Abstract
Sodium-glucose cotransporter 2 inhibitors (SGLT2i) are a relatively new class of antidiabetic drugs that in addition to emerging as an effective antihyperglycemic treatment have been shown to improve, in several trials, both renal and cardiovascular outcomes. In consideration of the renal site of action and the associated osmotic diuresis, a negative sodium balance has been postulated during SGLT2i administration. Actually, sodium and water depletion may contribute to some positive actions of SGLT2i but evidence is far from being conclusive and the real physiologic effects of SGLT2i on sodium remain largely unknown. Indeed, no study has yet investigated how SGLT2i change sodium balance in the long term and especially the pathways through which the natriuretic effect is expressed. Furthermore, several experimental studies have recently identified different pathways, not directly linked to tubular sodium handling, which could contribute to the renal and cardiovascular benefits associated with SGLT2i. This paper will review the evidence of SGLT2i action on sodium transporters, their off-target effects and their potential role on kidney protection.


Similar content being viewed by others
References
Verma S, McMurray JJV (2018) SGLT2 inhibitors and mechanisms of cardiovascular benefit: a state-of- the-art review. Diabetologia 61:2108–2117
Kaplan A, Abidi E, El-Yazbi A et al (2018) Direct cardiovascular impact of SGLT2 inhibitors: mechanisms and effects. Heart Fail Rev 23:419–437
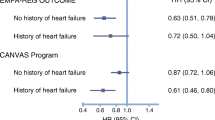
Zinman B, Wanner C, Lachin JM et al (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373:2117–2128
Cavender MA, Steg G, Smith SC et al (2015) Impact of diabetes mellitus on hospitalization for heart failure, cardiovascular events, and death. Circulation 132:923–931
Neal B, Perkovic V, Mahaffey KW et al (2017) Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 377:644–657
Wiviott SD, Raz I, Bonaca MP et al (2019) Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 380:347–357
Kenneth WM (2019) Canagliflozin and cardiovascular and renal outcomes in type 2 diabetes mellitus and chronic kidney disease in primary and secondary cardiovascular prevention groups: results from the randomized CREDENCE trial. Circulation 140(9):739–750
Dekkers CCJ, Wheeler DC, Sjöström CD, Stefansson BV, Cain V, Heerspink HJL (2018) Effects of the sodium-glucose co-transporter 2 inhibitor dapagliflozin in patients with type 2 diabetes and stages 3b–4 chronic kidney disease. Nephrol Dial Transpl 33(11):2005–2011
Ansary TM, Fujisawa Y, Rahman A, Nakano D, Hitomi H, Kobara H, Masaki T, Titze JM, Kitada K, Nishiyama A (2017) Responses of renal hemodynamics and tubular functions to acute sodium-glucose cotransporter 2 inhibitor administration in non-diabetic anesthetized rats. Sci Rep 7:9555. https://doi.org/10.1038/s41598-017-09352-5
Thomson SC, Rieg T, Miracle C, Mansoury H, Whaley J, Vallon V, Singh P (2012) Acute and chronic effects of SGLT2 blockade on glomerular and tubular function in the early diabetic rat. Am J Physiol Regul Integr Comp Physiol 302:R75–R83
Tanaka H, Takano K, Iijima H, Kubo H, Maruyama N, Hashimoto T, Arakawa K, Togo M, Inagaki N, Kaku K (2017) Factors affecting canagliflozin-induced transient urine volume increase in patients with type 2 diabetes mellitus. Adv Ther 34:436–451
Rajasekeran H, Lytvyn Y, Cherney DZ (2016) Sodium-glucose cotransporter 2 inhibition and cardiovascular risk reduction in patients with type 2 diabetes: the emerging role of natriuresis. Kidney Int 89:524–526
