Abstract
Background
Transplant nephropathology is a highly specialized field of pathology comprising both the evaluation of organ donor biopsy for organ allocation and post-transplant graft biopsy for assessment of rejection or graft damage. The introduction of digital pathology with whole-slide imaging (WSI) in clinical research, trials and practice has catalyzed the application of artificial intelligence (AI) for histopathology, with development of novel machine-learning models for tissue interrogation and discovery. We aimed to review the literature for studies specifically applying AI algorithms to WSI-digitized pre-implantation kidney biopsy.
Methods
A systematic search was carried out in the electronic databases PubMed-MEDLINE and Embase until 25th September, 2021 with a combination of the key terms “kidney”, “biopsy”, “transplantation” and “artificial intelligence” and their aliases. Studies dealing with the application of AI algorithms coupled with WSI in pre-implantation kidney biopsies were included. The main theme addressed was detection and quantification of tissue components. Extracted data were: author, year and country of the study, type of biopsy features investigated, number of cases, type of algorithm deployed, main results of the study in terms of diagnostic outcome, and the main limitations of the study.
Results
Of 5761 retrieved articles, 7 met our inclusion criteria. All studies focused largely on AI-based detection and classification of glomerular structures and to a lesser extent on tubular and vascular structures. Performance of AI algorithms was excellent and promising.
Conclusion
All studies highlighted the importance of expert pathologist annotation to reliably train models and the need to acknowledge clinical nuances of the pre-implantation setting. Close cooperation between computer scientists and practicing as well as expert renal pathologists is needed, helping to refine the performance of AI-based models for routine pre-implantation kidney biopsy clinical practice.
Similar content being viewed by others
Introduction
Transplant nephropathology is a highly specialized field of pathology comprising both the evaluation of organ donor biopsy for organ allocation and post-transplant graft biopsy for assessment of rejection or graft damage. Recognizing and quantifying various organ structures and subtle histopathological features, and correlating these findings with clinical parameters are required to be of use for donor or recipient management in the current era of precision medicine [1]. Added challenges in this field include the increasing demand to render complex diagnoses in kidney biopsy samples, pressure of time constraints in the case of pre-implantation biopsy for organ allocation, and the lack of specifically trained nephropathologists. Moreover, when dealing with kidney transplant pathology, a distinction should be made between pre-transplant or time-zero donor biopsy and protocol biopsy on a graft kidney as the clinical setting and related challenges of these two scenarios are quite different. In a graft biopsy, simultaneous assessment of rejection and/or chronic organ damage is made by means of a multiplicity of ancillary techniques (e.g., immunohistochemistry for C4d, special stains for fibrosis or deposits, immunofluorescence or molecular investigations) on a biopsy specimen collected in optimal conditions with an expected turn-around-time (TAT) for results of days to weeks, usually assessed by reference pathologists with expertise in the field. On the other hand, pre-implantation biopsy for organ suitability to transplantation is usually assessed via frozen section (FS) or microwave rapid processing protocols of slides with no aid of ancillary techniques or only very few, with a time-critical diagnostic TAT diagnosis rendered by a general pathologist with relatively little specific expertise in this field. The Banff group developed definitions for features to be evaluated in kidney biopsy and scoring systems, but reproducibility even among experts remains an issue [2], and studies on correlation of pre-implantation biopsy and graft outcome have highlighted that expertise is crucial in predicting the true state of an organ and subsequent outcome [3, 4].
The introduction of digital pathology with whole-slide imaging (WSI) in clinical research, trials and practice has catalyzed the application of artificial intelligence (AI) in histopathology, with the development of novel machine-learning models for tissue interrogation and discovery. Such advances in technology offer the potential to improve our ability to classify disease, quantify morphological alterations more accurately, discover correlations with pathogenesis and clinical data, and predict disease outcome with new prediction models [5]. As reported in a recent review by Farris et al., interest in the application of AI algorithms towards the topic of kidney transplant has grown, as demonstrated by the increasing number of publications retrieved from PubMed with the keywords “computer & pathology & image & analysis” [6]. As highlighted from previous work [7], most efforts have been devoted to the post-transplant graft biopsy with algorithms aiming to quantify and describe features of rejection such as immune infiltrate, or to quantify chronic organ damage in terms of interstitial fibrosis with special stains. By comparison, studies regarding the application of AI algorithms to the pre-implantation biopsy are scarce and more focused on fewer simpler tasks, such as counting glomeruli, sclerotic glomeruli, vascular structures, and quantification of interstitial fibrosis. Nevertheless, digital pathology with WSI has already been deployed in the pre-implantation setting for consultation and training [8,9,10,11].
