Abstract
Purpose
The screening and diagnosis of osteoporosis in patients with type 2 diabetes mellitus (T2DM) based on bone mineral density remains challenging because of the limited availability and accessibility of dual-energy X-ray absorptiometry. We aimed to develop and validate models to predict the risk of osteoporosis in postmenopausal women with T2DM based on machine learning (ML) algorithms.
Methods
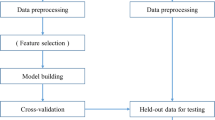
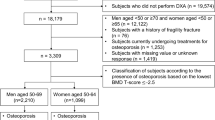
This retrospective study included 303 postmenopausal women with T2DM. To develop prediction models for osteoporosis, we applied nine ML algorithms combined with demographic, clinical, and laboratory data. The least absolute shrinkage and selection operator were used to perform feature selection. We used the bootstrap resampling technique for model training and validation. To test the performance of the models, we calculated indices including the area under the receiver operating characteristic curve (AUROC), accuracy, sensitivity, specificity, positive predictive value, negative predictive value, F1 score, calibration curve, and decision curve analysis. Furthermore, we conducted fivefold cross-validation for parameter optimization and model validation. Feature importance was assessed using the SHapley additive explanation (SHAP).
Results
We identified 10 independent predictors as the most valuable features. An AUROC of 0.616–1.000 was observed for nine ML algorithms. The extreme gradient boosting (XGBoost) model exhibited the best performance, outperforming conventional risk assessment tools and registering 0.993 in the training set, 0.798 in the validation set, and 0.786 in the test set for fivefold cross-validation. Using SHAP, we found that the explanatory variables contributed to the model and their relationship with osteoporosis occurrence. Furthermore, we developed a user-friendly tool for calculating the risk of osteoporosis.
Conclusions
With the integration of demographic and clinical risk factors, ML algorithms can accurately predict osteoporosis. The XGBoost model showed ideal performance. With the incorporation of these models in the clinic, patients may benefit from early osteoporosis diagnosis and treatment.





Similar content being viewed by others
Data availability
Some or all of the datasets generated and/or analyzed in the current study are not publicly available, but are available on reasonable request by the relevant authors.
References
Valderrabano RJ, Linares MI (2018) Diabetes mellitus and bone health: epidemiology, etiology and implications for fracture risk stratification. Clin Diabetes Endocrinol 4(9):1. https://doi.org/10.1186/s40842-018-0060-9
Hofbauer LC, Busse B, Eastell R, Ferrari S, Frost M, Muller R, Burden AM, Rivadeneira F, Napoli N, Rauner M (2022) Bone fragility in diabetes: novel concepts and clinical implications. Lancet Diabetes Endocrinol 10(3):207–220. https://doi.org/10.1016/S2213-8587(21)00347-8
Greenhill C (2018) Shared variants for osteoporosis and T2DM. Nat Rev Endocrinol 14(11):627. https://doi.org/10.1038/s41574-018-0095-0
Camacho PM, Petak SM, Binkley N, Diab DL, Eldeiry LS, Farooki A, Harris ST, Hurley DL, Kelly J, Lewiecki EM, Pessah-Pollack R, McClung M, Wimalawansa SJ, Watts NB (2020) American Association of Clinical Endocrinologists/American College of endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update. Endocr Pract 26(Suppl 1):1–46. https://doi.org/10.4158/GL-2020-0524SUPPL
Choksi P, Jepsen KJ, Clines GA (2018) The challenges of diagnosing osteoporosis and the limitations of currently available tools. Clin Diabetes Endocrinol 4(12):1. https://doi.org/10.1186/s40842-018-0062-7
Sheu A, Greenfield JR, White CP, Center JR (2022) Assessment and treatment of osteoporosis and fractures in type 2 diabetes. Trends Endocrinol Metab 33(5):333–344. https://doi.org/10.1016/j.tem.2022.02.006
Goswami R, Nair A (2019) Diabetes mellitus, vitamin D and osteoporosis: insights. Indian J Med Res 150(5):425–428. https://doi.org/10.4103/ijmr.IJMR_1920_19
