Abstract
Introduction
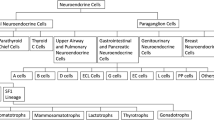
Pituitary neuroendocrine tumors (PitNETs) represent 15–18.2% of all intracranial tumors. Their clinical presentation can range from chronic headache, visual defects, hypopituitarism to hormone excess syndromes. PitNETS are commonly classified as functioning neuroendocrine tumors (F-PitNETs) and non-functioning neuroendocrine tumors (NF-PitNETs). At the moment, new classification has emerged based on cell lineages. Almost 50% of all patients with PitNETs require surgical intervention, and about 25% of these have residual and persistent disease that may require additional management.
Subjects and methods
A retrospective cohort of medical records of patients with PitNETs, aiming to describe the incidence of recurrence of patients who received surgical treatment over a 12 month follow up period at San Jose Hospital (SJH) in Bogotá, Colombia, over an observation period of 10 years. Furthermore, clinical presentation, biochemical characteristics and immunohistochemistry, postoperative complications are detailed.
Results
Eight hundred and eighty-seven patients with pituitary tumors were included in the cohort; 83% (737/887) had a diagnosis of PitNET. Of these, 18.9% (140) received surgical management. The majority 58% (98/140) had nonfunctional-PitNETs (NF-PitNETs), followed by growth-hormone-secreting pituitary adenoma (22.1%; 33/140), adrenocorticotropic- hormone-secreting pituitary adenoma (9.3%; 13/140), and prolactinomas (9.3%; 13/140). A recurrence was found in 45.71% (64/140), subclassified as biochemical in 15.71% (22/140), controlled with medications in 20% (28/140), and remission occurred in 18.57% (26/140).
Conclusion
Clinical presentation and incidence of recurrence in patients with PitNETs in a referral center in Colombia are similar to other surgical cohorts with low cure rates and high recurrence.




Similar content being viewed by others
Data availability
Data of this study are available in the investigations division for University Foundation of Health Sciences and from the corresponding author.
References
Asa SL, Mete O, Perry A, Osamura RY (2022) Overview of the 2022 WHO classification of pituitary tumors. Endocr Pathol 33(1):6–26. https://doi.org/10.1007/s12022-022-09703-7
Qin J, Li K, Wang X, Bao Y (2021) A comparative study of functioning and non-functioning pituitary adenomas. Medicine 100(14):e25306. https://doi.org/10.1097/MD.0000000000025306
Liu Z, Zhang H, Liu S, Chen H (2019) The functional evaluation of pituitary in patients with a surgical resection of sellar tumours. Arch Med Sci AMS 16(2):460–465. https://doi.org/10.5114/aoms.2019.89356
Melmed S (2020) Pituitary-tumor endocrinopathies. N Engl J Med 382(10):937–950. https://doi.org/10.1056/NEJMra1810772
Neou M, Villa C, Armignacco R, Jouinot A, Raffin-Sanson ML, Septier A, Letourneur F, Diry S, Diedisheim M, Izac B, Gaspar C, Perlemoine K, Verjus V, Bernier M, Boulin A, Emile JF, Bertagna X, Jaffrezic F, Laloe D, Baussart B, Assié G (2020) Pangenomic classification of pituitary neuroendocrine tumors. Cancer Cell 37(1):123-134.e5. https://doi.org/10.1016/j.ccell.2019.11.002
Asa SL, Asioli S, Bozkurt S, Casar-Borota O, Chinezu L, Comunoglu N, Cossu G, Cusimano M, Delgrange E, Earls P, Ezzat S, Gazioglu N, Grossman A, Guaraldi F, Hickman RA, Ikeda H, Jaffrain-Rea ML, Karavitaki N, Kraljević I, La Rosa S, Yarman S (2020) Pituitary neuroendocrine tumors (PitNETs): nomenclature evolution, not clinical revolution. Pituitary 23(3):322–325. https://doi.org/10.1007/s11102-019-01015-0
Asa SL, Mete O, Cusimano MD, McCutcheon IE, Perry A, Yamada S, Nishioka H, Casar-Borota O, Uccella S, La Rosa S, Grossman AB, Ezzat S, Attendees of the 15th Meeting of the International Pituitary Pathology Club, Istanbul October 2019 (2021) Pituitary neuroendocrine tumors: a model for neuroendocrine tumor classification. Modern Pathol 34(9):1634–1650. https://doi.org/10.1038/s41379-021-00820-y
Henao DC, Rojas W (2014) Manejo de pacientes con diagnóstico de adenoma hipofisario productor de prolactina. Experiencia del Hospital San José. Revista Colombiana de Endocrinología Diabetes Metabolismo 1(1):20–26. https://doi.org/10.53853/encr.1.1.57
Rojas W (2003) Actualización en Acromegalia. Revista Repertorio de Medicina y Cirugía 12(2):59–66. https://doi.org/10.31260/RepertMedCir.v12.n2.2003.315