In this work we systematically reviewed the literature searching for all studies applying AI algorithms to digitized slides of pre-implantation kidney biopsy. The various AI-based algorithms developed and deployed for this purpose are discussed, as are the potential benefits and main challenges encountered.
Methods
Search strategy
A systematic search was carried out in the electronic databases PubMed-MEDLINE and Embase until 25th September, 2021 with a combination of the key terms “kidney”, “biopsy”, “transplantation” and “artificial intelligence” and their aliases (see complete search strategy in the Supplementary Table 1). No language filters were applied. Two authors screened all retrieved items after removal of duplicates with the aid of the web-app Rayyan QRCI [12]. Briefly, the two authors screened abstracts blinded to each other’s decision and after finishing they compared the results of the screening. Disagreement was resolved by consensus. Then authors read the full text and decided on final inclusion, with consultation of a third author in case of disagreement.
PICOS analysis
Pre-implantation kidney biopsy (P) employing AI algorithms coupled with WSI (I) were compared to conventional assessment (C) to determine potential concordance rates and performance of algorithms (O). Studies concerning protocol graft biopsy for rejection, not dealing with AI algorithms or not deploying WSI, together with studies represented only by abstracts were excluded. Disagreement on article screening and final inclusion was resolved with the participation of a third reviewer. References listed in the excluded but relevant articles, as well as recent reviews on the topic were checked for additional studies that might be potentially included. Full-texts of relevant studies were acquired and checked, and data from included studies were extracted and summarized. Extracted data were: author, year and country of the study, type of biopsy features investigated, number of cases, type of algorithm deployed, main results of the study in terms of diagnostic outcome, and the main limitations of the study.
Results
After removal of duplicates, a total of 5761 publications were screened. Of these, 184 were selected as potentially relevant, and only seven were finally included [13,14,15,16,17,18,19]. Reasons for exclusion included: 23 with only an abstract available, 115 not using WSI, 11 not specifically concerned with the transplant setting, and 28 not dealing with pre-implantation biopsy. Only a few studies we identified regarding AI algorithms coupled with WSI were dedicated to pre-implantation biopsies, and they mainly focused on the detection and classification of glomerular structures and to a lesser extent tubular and vascular structures. Included studies reported the performance of the algorithms in terms of sensitivity and specificity or correlation with pathologists’ assessment as outcome measures. The included studies are summarized in Table 1.
Assessment and concordance rates
Marsh et al. in 2018 trained a deep-learning model based on a convolutional neural network (CNN) utilizing 48 WSI cases of kidney biopsy processed by FS. These authors tested the performance of their model to detect and classify normal and sclerosed glomeruli, demonstrating performance comparable to that of expert pathologists and reported robustness of their algorithm against slide preparation artifacts. In the training phase, normal and sclerosed glomeruli were annotated in the test set of biopsies obtained from 20 kidneys of 17 donors, with a range of glomerulosclerosis 1–72%. Annotation was undertaken by a senior resident and amended by a specialist nephropathologist, thus underscoring the importance of expert annotation in training AI algorithms. Two different CNN models were tested, an image patch-based and full WSI convolutional model. The fully convolutional model showed the best performance by more accurately measuring the proportion of correctly classified sclerosed glomeruli. The fully convolutional model also showed greater correlation with the percent global glomerulosclerosis evaluated (R2 = 0.828) compared with the patch-based model (R2 = − 0.491)[13]. Moreover, as these authors stressed, the model was not only robust to slide preparation artifacts such as tissue folds, but it was also capable of running the analysis within a time-span satisfactory for a FS request. Additional data reported by the same group of investigators in 2021 [14], where a deep-learning model was based on the model of their previous study, were challenged on a larger population of mixed wedge and core kidney biopsy cases (98 FS and 51 permanent sections). Again, the training set of biopsies was annotated by three certified pathologists with expertise in renal transplant pathology. Glomeruli counts were compared against annotation ground truth, with accuracy assessed by Pearson correlation coefficient r and root-mean-square error (RMSE). Corresponding quantities for percent global glomerulosclerosis were computed for on-call pathologists’ estimates, and those values were compared with the model’s performance [14]. Moreover, the authors used Cohen’s Kappa to test the concordance of the model with the ground truth derived from pathologists at the cut-off of 20% glomerulosclerosis for organ discard. The model correlated very well with the pathologists’ annotations, with a correlation coefficient higher than 0.900. Interestingly, when the pathologists were asked to check and correct the classification of glomeruli after the model had been run on a subset of 25 cases with different grades of glomerulosclerosis by visualizing the histology images with overlaid model-generated glomeruli classifications, the correlation with ground truth improved with respect to both the original on-call pathologists’ reports and to the model alone. This was underscored by the authors as indirect proof that their model could potentially be incorporated into routine clinical practice [14].