Sha S, Polidori D, Heise T, Natarajan J, Farrell K, Wang SS, Sica D, Rothenberg P, Plum-Morschel L (2014) Effect of the sodium glucose co-transporter 2 inhibitor canagliflozin on plasma volume in patients with type 2 diabetes mellitus. Diabetes Obes Metab 16:1087–1095
Iijima H, Kifuji T, Maruyama N, Inagaki N (2015) Pharmacokinetics, pharmacodynamics, and safety of canagliflozin in Japanese patients with type 2 diabetes mellitus. Adv Ther 32:768–782
Weir MR, Kline I, Xie J, Edwards R, Usiskin K (2019) Effect of canagliflozin on serum electrolytes in patients with type 2 diabetes in relation to estimated glomerular filtration rate (eGFR). Curr Med Res Opin 30:1759–1768. https://doi.org/10.1185/03007995.2014.919907
Abdul-Ghani M, Del Prato S, Chilton R, DeFronzo RA (2016) SGLT2 inhibitors and cardiovascular risk: lessons learned from the EMPA-REG OUTCOME study. Diabetes Care 39:717–725. https://doi.org/10.2337/dc16-0041
Lambers Heerspink HJ, de Zeeuw D, Wie L, Leslie B, List J (2013) Dapagliflozin a glucose-regulating drug with diuretic properties in subjects with type 2 diabetes. Diabetes Obes Metab 15:853–862. https://doi.org/10.1111/dom.12127
Abdul-Ghani MA, DeFronzo RA, Norton L (2013) Novel hypothesis to explain why SGLT2 inhibitors inhibit only 30–50% of filtered glucose load in humans. Diabetes 62:3324–3328
Reed JW (2016) Impact of sodium-glucose cotransporter 2 inhibitors on blood pressure. Vasc Health Risk Manag 12:393–405
Ansary TM, Nakano D, Nishiyama A (2019) Diuretic effects of sodium glucose cotransporter 2 inhibitors and their influence on the renin-angiotensin system. Int J Mol Sci. 20(3):629
Shin SJ, Chung S, Kim SJ, Lee EM, Yoo YH, Kim JW, Ahn YB, Kim ES, Moon SD, Kim MJ et al (2016) Effect of sodium-glucose co-transporter 2 inhibitor, dapagliflozin, on renal renin-angiotensin system in an animal model of type 2 diabetes. PLoS ONE 11:e0165703
McCullough PA, Kluger AY, Tecson KM, Barbin CM, Lee AY, Lerma EV, Rosol ZP, Kluger SL, Rangaswami J (2018) Inhibition of the sodium-proton antiporter (exchanger) is a plausible mechanism of potential benefit and harm for drugs designed to block sodium glucose co-transporter 2. Rev Cardiovasc Med 19(2):51–63. https://doi.org/10.31083/j.rcm.2018.02.021
Kimura G (2016) Importance of inhibiting sodium glucose cotransporter and its compelling indication in t2diabetes: pathophysiological hypothesis. J Am Soc Hypertens 10(3):271–278
Mayer GJ, Wanner C et al (2019) Analysis from the EMPA-REG OUTCOME® trial indicates empagliflozin may assist in preventing the progression of chronic kidney disease in patients with type 2 diabetes irrespective of medications that alter intrarenal hemodynamics. Kidney Int 96(2):489–504
Baartscheer A, Schumacher CA, Wüst RC, Fiolet JW, Stienen GJ, Coronel R (2017) Zuurbier CJ Empagliflozin decreases myocardial cytoplasmic Na+ through inhibition of the cardiac Na+/H+ exchanger in rats and rabbits. Diabetologia 60(3):568–573. https://doi.org/10.1007/s00125-016-4134
Satou R et al (2012) Interferon-γ biphasically regulates angiotensinogen expression via a JAK-STAT pathway and suppressor of cytokine signaling 1 (SOCS1) in renal proximal tubular cells. FASEB J 26:1821–1830
Javier Donate-Correa et al. (2015) Inflammatory citokynes in diabetic nephropathy. J Diabetes Res
Baer PC (2020) Kidney inflammation, injury and regeneration. https://doi.org/10.3390/ijms21031164
Iannantuoni F, de Marañon AM et al (2019) The SGLT2 inhibitor empagliflozin ameliorates the inflammatory profile in type 2 diabetic patients and promotes an antioxidant response in leukocytes. J Clin Med 8(11):1814