Khosla S, Melton LJ 3rd (2007) Clinical practice. Osteopenia N Engl J Med 356(22):2293–2300. https://doi.org/10.1056/NEJMcp070341
Toh LS, Lai PSM, Wu DB, Bell BG, Dang CPL, Low BY, Wong KT, Guglielmi G, Anderson C (2019) A comparison of 6 osteoporosis risk assessment tools among postmenopausal women in Kuala Lumpur. Malaysia Osteoporos Sarcopenia 5(3):87–93. https://doi.org/10.1016/j.afos.2019.09.001
Ho-Pham LT, Doan MC, Van LH, Nguyen TV (2020) Development of a model for identification of individuals with high risk of osteoporosis. Arch Osteoporos 15(1):111. https://doi.org/10.1007/s11657-020-00788-3
Benke K, Benke G (2018) Artificial intelligence and big data in public health. Int J Environ Res Public Health 15(12):1. https://doi.org/10.3390/ijerph15122796
Obermeyer Z, Emanuel EJ (2016) Predicting the future—big data, machine learning, and clinical medicine. N Engl J Med 375(13):1216–1219. https://doi.org/10.1056/NEJMp1606181
Shim JG, Kim DW, Ryu KH, Cho EA, Ahn JH, Kim JI, Lee SH (2020) Application of machine learning approaches for osteoporosis risk prediction in postmenopausal women. Arch Osteoporos 15(1):169. https://doi.org/10.1007/s11657-020-00802-8
Park HW, Jung H, Back KY, Choi HJ, Ryu KS, Cha HS, Lee EK, Hong AR, Hwangbo Y (2021) Application of machine learning to identify clinically meaningful risk group for osteoporosis in individuals under the recommended age for dual-energy X-ray absorptiometry. Calcif Tissue Int 109(6):645–655. https://doi.org/10.1007/s00223-021-00880-x
Ou Yang WY, Lai CC, Tsou MT, Hwang LC (2021) Development of machine learning models for prediction of osteoporosis from clinical health examination data. Int J Environ Res Public Health 18(14):1. https://doi.org/10.3390/ijerph18147635
Yoo TK, Kim SK, Kim DW, Choi JY, Lee WH, Oh E, Park EC (2013) Osteoporosis risk prediction for bone mineral density assessment of postmenopausal women using machine learning. Yonsei Med J 54(6):1321–1330. https://doi.org/10.3349/ymj.2013.54.6.1321
Wang Y, Wang L, Sun Y, Wu M, Ma Y, Yang L, Meng C, Zhong L, Hossain MA, Peng B (2021) Prediction model for the risk of osteoporosis incorporating factors of disease history and living habits in physical examination of population in Chongqing, Southwest China: based on artificial neural network. BMC Public Health 21(1):991. https://doi.org/10.1186/s12889-021-11002-5
Chin KY, Ng BN, Rostam MKI, Muhammad Fadzil NFD, Raman V, Mohamed Yunus F, Syed Hashim SA, Ekeuku SO (2022) A mini review on osteoporosis: from biology to pharmacological management of bone loss. J Clin Med 11(21):1. https://doi.org/10.3390/jcm11216434
Zhang W, Gao R, Rong X, Zhu S, Cui Y, Liu H, Li M (2022) Immunoporosis: role of immune system in the pathophysiology of different types of osteoporosis. Front Endocrinol (Lausanne) 13:965258. https://doi.org/10.3389/fendo.2022.965258
Lorenzo J (2020) Cytokines and bone: osteoimmunology. Handb Exp Pharmacol 262:177–230. https://doi.org/10.1007/164_2019_346
Donath MY, Shoelson SE (2011) Type 2 diabetes as an inflammatory disease. Nat Rev Immunol 11(2):98–107. https://doi.org/10.1038/nri2925
Sowers MR, La Pietra MT (1995) Menopause: its epidemiology and potential association with chronic diseases. Epidemiol Rev 17(2):287–302. https://doi.org/10.1093/oxfordjournals.epirev.a036194
Drouin P, Blickle JF, Charbonnel B, Eschwege E, Guillausseau PJ, Plouin PF, Daninos JM, Balarac N, Sauvanet JP (1999) Diagnosis and classification of diabetes mellitus: the new criteria. Diabetes Metab 25(1):72–83
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation: modification of Diet in Renal Disease Study Group. Ann Intern Med 130(6):461–470. https://doi.org/10.7326/0003-4819-130-6-199903160-00002
Consensus development conference (1993) diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med 94(6):646–650. https://doi.org/10.1016/0002-9343(93)90218-e
Chiu A, Ayub M, Dive C, Brady G, Miller CJ (2017) twoddpcr: an R/Bioconductor package and Shiny app for Droplet Digital PCR analysis. Bioinformatics 33(17):2743–2745. https://doi.org/10.1093/bioinformatics/btx308