A group of Italian researchers shared slightly different semantic segmentation CNN models that were trained on small datasets of pre-implantation kidney biopsies stained with Periodic acid-Schiff (PAS) to detect vessel and tubular structures, starting with a lumen as an object and then extracting nuclei and membranes to classify the structure [16], or detect healthy and sclerosed glomeruli [15, 17]. Early work of this group utilized a binary classifier (vessel vs tubule) classification that was performed with Back Propagation Neural Network (BPNN) and Haralick texture features [16]. The classification provided by the algorithm in terms of counting vascular and tubular structures was compared to manual counting provided by an expert nephropathologist. They tested four different approaches to reduce false positives detected by the algorithm. The model always detected more vessels and tubules than the human expert, with a final precision in the test set of 0.91. These authors concluded that such an algorithm could be of aid to a pathologist assessing these structures, given that their task would be simplified and limited to a final check on the output of the algorithm [16]. Subsequent research by this Italian group focused on glomerular structure detection and classification as sclerosed or normal. The detection of glomeruli and their classification was based on the evaluation of several features, such as the sum of the area related to Bowman’s capsule, blood vessel area and the inter-capillary space, diameter, and texture features, with the use of two well-known texture analysis algorithms; namely, Local Binary Pattern (LBP) and Haralick features. A total of 150 features were extracted and reduced to 95 by a principal component analysis, and a shallow CNN final model was applied. The best performance achieved an accuracy and precision of 0.98, and the authors reported that the cases of misclassified glomeruli were reviewed by an expert pathologist who acknowledged the challenge of classifying such images and indicated that in routine practice such image fields would not be considered for evaluation [17]. In their subsequent work, the authors replaced the last layer of both SegNet [20] and DeepLab v3 + [21] networks with a pixel-wise classification layer with three output classes (background, sclerotic glomeruli and non-sclerotic glomeruli) to accomplish the same task. Both models worked better in the detection of non-sclerosed glomeruli and background tissue, i.e., the SegNet-based model yielded a better F-score for both classes of glomeruli , while the DeepLab v3 + -based model had a better F-score for non-sclerotic glomeruli and a slightly worse F-score for sclerotic glomeruli [15]. In both studies the authors stressed the importance of expert human annotation for reliably training models and the potential application of such computer-aided diagnosis tools for practicing pathologists. They also acknowledged that non-expert pathologists tend to overscore glomerulosclerosis, which may lead to excessive discarding of kidneys [3, 4].
