Abstract
Background
Familial hypomagnesemia with hypercalciuria and nephrocalcinosis (FHHNC) is a rare tubulopathy caused by mutations in the CLDN16 or CLDN19 genes. Patients usually develop hypomagnesemia, hypercalciuria, nephrocalcinosis and renal failure early in life. Patients with CLDN19 mutations may also have ocular abnormalities. Despite clinical variability, factors associated with kidney function impairment, especially in patients with CLDN19 mutations, have not been addressed.
Methods
Retrospective multicenter study of 30 genetically confirmed FHHNC Spanish patients. We analyzed kidney function impairment considering as outcomes chronic kidney disease (CKD) stage 3 and annual estimated glomerular filtration rate (eGFR) decline, to identify factors associated with the different phenotypes.
Results
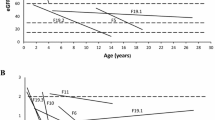
Of thirty patients, 27 had mutations in the CLDN19 gene (20 homozygous for the p.G20D mutation) and 3 in the CLDN16. Age at diagnosis was 1.71 (0.67–6.04) years and follow-up time was 8.34 ± 4.30 years. No differences in CKD stage 3-free survival based on CLDN19 mutation (p.G20D homozygous vs. other mutations) or gender were found, although females seemed to progress faster than males. Patients with more pronounced eGFR decline had higher PTH levels at diagnosis than those with stable kidney function, despite similar initial eGFR. Approximately 60% of CLDN19 patients presented ocular abnormalities. Furthermore, we confirmed high phenotypic intrafamilial variability.
Conclusions
In a contemporary cohort of FHHNC patients with CLDN19 mutations, females seemed to progress to CKD-stage 3 faster than males. Increased PTH levels at baseline may indicate a more severe renal course. There was high phenotype variability among patients with CLDN19 mutations and kidney function impairment differed even between siblings.
Graphical abstract





Similar content being viewed by others
References
Praga M, Vara J, González-Parra E et al (1995) Familial hypomagnesemia with hypercalciuria and nephrocalcinosis. Kidney Int 47:1419–1425. https://doi.org/10.1038/ki.1995.199
Simon DB, Lu Y, Choate KA et al (1999) Paracellin-1, a renal tight junction protein required for paracellular Mg2+ resorption. Science (80-) 285:103–106. https://doi.org/10.1126/science.285.5424.103
Konrad M, Seelow D, Pandey AV et al (2006) Mutations in the tight-junction gene Claudin 19 (CLDN19) are associated with renal magnesium wasting, renal failure, and severe ocular involvement. Am J Hum Genet 79:949–957
Hou J, Renigunta A, Konrad M et al (2008) Claudin-16 and claudin-19 interact and form a cation-selective tight junction complex. J Clin Invest 118:619–628. https://doi.org/10.1172/JCI33970
Ariceta G, Vallo A, Rodriguez-Soriano J (2004) Acidosis increases magnesiuria in children with distal renal tubular acidosis. Pediatr Nephrol 19:1367–1370. https://doi.org/10.1007/s00467-004-1609-7
Claverie-Martín F, García-Nieto V, Loris Pablo C et al (2013) Claudin-19 mutations and clinical phenotype in spanish patients with familial hypomagnesemia with hypercalciuria and nephrocalcinosis. PLoS ONE 8:e53151. https://doi.org/10.1371/journal.pone.0053151
Weber S, Hoffmann K, Jeck N et al (2000) Familial hypomagnesaemia with hypercalciuria and nephrocalcinosis maps to chromosome 3q27 and is associated with mutations in the PCLN-1 gene. Eur J Hum Genet 8:414–422. https://doi.org/10.1038/sj.ejhg.5200475
Sikora P, Zaniew M, Haisch L et al (2015) Retrospective cohort study of familial hypomagnesaemia with hypercalciuria and nephrocalcinosis due to CLDN16 mutations. Nephrol Dial Transpl 30:636–644. https://doi.org/10.1093/ndt/gfu374
Weber S, Schneider L, Peters M et al (2001) Novel paracellin-1 mutations in 25 families with familial hypomagnesemia with hypercalciuria and nephrocalcinosis. J Am Soc Nephrol 12:1872–1881
