Abstract
Background
In February 2020 the corona virus disease 2019 (COVID-19) infection started spreading throughout Italy, hitting the Lombardy region very hard. Despite the high diffusion, only a subset of patients developed severe COVID-19: around 25% of them developed acute kidney injury (AKI) and one-third of them died. Elderly patients and patients with high comorbidities were identified as being at higher risk of severe COVID-19.
Methods
Our prospective observational cohort study includes 392 consecutive patients hospitalized for COVID-19 in Milan (median age 67 years, 75% male). We evaluated the relationship between blood pressure at presentation, presence of AKI at Emergency Department admission and during hospitalization, and total in-hospital mortality (24%).
Results
Although 58% of our study patients reported a history of hypertension (HYP) (86% on treatment), 30% presented with low blood pressure levels. Only 5.5% were diagnosed with AKI on admission; 75% of hypertensive patients discontinued therapy during hospitalization (only 20% were on treatment at discharge). Gender and hypertension were strongly associated with AKI at admission (odds ratio 11). Blood pressure was inversely correlated with increased risk of AKI upon admission, regardless of the severity of respiratory distress. Age over 65, history of hypertension, and severity of respiratory distress were the main predictors of AKI, which developed in 34.7% of cases during hospitalization. AKI was associated with increased in-hospital mortality. Hypertension and low blood pressure at presentation were the main predictors of in-hospital mortality, together with age over 65, baseline pulmonary involvement, and severity of illness.
Conclusions
In patients hospitalized for COVID-19, hypertension and low blood pressure at presentation are important risk factors for AKI and mortality. Early reduction of antihypertensive therapy may improve outcomes in patients with SARS-CoV-2 infection.
Similar content being viewed by others
Introduction
On February 20th, 2020 the first patient diagnosed with the novel Coronavirus disease 2019 (COVID-19) developed respiratory failure and was admitted to the Intensive Care Unit in Lombardy [1]. The COVID-19 infection then spread across the whole of Lombardy and Italy and became the most serious public health threat in the world. Evidence collected since the beginning of the COVID-19 outbreak has shown that only a subset of patients will develop severe disorders after COVID-19, while the majority of subjects exhibit weak respiratory symptoms or remain asymptomatic. Severe COVID-19 is characterized by a potent cytokine storm that can damage several organs, mainly the lungs but also the liver, central and peripheral nervous system, heart and kidneys [2,3,4,5], and causes high mortality [6]. This hyperinflammatory syndrome is accompanied by massive coagulation resulting in multiorgan failure. Early identification of patients at high risk of developing severe COVID-19 and initiation of timely treatment are mandatory to reduce mortality. Respiratory failure from acute respiratory distress syndrome (ARDS) is the leading cause of mortality; management is currently supportive, although recent improvements in our treatment strategies have been made [7]. In addition to respiratory failure, COVID-19 patients may eventually die of multiple organ failure, shock, heart failure, arrhythmia, and acute kidney injury (AKI).
The complex organ derangement occurring in patients with COVID-19 may worsen their original comorbidities which need to be accurately evaluated, especially in older patients who may have serious comorbid conditions. In a large cohort of patients of Caucasian origin followed-up at a single University hospital in the north of Italy, we recently showed that older age and hypertension (HYP), as well as biomarkers of systemic hyperinflammation, are predictors of early death [8]. Arterial hypertension is one of the most common comorbidities associated with COVID-19, especially in patients with severe clinical involvement and at risk of death [2, 9, 10]. The association between hypertension and early death may be sustained by the interaction of the SARS-CoV-2 virus with ACE2 which is the port of entry into host cells. ACE2 is expressed in endothelial lung and kidney cells [11]. It exerts a substantial anti-inflammatory activity and antagonizes the renin–angiotensin–aldosterone pathway [12]. The interaction with SARS-CoV-2 may alter the ACE2 vasodilating activity and the homeostasis of the renin–angiotensin–aldosterone system (RAAS). Greater expression of ACE2 predisposes to a higher incidence of COVID-19 but with lower severity (as observed in younger patients), whereas subjects with lower ACE2 develop more severe disease. Lower ACE2 levels and upregulation of proinflammatory Angiotensin II predispose elderly patients with cardiovascular diseases to greater COVID-19 severity and mortality [13].