Algorithms
Salvi et al. also designed algorithms to classify glomeruli, quantify tubular atrophy, detect blood vessels and quantify interstitial fibrosis on PAS-stained slides [18, 19]. Their algorithm, called RENFAST (Rapid Evaluation of Fibrosis And vessels Thickness), deals with semantic segmentation using CNN and employs U-Net architecture with a ResNet34 backbone [22]. A dataset of 65 kidney biopsies stained with PAS and a trichrome stain for fibrosis were manually annotated by an expert renal pathologist. The RENFAST algorithm yielded a balanced accuracy of 0.89 and a precision of 0.92 utilizing the test set for blood vessel detection and of 0.92 and 0.91, respectively, for fibrosis quantification; of note, average absolute errors between manual and computational assessment were lower than 2.5%. Moreover, these authors reported that their computational time was around 2 min, significantly less than the 20 min required by the pathologist to manually evaluate arterial and interstitial fibrosis [18]. The algorithm, named RENTAG (Robust Evaluation of Tubular Atrophy & Glomerulosclerosis), deployed by another study group [19], consisted of three modules: PAS normalization, glomerulosclerosis assessment, and tubular atrophy quantification. This algorithm was based on a deep convolutional network, with pixels labeled into three different classes depending on whether they belonged to healthy glomeruli/tubuli, sclerotic glomeruli/atrophic tubuli or other components of renal tissue and then subjected to a post-processing procedure. A total of 83 needle-core biopsy cases stained with PAS were used and annotated by two trained pathologists. The algorithm achieved high sensitivity and positive predictive value concerning correct classification of normal and sclerosed glomeruli and normal and atrophic tubuli, with a reported total time needed to run the analysis of around 3 min.
Discussion
As expected, we retrieved very few papers concerning AI and WSI slides of pre-implantation biopsy, as anticipated in previous reviews [7]. This is not surprising, considering that in many settings pre-implantation biopsies are evaluated with rapid protocols that are more prone to artifacts and pose challenges in standardization. Moreover, in the pre-implantation setting, the features of interest to be assessed are almost exclusively based upon morphology, given that any sort of score (Karpinski-Remuzzi [23, 24], donor score [4], Banff [2]) is based on relatively simple tasks such as counting and classifying glomeruli and quantifying interstitial fibrosis, tubular atrophy and vascular narrowing, usually with no availability of ancillary techniques such as special stains and immunohistochemistry. On the other hand, the development and testing of AI algorithms offers an opportunity for standardization. Indeed, many of the studies encountered in this review were about “narrow AI” because they dealt only with these elementary tasks (e.g. enumerating and classifying glomeruli and quantifying fibrosis). A brief overview of these studies is provided in Supplementary Table 2.
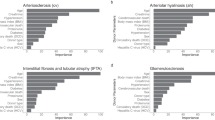
Animal model-derived samples were deployed in several studies, most of which dealt with glomerular detection [25,26,27,28,29,30,31,32,33], or unspecified human kidney biopsies with no reference to the pre-implantation setting or specific pathology [34,35,36,37,38]. Only three larger-sized studies applied segmentation CNN models to the detection and simultaneous classification of multiple renal structures, not only glomeruli but also different kinds of tubuli and vessels [39,40,41]. In particular, Hermsen et al. [39] developed a multiclass segmentation CNN that achieved a high Dice coefficient for all of the segmentation classes (“glomeruli,” “sclerotic glomeruli,” “empty Bowman’s capsules,” “proximal tubuli,” “distal tubuli,” “atrophic tubuli,” “undefined tubuli,” “capsule,” “arteries,” and “interstitium”), with the best results being yielded by glomerular detection, followed by tubules as a whole class and then the interstitium. Their AI-based algorithm was validated not only in a single-center experimentation setting, but also on biopsy material from another center and on nephrectomy specimens. Moreover, the study by Hermsen and colleagues is the only one to correlate results of the algorithm to expert pathologists’ assessment according to Banff categories for tubular damage and interstitial fibrosis. In another study by Jayapandian et al., albeit unrelated to the transplantation setting, the multicenter Nephrotic Syndrome Study Network (NEPTUNE) dataset of digitized renal biopsies was evaluated for the feasibility of deep learning approaches to automatically segment utilizing four stains [40]. Five nephropathologists were employed for annotations and 29 centers were enrolled to provide material whereby 20 deep-learning models were tested, making this work one of the most powered to date concerning kidney histology and AI. PAS proved to be the most suitable stain for computer-aided diagnosis and produced the highest concordance with expert evaluation for all the investigated structures, while silver-based stains yielded the worst results. Bouteldja et al. tested a CNN multiclass segmentation model on a large series of tissue specimens, derived from a plethora of animal models of various kidney diseases and a small subset of human tissue. All their preparations were PAS stained and six classes were tested: tubule, full glomerulus, glomerular tuft, artery (including intima and media, but excluding adventitia), arterial lumen, and vein. The best results in terms of average precision in detection was achieved for glomeruli, while accuracy for vascular structures was the lowest; moreover, performance on human tissue was intermediate. The authors also underscored the importance of training pathologists to ensure high quality annotations, and highlighted that good algorithm performance can be achieved with database heterogeneity, such as utilizing a variety of animal species and renal diseases [41].