Wang C, Zhang T, Wang P, Liu X, Zheng L, Miao L, Zhou D, Zhang Y, Hu Y, Yin H, Jiang Q, Jin H, Sun J (2021) Bone metabolic biomarker-based diagnosis of type 2 diabetes osteoporosis by support vector machine. Ann Transl Med 9(4):316. https://doi.org/10.21037/atm-20-3388
Meng J, Sun N, Chen Y, Li Z, Cui X, Fan J, Cao H, Zheng W, Jin Q, Jiang L, Zhu W (2019) Artificial neural network optimizes self-examination of osteoporosis risk in women. J Int Med Res 47(7):3088–3098. https://doi.org/10.1177/0300060519850648
Shaabanpour Aghamaleki F, Mollashahi B, Nosrati M, Moradi A, Sheikhpour M, Movafagh A (2019) Application of an artificial neural network in the diagnosis of chronic lymphocytic leukemia. Cureus 11(2):e4004. https://doi.org/10.7759/cureus.4004
Smets J, Shevroja E, Hugle T, Leslie WD, Hans D (2021) Machine learning solutions for osteoporosis—a review. J Bone Miner Res 36(5):833–851. https://doi.org/10.1002/jbmr.4292
Raisz LG (2005) Clinical practice: screening for osteoporosis. N Engl J Med 353(2):164–171. https://doi.org/10.1056/NEJMcp042092
Walsh JS, Vilaca T (2017) Obesity, type 2 diabetes and bone in adults. Calcif Tissue Int 100(5):528–535. https://doi.org/10.1007/s00223-016-0229-0
Fassio A, Idolazzi L, Rossini M, Gatti D, Adami G, Giollo A, Viapiana O (2018) The obesity paradox and osteoporosis. Eat Weight Disord 23(3):293–302. https://doi.org/10.1007/s40519-018-0505-2
Zhang J, Li Y, Lai D, Lu D, Lan Z, Kang J, Xu Y, Cai S (2021) Vitamin D status is negatively related to insulin resistance and bone turnover in chinese non-osteoporosis patients with type 2 diabetes: a retrospective cross-section research. Front Public Health 9:727132. https://doi.org/10.3389/fpubh.2021.727132
Shanbhogue VV, Hansen S, Frost M, Jorgensen NR, Hermann AP, Henriksen JE, Brixen K (2016) Compromised cortical bone compartment in type 2 diabetes mellitus patients with microvascular disease. Eur J Endocrinol 174(2):115–124. https://doi.org/10.1530/EJE-15-0860
Chen J, Hendriks M, Chatzis A, Ramasamy SK, Kusumbe AP (2020) Bone vasculature and bone marrow vascular niches in health and disease. J Bone Miner Res 35(11):2103–2120. https://doi.org/10.1002/jbmr.4171
Zhao Z (2018) Correlation analysis of urine proteins and inflammatory cytokines with osteoporosis in patients with diabetic nephropathy. J Musculoskelet Neuronal Interact 18(3):348–353
Lee HS, Hwang JS (2020) Impact of type 2 diabetes mellitus and antidiabetic medications on bone metabolism. Curr Diab Rep 20(12):78. https://doi.org/10.1007/s11892-020-01361-5
Sun M, Yang J, Wang J, Hao T, Jiang D, Bao G, Liu G (2016) TNF-alpha is upregulated in T2DM patients with fracture and promotes the apoptosis of osteoblast cells in vitro in the presence of high glucose. Cytokine 80:35–42. https://doi.org/10.1016/j.cyto.2016.01.011
Acknowledgements
This work is supported by the the Extreme Smart Analysis platform (http://xsmartanalysis.cn/) and EmpowerStats (http://www.empowerstats.com). Thanks are also extended to Bullet Edits Company for professional language improvement.
Funding
This study was supported by the Youth Science and technology project, Hebei Medical Science Research Project (20211155).
Author information
Authors and Affiliations
Contributions
XW and FZ designed the study. AC and JW collected the data. XW and FZ analyzed the data. XW wrote and edited the article. YG improved the English language. JZ revised the article for intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Consent to participate
Written informed consent for participation was waived by the Ethics Committee of Cangzhou Central Hospital.
Consent for publication
All of the authors approved the publication of the article.
Ethical approval
This study was approved by the Ethics Committee of Cangzhou Central Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, X., Zhai, F., Chang, A. et al. Application of machine learning algorithms to predict osteoporosis in postmenopausal women with type 2 diabetes mellitus. J Endocrinol Invest 46, 2535–2546 (2023). https://doi.org/10.1007/s40618-023-02109-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02109-0