Stenson PD, Mort M, Ball EV et al (2017) The Human Gene Mutation Database: towards a comprehensive repository of inherited mutation data for medical research, genetic diagnosis and next-generation sequencing studies. Hum Genet 136:665–677. https://doi.org/10.1007/s00439-017-1779-6
Konrad M, Hou J, Weber S et al (2008) CLDN16 genotype predicts renal decline in familial hypomagnesemia with hypercalciuria and nephrocalcinosis. J Am Soc Nephrol 19:171–181. https://doi.org/10.1681/ASN.2007060709
Faguer S, Chauveau D, Cintas P et al (2011) Renal, ocular, and neuromuscular involvements in patients with CLDN19 mutations. J Am Soc Nephrol 6:355–360. https://doi.org/10.2215/CJN.02870310
Seeley HH, Loomba-Albrecht LA, Nagel M et al (2012) Familial hypomagnesemia with hypercalciuria and nephrocalcinosis in three siblings having the same genetic lesion but different clinical presentations. World J Pediatr 8:177–180. https://doi.org/10.1007/s12519-011-0295-3
Müller D, Kausalya PJ, Bockenhauer D et al (2006) Unusual clinical presentation and possible rescue of a novel claudin-16 mutation. J Clin Endocrinol Metab 91:3076–3079. https://doi.org/10.1210/jc.2006-0200
Arteaga ME, Hunziker W, Teo ASM et al (2015) Familial hypomagnesemia with hypercalciuria and nephrocalcinosis: variable phenotypic expression in three affected sisters from Mexican ancestry. Ren Fail 37:180–183. https://doi.org/10.3109/0886022X.2014.977141
Godron A, Harambat J, Boccio V et al (2012) Familial hypomagnesemia with hypercalciuria and nephrocalcinosis: phenotype-genotype correlation and outcome in 32 patients with CLDN16 or CLDN19 mutations. Clin J Am Soc Nephrol 7:801–809. https://doi.org/10.2215/CJN.12841211
Al-shibli A, Konrad M, Altay W et al (2013) Familial hypomagnesemia with hypercalciuria and nephrocalcinosis (FHHNC): report of three cases with a novel mutation in CLDN19 gene. Saudi J Kidney Dis Transpl 24:338–344
Sharma S, Place E, Lord K et al (2016) Claudin 19-based familial hypomagnesemia with hypercalciuria and nephrocalcinosis in a sibling pair. Clin Nephrol 85(2016):346–352. https://doi.org/10.5414/CN108783
Perdomo-Ramirez A, Aguirre M, Davitaia T et al (2019) Characterization of two novel mutations in the claudin-16 and claudin-19 genes that cause familial hypomagnesemia with hypercalciuria and nephrocalcinosis. Gene 689:227–234. https://doi.org/10.1016/j.gene.2018.12.024
Mejía N, Santos F, Claverie-Martín F et al (2013) RenalTube: a network tool for clinical and genetic diagnosis of primary tubulopathies. Eur J Pediatr 172:775–780. https://doi.org/10.1007/s00431-013-1934-6
Carrascosa Lezcano A, Fernández García JM, Fernández Ramos C et al (2008) Estudio transversal español de crecimiento 2008. Parte II: Valores de talla, peso e índice de masa corporal desde el nacimiento a la talla adulta. An Pediatría 68:552–569
Schwartz GJ, Muñoz A, Schneider MF et al (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637. https://doi.org/10.1681/ASN.2008030287
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Müller D, Kausalya PJ, Claverie-Martin F et al (2003) A novel claudin 16 mutation associated with childhood hypercalciuria abolishes binding to ZO-1 and results in lysosomal mistargeting. Am J Hum Genet 73:1293–1301. https://doi.org/10.1086/380418
Ariceta G, Rodriguez-Soriano J, Vallo A (1996) Renal magnesium handling in infants and children. Acta Paediatr Int J Paediatr 85:1019–1023. https://doi.org/10.1111/j.1651-2227.1996.tb14209.x
Michelis MF, Drash AL, Linarelli LG et al (1972) Decreased bicarbonate threshold and renal magnesium wasting in a sibship with distal renal tubular acidosis. Metabolism 21:905–920. https://doi.org/10.1016/0026-0495(72)90025-X
Yuan T, Pang Q, Xing X et al (2015) First report of a novel missense CLDN19 mutations causing familial hypomagnesemia with hypercalciuria and nephrocalcinosis in a Chinese family. Calcif Tissue Int 96:265–273. https://doi.org/10.1007/s00223-014-9951-7