It is noteworthy that all the included studies stressed the impact of their experimental setting: i.e., pre-implantation kidney biopsy stained only with PAS or H&E in the case of frozen sections, aiming to adhere as much as possible to the real-life practice of pathologists, with a subset aiming to use AI-aided evaluation of the Karpinski score [15,16,17]. Only one study explicitly compared the performance of the algorithm virtually, in terms of decision to discard a kidney with the cutoff of 20% glomerulosclerosis with the results of the on-call pathologists and the annotations made by expert pathologists [14], thus directly translating the deployment of the algorithm in clinical practice. However, all the other included studies recapitulate and discuss briefly the importance of an accurate and reliable evaluation of the single features of the kidney biopsy, its difficulties, the need for specific expertise and the relevant consequences in terms of erroneous discard. Nevertheless, despite the fact that deep-learning models are capable of excellent detection and classification of renal structures, for such an algorithm to be approved for clinical use it must first be tested and validated prior to clinical deployment. AI could become extremely helpful for practicing pathologists, especially given the projected decrease in the pathology workforce and continued demand for specialization [42]. All included studies also highlighted the need to adjust AI models to work with WSI, in anticipation of more pathology laboratories ultimately transitioning to a fully digital workflow.
Conclusion
Within the last decade many studies have been published testing AI algorithms developed for the detection and classification of elementary structures in kidney biopsy material. However, very few of these studies specifically designed AI-based models to optimize the evaluation of renal biopsies in the pre-implantation setting. It is foreseeable that in the near future more multicenter projects will provide additional contributions to the transplantation field. Closer cooperation between computer scientists and practicing as well as expert renal pathologists is needed, helping to refine the performance of AI-based models for routine pre-implantation kidney biopsy clinical practice.
Data availability
Not applicable.
Change history
16 July 2022
Missing Open Access funding information has been added in the Funding Note.
References
Becker JU, Mayerich D, Padmanabhan M et al (2020) Artificial intelligence and machine learning in nephropathology. Kidney Int 98:65–75. https://doi.org/10.1016/j.kint.2020.02.027
Liapis H, Gaut JP, Klein C et al (2017) Banff histopathological consensus criteria for preimplantation kidney biopsies. Am J Transplant 17:140–150. https://doi.org/10.1111/ajt.13929
Girolami I, Gambaro G, Ghimenton C et al (2020) Pre-implantation kidney biopsy: value of the expertise in determining histological score and comparison with the whole organ on a series of discarded kidneys. J Nephrol 33:167–176. https://doi.org/10.1007/s40620-019-00638-7
Antonieta Azancot M, Moreso F, Salcedo M et al (2014) The reproducibility and predictive value on outcome of renal biopsies from expanded criteria donors. Kidney Int 85:1161–1168. https://doi.org/10.1038/ki.2013.461
Barisoni L, Lafata KJ, Hewitt SM et al (2020) Digital pathology and computational image analysis in nephropathology. Nat Rev Nephrol 16:669–685. https://doi.org/10.1038/s41581-020-0321-6
Farris AB, Vizcarra J, Amgad M et al (2021) Artificial intelligence and algorithmic computational pathology: an introduction with renal allograft examples. Histopathology 78:791–804. https://doi.org/10.1111/his.14304
Girolami I, Parwani A, Barresi V et al (2019) The landscape of digital pathology in transplantation: from the beginning to the virtual E-slide. J Pathol Inform 10:21. https://doi.org/10.4103/jpi.jpi_27_19
Eccher A, Neil D, Ciangherotti A et al (2016) Digital reporting of whole-slide images is safe and suitable for assessing organ quality in preimplantation renal biopsies. Hum Pathol 47:115–120. https://doi.org/10.1016/j.humpath.2015.09.012