In COVID-19 patients with respiratory failure undergoing mechanical ventilation [14], AKI is the most frequent and severe non-pulmonary complication. Around 25% of COVID-19 patients develop AKI and one-third of them die [15]. Histological examination of the kidneys of COVID-19 patients showed both tubular and glomerular involvement (ranging from tubular necrosis to glomerular collapse associated with fibrin thrombus deposition in glomerular and peritubular capillaries) despite normal kidney function. SARS-CoV-2 tropism for the kidney is still under debate [5, 16, 17]. In COVID-19 patients, AKI may result from microvascular and immunological injuries, non-viral toxic and hemodynamic factors induced by sepsis, and cytokine storm.
In the present study, we further highlight the relevance of hypertension and kidney function on clinical outcomes in our cohort of COVID-19 patients. The patients’ characteristics upon admission to the emergency department (ED) and during hospitalization were analyzed separately to identify features associated with critical illness and worse prognosis.
Materials and methods
Study design and participants
This is a retrospective and prospective cohort study included in an extensive single-center observational investigation, the COVID-BioB study, implemented at the (IRCCS) San Raffaele Scientific Institute in Milan, Italy. The study is retrospective concerning comorbidity and basal renal function but is prospective concerning mortality and AKI development.
All patients aged 18 years or older, admitted to the IRCCS San Raffaele Scientific Institute from 25th February to April 25th, 2020, with confirmed SARS-CoV-2 infection were consecutively enrolled in the COVID-BioB study. Confirmed infection was defined as positive real-time reverse-transcriptase polymerase chain reaction (RT-PCR) from a nasopharyngeal and/or throat swab. All adult patients with clinical and radiologic findings suggestive of COVID-19 pneumonia and with plasma creatinine measured at least once during SARS-CoV-2 infection, were included in the present study (n = 392, M/F 293/99). The in-hospital mortality was analyzed in the whole patient cohort. After the exclusion of patients undergoing chronic dialysis and patients with only one measurement of serum creatinine, 380 subjects were analyzed for the AKI outcome.
The study was approved by the Hospital Ethics Committee (protocol no. 34/int/2020) and was registered on ClinicalTrials.gov (NCT04318366).
Written informed consent was obtained before data collection from patients able to provide signed informed consent at the time of hospital admission. Otherwise, patients consented as soon as they were able to sign. This study is reported in compliance with the STROBE statement.
Full description of patient management as well as clinical protocols were previously published [18, 19].
Outcomes
The main outcomes were the presence of AKI at admission to the Emergency Department, AKI development during hospitalization, and in-hospital death. Follow-up time was right-censored on April 25th, 2020.
Data collection and definitions
Data were collected by reviewing the medical charts or directly from interviews with the patients and entered into a dedicated COVID-BioB study electronic case record form (eCRF). Baseline serum creatinine was defined as the most recent creatinine value measured in the previous six months in stable clinical conditions if available (21%), or the last available value prior to discharge. The lowest creatinine value measured during hospitalization was selected as the baseline renal function for patients who died during the study. We considered two different forms of AKI: the presence of AKI on the day of Emergency Department admission and the development of AKI during hospitalization. AKI was defined as a 50% increase in serum creatinine from baseline according to the KDIGO criteria [20]. For patients with AKI at presentation, we compared the basal value with the first available creatinine value following Emergency Department admission; AKI during hospitalization was defined as the earliest serum creatinine change during hospitalization meeting KDIGO criteria.