Espinosa Román L (2017) Valoración de la función renal. Pediatr Integr 21:549–555
de Kieviet W, Slaats EH, Abeling NG (1986) Pediatric reference values for calcium, magnesium and inorganic phosphorus in serum obtained from Bhattacharya plots for data from unselected patients. J Clin Chem Clin Biochem 24:233–242. https://doi.org/10.1515/cclm.1986.24.4.233
Haisch L, Almeida JR, Abreu Da Silva PR et al (2011) The role of tight junctions in paracellular ion transport in the renal tubule: lessons learned from a rare inherited tubular disorder. Am J Kidney Dis 57:320–330. https://doi.org/10.1053/j.ajkd.2010.08.038
Acknowledgements
This study could not have been done without the collaboration of patients and families, the FHHNC patient advocacy group HIPOFAM (http://hipofam.org) and the Renaltube group (http://renaltube.com). We are also grateful to the physicians for their cooperation: Marisa Justa and Belen Campos (Pediatric Nephrology, and Nephrology. Hospital Infantil Miguel Servet. Zaragoza), Mireia Aguirre, María Herrero and Leire Madariaga (Pediatric Nephrology. Hospital Universitario Cruces. Bizkaia), Carmen de Lucas and Cristina Aparicio (Pediatric Nephrology. Hospital Infantil Universitario Niño Jesús. Madrid), Javier Lumbreras (Pediatric Nephrology. Hospital Universitari Son Espases. Palma de Mallorca), Ainhoa Iceta (Pediatric Nephrology. Hospital Virgen del Camino. Pamplona), Inés Vergara (Pediatric Nephrology. Complexo Hospitalario Universitario A Coruña), Ana Sánchez (Pediatric Nephrology. Hospital Universitario Virgen del Rocío. Sevilla), Marta Melgosa (Pediatric Nephrology. Hospital Infantil La Paz. Madrid), Santiago Rodríguez (Pediatric Nephrology. Hospital de Terrassa), Ana Ruiz (Pediatric Nephrology. Hospital Universitario Torrecárdenas), Juan David González (Pediatric Nephrology. Hospital General Universitario Santa Lucía. Cartagena), Montse Antón (Pediatric Nephrology. Hospital Universitario Reina Sofía de Córdoba), Jonay Pantoja (Nephrology. Hospital Universitari Doctor Peset de Valencia), Manel Perelló (Pediatric Nephrology. Hospital Universitari Vall d’Hebron. Barcelona), Ramón Saracho (Pediatric Nephrology. Hospital Universitario de Álava. Vitoria-Gazteiz), Rebeca Garrote (Pediatric Nephrology. Hospital Clínico Universitario de Valladolid) and Francisco Aguilar (Pediatric Nephrology. Hospital General de Valencia).
Funding
Research grants from Fondo de Investigación Sanitaria (PI14/01107 and PI18/01107) and HIPOFAM contribution supported this work. FCM was supported by grant PI17/00153 co-financed by the ISCIII-Subdirección General de Evaluación y Fomento de la Investigación and the European Regional Development Fund “Another way to build Europe”.
Author information
Authors and Affiliations
Contributions
MV-P and CB contributed equally in research design, research performance, data analysis and writing of the manuscript. FC-M participated in the diagnosis of patients and writing of the manuscript. AM participated in research design, data analysis and writing of the manuscript. GA participated in research design, research performance, data analysis and writing of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Vall d’Hebron Hospital [Date 01.04.201/No. (PR(AMI)280/2015)].
Informed consent
All patients, or their caregivers, provided written informed consent before participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vall-Palomar, M., Burballa, C., Claverie-Martín, F. et al. Heterogeneity is a common ground in familial hypomagnesemia with hypercalciuria and nephrocalcinosis caused by CLDN19 gene mutations. J Nephrol 34, 2053–2062 (2021). https://doi.org/10.1007/s40620-021-01054-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-021-01054-6