Eccher A, Girolami I, Brunelli M et al (2020) Digital pathology for second opinion consultation and donor assessment during organ procurement: Review of the literature and guidance for deployment in transplant practice. Transplant Rev 34:100562. https://doi.org/10.1016/j.trre.2020.100562
Neri F, Eccher A, Rigotti P et al (2021) Advantages of using a web-based digital platform for kidney preimplantation biopsies. J Pathol Inform 12:41. https://doi.org/10.4103/jpi.jpi_23_21
Cima L, Brunelli M, Parwani A et al (2018) Validation of remote digital frozen sections for cancer and transplant intraoperative services. J Pathol Inform 9:34. https://doi.org/10.4103/jpi.jpi_52_18
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev 5:210. https://doi.org/10.1186/s13643-016-0384-4
Marsh JN, Matlock MK, Kudose S et al (2018) Deep learning global glomerulosclerosis in transplant kidney frozen sections. IEEE Trans Med Imaging 37:2718–2728. https://doi.org/10.1109/TMI.2018.2851150
Marsh JN, Liu T-C, Wilson PC et al (2021) Development and validation of a deep learning model to quantify glomerulosclerosis in kidney biopsy specimens. JAMA Netw Open 4:e2030939. https://doi.org/10.1001/jamanetworkopen.2020.30939
Altini N, Cascarano GD, Brunetti A et al (2020) Semantic segmentation framework for glomeruli detection and classification in kidney histological sections. Electronics 9:503. https://doi.org/10.3390/electronics9030503
Bevilacqua V, Pietroleonardo N, Triggiani V et al (2017) An innovative neural network framework to classify blood vessels and tubules based on Haralick features evaluated in histological images of kidney biopsy. Neurocomputing 228:143–153. https://doi.org/10.1016/j.neucom.2016.09.091
Cascarano GD, Debitonto FS, Lemma R, et al (2019) An Innovative Neural Network Framework for Glomerulus Classification Based on Morphological and Texture Features Evaluated in Histological Images of Kidney Biopsy. pp 727–738
Salvi M, Mogetta A, Meiburger KM et al (2020) Karpinski score under digital investigation: a fully automated segmentation algorithm to identify vascular and stromal injury of Donors’ Kidneys. Electronics 9:1644. https://doi.org/10.3390/electronics9101644
Salvi M, Mogetta A, Gambella A et al (2021) Automated assessment of glomerulosclerosis and tubular atrophy using deep learning. Comput Med Imaging Graph Off J Comput Med Imaging Soc 90:101930. https://doi.org/10.1016/j.compmedimag.2021.101930
Badrinarayanan V, Kendall A, Cipolla R (2017) SegNet: a deep convolutional encoder-decoder architecture for image segmentation. IEEE Trans Pattern Anal Mach Intell 39:2481–2495. https://doi.org/10.1109/TPAMI.2016.2644615
Chen L-C, Zhu Y, Papandreou G et al (2018) Encoder-decoder with atrous separable convolution for semantic image segmentation. In: Ferrari V, Hebert M, Sminchisescu C, Weiss Y (eds) Computer vision—ECCV 2018. Springer International Publishing, Cham, pp 833–851
Ronneberger O, Fischer P, Brox T (2015) U-net: convolutional networks for biomedical image segmentation. In: Navab N, Hornegger J, Wells WM, Frangi AF (eds) Medical image computing and computer-assisted intervention—MICCAI 2015. Springer International Publishing, Cham, pp 234–241
Karpinski J, Lajoie G, Cattran D et al (1999) Outcome of kidney transplantation from high-risk donors is determined by both structure and function. Transplantation 67:1162–1167. https://doi.org/10.1097/00007890-199904270-00013
Remuzzi G, Cravedi P, Perna A et al (2006) Long-term outcome of renal transplantation from older donors. N Engl J Med 354:343–352. https://doi.org/10.1056/NEJMoa052891
Bukowy JD, Dayton A, Cloutier D et al (2018) Region-based convolutional neural nets for localization of glomeruli in trichrome-stained whole kidney sections. J Am Soc Nephrol 29:2081–2088. https://doi.org/10.1681/ASN.2017111210
Gadermayr M, Eschweiler D, Jeevanesan A et al (2017) Segmenting renal whole slide images virtually without training data. Comput Biol Med 90:88–97. https://doi.org/10.1016/j.compbiomed.2017.09.014