SpO2/FiO2 was used as an indicator of the severity of respiratory distress; SpO2/FiO2 was divided into 4 classes as defined by SOFA score [21, 22]. See Supplementary materials for details.
Statistical analysis
Continuous variables were expressed as means and standard deviations (SD) for normally distributed continuous measures, medians and interquartile ranges (IQR) for skewed continuous measures. Categorical variables were summarized as counts and percentages; X2 or Fisher’s exact test was performed for comparison, as appropriate.
For mortality analysis, we created Kaplan–Meier cumulative incidence plots. We estimated hazard ratio (HR) for death using the Cox proportional hazards model; time-to-event was expressed in days from the date of hospital admission to the date of in-hospital death.
To investigate the relationship between SARS-CoV-2 infection, blood pressure dysregulation, kidney damage and mortality rate, a multivariable Cox regression model with eleven variables was performed.
To identify risk factors associated with the development of AKI (both AKI at presentation in the Emergency Department and AKI during hospitalization), we performed a logistic regression analysis using a stepwise procedure, with odds ratio (OR) estimation. All analyses were carried out using SPSS (version 24; IBM corporation). See supplementary materials for more details.
Results
Baseline characteristics
A total of 392 consecutive patients were included in our study. Table 1 shows the clinical and laboratory features of patients with SARS-CoV-2 infection.
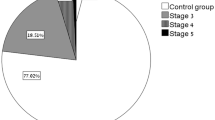
The median age was 67 years (range 28–94 years, mean age 65.6 years), 52.8% were older than 65 years, and 74.7% of patients were male; 30.4% of patients had eGFR < 60 ml/min/1.73 m2 (equal to CKD stage 3 or greater). The main comorbidity of SARS-CoV-2 infection was hypertension (58.3%); 86.3% of hypertensive subjects were on antihypertensive medication at Emergency Department admission (see Table 2 for details). Analyses of blood pressure values at presentation showed that systolic blood pressure (SBP) was slightly higher in hypertensive patients than in those without HYP, whereas diastolic blood pressure (DBP) and mean blood pressure (MBP) were similar in these patient groups. Other comorbidities included coronary artery disease [(CAD), 27%], diabetes [(DM), 17.8%] and chronic obstructive pulmonary disease [(COPD), 7.3%]. Fourteen point two% of patients presented with malignancy [neoplasm (NPL)]. Laboratory parameters and severity of respiratory distress at admission are listed in Table 1.
Surprisingly, considering the rate of HYP, only 4.6% of patients presented uncontrolled BP (defined as MBP > 110 mmHg) at admission; on the other hand, more than 30% of subjects presented low BP levels (MBP < 86 mmHg). Frank hemodynamic shock (defined as MBP < 65 mmHg) was observed in only 1.9% of patients.
The median in-hospital stay was 10 days (interquartile range, 6–15 days). The main outcomes (Table 2) we evaluated were total in-hospital mortality rate (24.2%; median time to death was 8 days [range (or interquartile range) 4–13 days]) and development of AKI (35.3%).
Presence of acute kidney injury at Emergency Department admission
AKI was already present in 5.5% of patients at Emergency Department admission. HYP and gender were associated with AKI at presentation in the Emergency Department in a stepwise conditional logistic regression analysis (Supplementary table 1a and 1b). Indeed, the incidence of cases with AKI at presentation in the Emergency Department was 7.5% in patients with HYP vs 0.6% in non-HYP subjects (Fisher test p = 0.002), thus showing a 10-fold increased risk (OR 10.72; 95% CI 1.19–97.73, logistic regression p-value = 0.03) after adjustment for independent covariates, including respiratory distress (RD).
