnote 1


-
2.
Pour a small amount of gelatin mixture into each indentation and refrigerate 30 min to solidify

-
3.
Place a balloon filled with purulent material in each indentation and cover the balloons with gelatin mixture


-
4.
Refrigerate molds for a minimum of 4 h or leave overnight to solidify

-
5.
Turn molds upside down to remove them from kidney basins and cut each in half to make 2 phantoms


Rights and permissions
About this article
Cite this article
Rosenblatt, L.S., King, S.A., Callahan, M.E. et al. Which Way Would You Slice It? Evaluation of 3 Educational Models for the Loop Drainage Technique. Med.Sci.Educ. 32, 481–494 (2022). https://doi.org/10.1007/s40670-022-01530-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-022-01530-z