Ginley B, Tomaszewski JE, Yacoub R et al (2017) Unsupervised labeling of glomerular boundaries using Gabor filters and statistical testing in renal histology. J Med Imaging 4:021102. https://doi.org/10.1117/1.JMI.4.2.021102
Ginley B, Lutnick B, Jen K-Y et al (2019) Computational segmentation and classification of diabetic glomerulosclerosis. J Am Soc Nephrol 30:1953–1967. https://doi.org/10.1681/ASN.2018121259
Lutnick B, Ginley B, Govind D et al (2019) An integrated iterative annotation technique for easing neural network training in medical image analysis. Nat Mach Intell 1:112–119. https://doi.org/10.1038/s42256-019-0018-3
Kato T, Relator R, Ngouv H et al (2015) Segmental HOG: new descriptor for glomerulus detection in kidney microscopy image. BMC Bioinform 16:316. https://doi.org/10.1186/s12859-015-0739-1
Sarder P, Ginley B, Tomaszewski JE (2016) Automated renal histopathology: digital extraction and quantification of renal pathology. Proc. SPIE 9791, Medical Imaging 2016: Digital Pathology, 97910F. https://doi.org/10.1117/12.2217329
Simon O, Yacoub R, Jain S et al (2018) Multi-radial LBP features as a tool for rapid glomerular detection and assessment in whole slide histopathology images. Sci Rep 8:2032. https://doi.org/10.1038/s41598-018-20453-7
Zhao Y, Black EF, Marini L, et al (2016) Automatic glomerulus extraction in whole slide images towards computer aided diagnosis. In: 2016 IEEE 12th International Conference on e-Science (e-Science). IEEE, pp 165–174
Bueno G, Fernandez-Carrobles MM, Gonzalez-Lopez L, Deniz O (2020) Glomerulosclerosis identification in whole slide images using semantic segmentation. Comput Methods Programs Biomed 184:105273. https://doi.org/10.1016/j.cmpb.2019.105273
Gallego J, Pedraza A, Lopez S et al (2018) Glomerulus classification and detection based on convolutional neural networks. J Imaging 4:20. https://doi.org/10.3390/jimaging4010020
Kawazoe Y, Shimamoto K, Yamaguchi R et al (2018) Faster R-CNN-based glomerular detection in multistained human whole slide images. J Imaging 4:91. https://doi.org/10.3390/jimaging4070091
Maree R, Dallongeville S, Olivo-Marin J-C, Meas-Yedid V (2016) An approach for detection of glomeruli in multisite digital pathology. In: 2016 IEEE 13th International Symposium on Biomedical Imaging (ISBI). IEEE, pp 1033–1036
Temerinac-Ott M, Forestier G, Schmitz J, et al (2017) Detection of glomeruli in renal pathology by mutual comparison of multiple staining modalities. In: Proceedings of the 10th International Symposium on Image and Signal Processing and Analysis. IEEE, pp 19–24
Hermsen M, de Bel T, den Boer M et al (2019) Deep learning-based histopathologic assessment of kidney tissue. J Am Soc Nephrol 30:1968–1979. https://doi.org/10.1681/ASN.2019020144
Jayapandian CP, Chen Y, Janowczyk AR et al (2021) Development and evaluation of deep learning–based segmentation of histologic structures in the kidney cortex with multiple histologic stains. Kidney Int 99:86–101. https://doi.org/10.1016/j.kint.2020.07.044
Bouteldja N, Klinkhammer BM, Bülow RD et al (2021) Deep learning-based segmentation and quantification in experimental kidney histopathology. J Am Soc Nephrol 32:52–68. https://doi.org/10.1681/ASN.2020050597
Robboy SJ, Weintraub S, Horvath AE et al (2013) Pathologist workforce in the United States: I. Development of a predictive model to examine factors influencing supply. Arch Pathol Lab Med 137:1723–1732. https://doi.org/10.5858/arpa.2013-0200-OA
Funding
Open access funding provided by Università degli Studi di Verona within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
No ethical issues are raised by systematic reviews.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Girolami, I., Pantanowitz, L., Marletta, S. et al. Artificial intelligence applications for pre-implantation kidney biopsy pathology practice: a systematic review. J Nephrol 35, 1801–1808 (2022). https://doi.org/10.1007/s40620-022-01327-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-022-01327-8