It was also observed that MBP levels at presentation (ED-MBP) were inversely related to an increased risk of the presence of AKI at Emergency Department admission (logistic regression p-value = 0.014). A stand-alone level of MBP < 83 mmHg (1° quartile of ED-MBP distribution) or MBP < 65 mmHg (hemodynamic shock) at presentation were associated with a threefold (OR 3.18; 95%CI 1.21–8.38, p = 0.014) or tenfold (OR 10.62; 95%CI 1.81–62.37; p = 0.001) increased risk of the simultaneous presence of AKI, respectively. Nevertheless, no relationship between blood pressure and the severity of illness was observed (Pearson Correlation r = 0.039; p = 0.48).
In-hospital acute kidney injury development
During hospitalization AKI occurred in 34.7% of patients; the median time to in-hospital AKI development was 7 days (IQR 3–12 days). High incidence of both proteinuria (57.5%) and hematuria (45.5%) were also observed although no significant relationship was found with the development of AKI (Table 2).
The incidence of in-hospital AKI was significantly higher in elderly patients (age > 65 years 44.7% vs 24.0%; X2 17.80; p < 0.001) and among patients with HYP (43.7% vs 20.8%; X2 21.33; p < 0.001). Logistic regression analysis showed that age over 65 yrs, HYP and RD were the main risk factors for in-hospital AKI development (Supplementary table 2a and 2b). Chronic therapy with diuretics (49.8% of patients) or anti-hypertensive drugs (and in particular RAAS inhibitors) was not associated with an increase in AKI development during hospitalization, however, pharmacological treatment was discontinued in 75.4% of hypertensive patients. Indeed, only 20.8% of hypertensive patients were still being treated at discharge (Supplementary table 4; Fig. 1).
In-hospital death
The presence of AKI, be it already present at admission to the Emergency Department or developing during hospitalization, increased the risk of death (HR 2.25; 95%CI 1.20–4.25 and OR 2.11; 95%CI 1.34–3.34, respectively), as shown in Fig. 2.
As expected in a viral respiratory disease, the severity of respiratory distress and COPD are relevant determinants of mortality. Interestingly, other factors, such as baseline kidney function and MBP at admission, were associated with an increased mortality rate in univariate analysis (see Supplementary table 3). In detail, a significantly higher mortality rate was observed in subjects with HYP, and in particular in elderly patients (44.4% in elderly patients with HYP compared to 14.1% in younger patients with HYP; X2 38.82; p < 0.001) and in patients with CKD stage 3 or greater (47.9% in CKD compared to 13.9% in non-CKD; X2 52.11; p < 0.001).
Finally, we observed a negative relationship between MBP levels at admission and mortality (logistic regression p = 0.021). Through the calculation of Youden Index [23], MBP 86 mmHg (i.e., 120/70 mmHg) was identified as the best cut-off for optimal in-hospital death risk assessment (OR 2.08; 95%CI 1.25–3.45). However, as shown in Table 3, taken together, only age (> 65 years), COPD, HYP, MBP at presentation < 86 mmHg and severity of illness were independently associated with total in-hospital mortality.
Discussion
Coronavirus disease 2019 is a highly contagious viral disease causing severe acute respiratory distress syndrome. In this study, we investigated the relationship between blood pressure, kidney function and in-hospital mortality in 392 Italian COVID-19 patients.
In our cohort, mortality was higher than in similar COVID-19 cohorts due to the characteristics of our hospital and the policy of hospital admission during the pandemic (including the transfer of the most critically ill patients from other hospitals) [23].
As has recently emerged in other studies, COVID-19 is not only a viral respiratory disease, but it often involves different organs with a variable presentation of the disease [2, 3]. In particular, our work has shown evidence of an important role of both the hemodynamic response to SARS-Cov-2 infection and the patient’s medical history on AKI development and patient mortality. The main results suggest that history of hypertension, CKD and presentation to the ED with low blood pressure are important risk factors for AKI. Furthermore, they play an important role in mortality in patients with COVID-19. Indeed, gender and HYP were the main predictors of the presence of AKI at Emergency Department admission; moreover, a stand-alone level of MBP < 83 mmHg at Emergency Department admission (i.e., < 120/70 mmHg) is independently associated with an increased risk of the simultaneous presence of AKI. Similarly, these factors impact in-hospital mortality. In a model of univariate Cox regression, HYP, CKD, MBP < 86 mmHg at Emergency Department admission, and severity of illness were independently associated with a two-fold increase in overall mortality.