Schneider MP, Raff U, Kopp C et al (2017) Skin sodium concentration corre- lates with left ventricular hypertrophy in CKD. J Am Soc Nephrol 28:1867–1876
Pogwizd SM, Sipido KR, Verdonck F et al (2003) Intracellular Na in animal models of hypertrophy and heart failure: contractile function and arrhythmogenesis. Cardiovasc Res 57:887–896
Cingolani HE, Ennis IL (2007) Sodium-hydrogen exchanger, cardiac overload, and myocardial hypertrophy. Circulation 115:1090–1100
Schmieder R, Ott C, Linz P, Jumar A et al (2016) OS 12–03 SGLT-2-inhibition with dapagliflozin reduces tissue sodium content. J Hypertens 34(suppl 1):e76
Brouwer TF, Vehmeijer JT, Kalkman DN et al (2018) Intensive blood pressure lowering in patients with and patients without type 2 diabetes: a pooled analysis from two randomized trials. Diabetes Care 41:1142–1148
Donowitz M, Ming Tse C, Fuster D (2013) SLC9/NHE gene family, a plasma membrane and organellar family of Na+/H+ exchangers. Mol Aspects Med 34:236–251
Wanner C, Inzucchi S et al (2016) Empaglifozin and progression of kidney disease in type 2 diabetes. N Engl J Med 375:323–334
Cassi P, Locatelli M et al. (2018) SGLT2 inhibitor dapagliflozin limits podocyte damage in proteinuric nondiabetic nephropathy. JCI Insight 3(15)
Yaribeygi H, Katsiki N, Butler AE, Sahebkar A (2019) Effects of anti- diabetic drugs on NLRP3 inflammasome activity, with a focus on diabetic kidneys. Drug Discov Today 24(1):256–262
Glick D et al (2010) Autophagy: cellular and molecular mechanisms. J Pathol 221(1):3–121
Rajani R, Pastor-Soler NM, Hallows KR (2017) Role of AMP-activated pro- tein kinase in kidney tubular transport, metabolism, and disease. Curr Opin Nephrol Hypertens 26:375–383
Lang F, Föller M (2014) Regulation of ion channels and transporters by AMP-activated kinase (AMPK). Channels 8(1):20–28
Packer M et al (2020) Interplay of adenosine monophosphate-activated protein kinase/sirtuin-1 activation and sodium influx inhibition mediates the renal benefits of sodium-glucose co-transporter-2 inhibitors in type 2 diabetes: a novel conceptual framework. Diabetes Obes Metab. 22(5):734–742
Huang DY, Gao H, Boini KM, Osswald H, Nürnberg B, Lang F (2010) In vivo stimulation of AMP-activated protein kinase enhanced tubuloglomerular feedback but reduced tubular sodium transport during high dietary NaCl intake. Pflugers Arch 460:187–196
Heerspink HJL, Stefansson BV, Chertow GM, Correa-Rotter R, Greene T, Hou FF, Lindberg M, McMurray J, Rossing P, Toto R, Langkilde AM, Wheeler DC (2020) Rationale and protocol of the dapagliflozin and prevention of adverse outcomes in chronic kidney disease (DAPA-CKD) randomized controlled trial. Nephrol Dial Transpl 35(2):274–282
Herrington WG et al (2018) The potential for improving cardio-renal outcomes by sodium-glucose co-transporter-2 inhibition in people with chronic kidney disease: a rationale for the EMPA-KIDNEY study. Clin Kidney J 11(6):749–761
Østergaard JA, Cooper ME, Jandeleit-Dahm KA (2020) Targeting oxidative stress and anti-oxidant defence in diabetic kidney disease. J Nephrol. https://doi.org/10.1007/s40620-020-00749-6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Ethical standards
The study has been approved by an appropriate ethics committee and has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
De Pascalis, A., Cianciolo, G., Capelli, I. et al. SGLT2 inhibitors, sodium and off-target effects: an overview. J Nephrol 34, 673–680 (2021). https://doi.org/10.1007/s40620-020-00845-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-020-00845-7