Surprisingly, hospital-acquired AKI did not prove to be a significant predictor of mortality in the multivariable Cox model. The absence of relationship is likely due to the simultaneous presence of clinical conditions at baseline, related to age, comorbidities (older age, arterial hypertension, cardiovascular diseases) and severity of COVID-19 disease (i.e., respiratory distress) that lead to the increased risk of AKI and death at the same time. Another explanation could be the possible lack of statistical power due to the limited number of deaths in this specific subset of cases (95 patients).
We analyzed AKI development both at Emergency Department admission and during hospitalization. We can speculate that the main difference in terms of pathophysiology between patients with AKI at Emergency Department presentation and those with in-hospital AKI development is that in the former case AKI is presumably a hemodynamic consequence of SARS-CoV-2 infection, whereas hospital-acquired AKI could be a multifactorial disorder with multiple mechanisms of development, including pharmacological treatments. Respiratory distress is a major determinant of in-hospital AKI most likely because of the more aggressive therapy critically ill patients undergo; on the other hand, low MBP at presentation directly affects kidney function thus leading to the development of AKI at Emergency Department admission. The association between BP and AKI does not appear to be the result of the severity of the clinical picture but suggests dysregulation of BP control and possibly of vascular tone in patients with COVID-19.
Unlike what occurs in systemic bacterial infections, the hemodynamic effect of SARS-CoV-2 infection seems to be independent of the severity of the disease. Indeed, we observed no relationship between the severity of respiratory distress, grade of hypoxia and low MBP in the Emergency Department. We may assume that the negative hemodynamic effect of SARS-CoV-2 infection was not mediated by the classical septic shock pathways alone, but that it was also a consequence of neurovegetative alterations. The effect on vascular resistance control mediated by its interaction with ACE2, which is a SARS-Cov-2 receptor, may be a potential mechanism of the hemodynamic effect of SARS-Cov-2 infection, even though no data have been collected to support this hypothesis.
Since 75.4% of hypertensive patients have to discontinue pharmacological treatment due to low BP levels, these findings suggest that early intervention is required at COVID-19 onset so as to prevent the negative hemodynamic impact. In this subset of patients, early discontinuation of any anti-hypertensive treatment could lead to better presentation at the Emergency Department resulting in an improvement in the clinical course of the disease. As our results suggest, this evidence is independent of the respiratory impact of COVID-19 and so this medical approach should be applied to any patients with or without severe respiratory distress.
In conclusion, on the basis of these data we would recommend including an evaluation of blood pressure values and kidney function at presentation of all patients with SARS-Cov-2, in association with the anamnestic history of hypertension and CKD (Fig. 3). Early reduction of antihypertensive therapy if blood pressure is lower than 120/70 may decrease AKI development and mortality in COVID-19.
This study has several limitations. First, our study was carried out in a single large hospital in Milan, thus potentially limiting generalizability to hospital settings elsewhere in Italy. Second, our analyses incorporated outcome data collected until April 25th, 2020. Vital status and hospital-acquired AKI are not yet known for patients who remained hospitalized after this date. Third, patients presented to the hospital at varying time points of their disease course, and time from symptom onset to hospital presentation was not available. Indeed, our analysis included the severity of illness at Emergency Department admission. Fourth, we did not analyze biomarkers because they are only available for a small group of patients and because we focused our analysis on blood pressure and kidney function. Fifth, complete urinalysis was available for only 24% of patients because, considering the presence of severe respiratory disease, it was not of primary importance and urinary sediment could not be examined. Moreover, information regarding the presence of urinary catheter was not available thereby affecting the reliability of the hematuria data.
This study also has many strengths. First, our study represents one of the largest nephrological focuses on patients with COVID-19 in Lombardy, the hardest hit region in Italy. Second, we prospectively identified patients and collected data from the beginning of the pandemic. Third, we collected data using a case record form completed with laboratory data which were available for at least a subgroup of patients. Fourth, our data was personally and carefully reviewed by two authors. Fifth, our study provides concrete recommendations on how to approach the patient at the onset of the SARS-CoV-2 infection. In a critical moment, such as a pandemic, it is crucial to have clear indications on the management of the patient at home [25].
Our results confirm the role of gender, age and medical history of hypertension in kidney outcome and survival in COVID-19. Moreover, we suggest including blood pressure measurement in initial, at-home screening for SARS-Cov2 infection. The aim of this strategy would be to maintain BP values > 120/70 mmHg in patients on chronic anti-hypertensive therapy through the timely reduction of these drugs.
Follow-up of patients to assess the need for antihypertensive therapy reintroduction, therefore, becomes imperative, also taking into account the effect of weight changes during illness. Considering the high frequency of proteinuria at presentation, we propose that it should be re-evaluated during follow-up.
Abbreviations
- AKI:
-
Acute kidney injury
- CAD:
-
Coronary artery disease
- CKD:
-
Chronic kidney disease
- COPD:
-
Chronic obstructive pulmonary disease
- DBP:
-
Diastolic blood pressure
- ED-AKI:
-
Presence of acute kidney failure at Emergency Department admission
- ED-MBP:
-
Mean arterial blood pressure levels at presentation
- ED:
-
Emergency department
- FiO2 :
-
Fraction of inspired oxygen
- H-AKI:
-
In-hospital kidney failure development
- HD:
-
Hazard ratios
- HR:
-
Heart rate
- HYP:
-
History of hypertension
- ICU:
-
Intensive care unit
- IHD:
-
In-hospital death
- IQR:
-
Interquartile range
- MBP:
-
Mean arterial blood pressure
- NPL:
-
Malignancy
- OR:
-
Odds ratio
- SatO2 :
-
Peripheral arterial oxygen saturation
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviations
References
Zangrillo A, Zanella A, Antonelli M et al (2020) Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA 323:1574. https://doi.org/10.1001/jama.2020.5394
Huang C, Wang Y, Li X et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395:497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
Chen N, Zhou M, Dong X et al (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395:507–513. https://doi.org/10.1016/S0140-6736(20)30211-7
Fan C, Li K, Ding Y et al (2020) ACE2 expression in kidney and testis may cause kidney and testis damage after 2019-nCoV infection. MedRxiv 71:9180
Su H, Yang M, Wan C et al (2020) Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. https://doi.org/10.1016/j.kint.2020.04.003
Mehta P, McAuley DF, Brown M et al (2020) COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 395:1033–1034. https://doi.org/10.1016/S0140-6736(20)30628-0
Ruan Q, Yang K, Wang W et al (2020) Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 46:846–848. https://doi.org/10.1007/s00134-020-05991-x
Ciceri F, Castagna A, Rovere-Querini P et al (2020) Early predictors of clinical outcomes of COVID-19 outbreak in Milan Italy. Clin Immunol 217:108509. https://doi.org/10.1016/j.clim.2020.108509
Guan W-J, Ni Z-Y, Hu Y et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382:1708–1720. https://doi.org/10.1056/NEJMoa2002032
Iaccarino G, Grassi G, Borghi C et al (2020) Age and multimorbidity predict death among COVID-19 patients: results of the SARS-RAS study of the Italian Society of Hypertension. Hypertension 26:hypertensionaha12015324. https://doi.org/10.1161/HYPERTENSIONAHA.120.15324
Zou X, Chen K, Zou J et al (2020) Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med 14:185–192. https://doi.org/10.1007/s11684-020-0754-0
Ferrario CM, Jessup J, Chappell MC et al (2005) Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation 111:2605–2610. https://doi.org/10.1161/CIRCULATIONAHA.104.510461
AlGhatrif M, Cingolani O, Lakatta EG (2020) The dilemma of coronavirus disease 2019, aging, and cardiovascular disease: insights from cardiovascular aging science. JAMA Cardiol. https://doi.org/10.1001/jamacardio.2020.1329
Hirsch JS, Ng JH, Ross DW et al (2020) Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. https://doi.org/10.1016/j.kint.2020.05.006
Ronco C, Reis T, Husain-Syed F (2020) Management of acute kidney injury in patients with COVID-19. Lancet Respir Med. https://doi.org/10.1016/S2213-2600(20)30229-0
Varga Z, Flammer AJ, Steiger P et al (2020) Endothelial cell infection and endotheliitis in COVID-19. Lancet 395:1417–1418. https://doi.org/10.1016/S0140-6736(20)30937-5
Rossi GM, Delsante M, Pilato FP et al (2020) Kidney biopsy findings in a critically ill COVID-19 patient with dialysisdependent acute kidney injury: a case against “SARS-CoV-2 nephropathy.” Kidney Int Rep 5:1100–1105. https://doi.org/10.1016/j.ekir.2020.05.005
Zangrillo A, Beretta L, Scandroglio AM et al (2020) Characteristics, treatment, outcomes and cause of death of invasively ventilated patients with COVID-19 ARDS in Milan, Italy. Crit Care Resusc 22(3):200–211
Zangrillo A, Landoni G, Beretta L et al (2020) Angiotensin II infusion in COVID-19-associated vasodilatory shock: a case series. Crit Care 24:227–234. https://doi.org/10.1186/s13054-020-02928-0
(2012) KDIGO clinical practice guidelines for acute kidney injury. Kidney Intern Suppl 2:1. https://doi.org/10.1038/kisup.2012.1
Vincent JL, Moreno R, Takala J et al (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Pandharipande PP, Shintani AK, Hagerman HE et al (2009) Derivation and validation of Spo2/Fio2 ratio to impute for Pao2/Fio2 ratio in the respiratory component of the Sequential Organ Failure Assessment score. Crit Care Med 37:1317–1321. https://doi.org/10.1097/CCM.0b013e31819cefa9
YOUDEN WJ, (1950) Index for rating diagnostic tests. Cancer 3:32–35
Malberti F, Pecchini P, Marchi G et al (2020) When a nephrology ward becomes a COVID-19 ward: the Cremona experience. J Nephrol 33:625–628. https://doi.org/10.1007/s40620-020-00743-y
Piccoli GB (2020) Hospitals as health factories and the coronavirus epidemic. J Nephrol 33:189–191. https://doi.org/10.1007/s40620-020-00719-y
Acknowledgements
We sincerely thank Ms. Emily-Jo Beth Reer for her support in English revision.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Consortia
Contributions
CL: research idea and study design; CL, MS, PM: data analysis/interpretation; CL, MS, TA, VG, MP: draft preparation; EM: sample and database management; RB, PB, MA, GM, CM: data acquisition; PRQ, FC, AC, VG, MP: supervision or mentorship. CM and MS provided an equal contribution to the paper and share the role of the first author. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
All data used in this study were collected in accordance with the ethical standards of the institutional and research committees, with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. According to the European GDPR, all data were anonymized before collection. See “Materials and Methods” section for details.
Competing interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lanzani, C., Simonini, M., Arcidiacono, T. et al. Role of blood pressure dysregulation on kidney and mortality outcomes in COVID-19. Kidney, blood pressure and mortality in SARS-CoV-2 infection. J Nephrol 34, 305–314 (2021). https://doi.org/10.1007/s40620-021-00997-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-021-00997-0