Rojas W, Lancheros AH, Tapiero M (2015) Descripción de las alteraciones cardiacas por ecocardiografía de los pacientes con acromegalia en el Hospital de San José. Bogotá Acta Médica Colombiana 40(1):30–35. https://doi.org/10.36104/amc.2015.332
Tovar H, Rojas W (2010) Experiencia en acromegalia en el Hospital de San José Reporte de serie de casos 1990–2007. Acta Médica Colombiana. 35(2):48–52
Rojas W, Tovar H, Florez A (2019) Pituitary gigantism: a case series from Hospital de San José (Bogotá, Colombia). Arch Endocrinol Metab 63(4):385–393. https://doi.org/10.20945/2359-3997000000150
Melmed S, Kaiser UB, Lopes MB, Bertherat J, Syro LV, Raverot G et al (2022) Clinical biology of the pituitary adenoma. Endocr Rev. https://doi.org/10.1210/endrev/bnac010
Lenders NF, Wilkinson AC, Wong SJ, Shein TT, Harvey RJ, Inder WJ et al (2021) Transcription factor immunohistochemistry in the diagnosis of pituitary tumours. Eur J Endocrinol 184(6):891–901. https://doi.org/10.1530/eje-20-1273
Treppiedi D, Barbieri AM, Di Muro G, Marra G, Mangili F, Catalano R et al (2021) Genetic profiling of a cohort of Italian patients with ACTH-secreting pituitary tumors and characterization of a novel USP8 gene variant. Cancers. https://doi.org/10.3390/cancers13164022
Neou M, Villa C, Armignacco R, Jouinot A, Raffin-Sanson ML, Septier A et al (2020) Pangenomic classification of pituitary neuroendocrine tumors. Cancer Cell 37(1):123–34.e5. https://doi.org/10.1016/j.ccell.2019.11.002
Broersen LHA, Jha M, Biermasz NR, Pereira AM, Dekkers OM (2018) Effectiveness of medical treatment for Cushing’s syndrome: a systematic review and meta-analysis. Pituitary 21(6):631–641. https://doi.org/10.1007/s11102-018-0897-z
Cho HJ, Kim H, Kwak YJ, Seo JW, Paek SH, Sohn C-H et al (2014) Clinicopathologic analysis of pituitary adenoma: a single institute experience. J Korean Med Sci 29(3):405–410. https://doi.org/10.3346/jkms.2014.29.3.405
Krivoy O (2010) Evolución del tratamiento neuroquirúrgico de la patología hipofisaria: Experiencia de 800 casos. Gac méd Caracas, pp 42–52
Tampourlou M, Ntali G, Ahmed S, Arlt W, Ayuk J, Byrne JV et al (2017) Outcome of nonfunctioning pituitary adenomas that regrow after primary treatment: a study from two large UK centers. J Clin Endocrinol Metab 102(6):1889–1897. https://doi.org/10.1210/jc.2016-4061
Valenciano EV, Miranda MÁE, Valverde AO, Galindo MQ (2016) Características epidemiológicas y complicaciones de los pacientes operados por adenomas de hipófisis por vía transesfenoidal endoscópica en la Unidad de Cirugía de Base de Cráneo del Hospital México. Revista Clínica de la Escuela de Medicina de la Universidad de Costa Rica 6(1):1–7. https://doi.org/10.15517/RC_UCR-HSJD.V6I1.23054
Watts AK, Easwaran A, McNeill P, Wang YY, Inder WJ, Caputo C (2017) Younger age is a risk factor for regrowth and recurrence of nonfunctioning pituitary macroadenomas: results from a single Australian centre. Clin Endocrinol (Oxf) 87(3):264–271. https://doi.org/10.1111/cen.13365
Ezzat S, Asa SL, Couldwell WT, Barr CE, Dodge WE, Vance ML et al (2004) The prevalence of pituitary adenomas. Cancer 101(3):613–619. https://doi.org/10.1002/cncr.20412
Mete O, Cintosun A, Pressman I, Asa SL (2018) Epidemiology and biomarker profile of pituitary adenohypophysial tumors. Modern Pathol 31(6):900–909. https://doi.org/10.1038/s41379-018-0016-8
Chacón Aponte AA, Durán Vargas EA, Moscote Salazar LR (2021) Epidemiología de los adenomas hipofisarios: una vista de américa latina y el mundo. Neurociencias J 28(3):45–68
Aldahmani KM, Sreedharan J, Ismail MM, Philip J, Nair SC, Alfelasi M et al (2020) Prevalence and characteristics of sellar masses in the city of Al Ain, United Arab Emirates: 2011 to 2016. Ann Saudi Med 40(2):105–112. https://doi.org/10.5144/0256-4947.2020.105
Sarmiento JG, Aguirre LC, Valero LJ, Saiz DK, Aparicio KD, Sanabria JL et al (2019) Caracterización de los hallazgos histopatológicos de tumores hipofisiarios y de la región selar en dos centros en Bucaramanga, Santander, entre 1992 y 2018. Revista Endocrino 6(1):30–34. https://doi.org/10.53853/encr.6.1.465
AlMalki MH, Ahmad MM, Brema I, AlDahmani KM, Pervez N, Al-Dandan S et al (2020) Contemporary management of clinically non-functioning pituitary adenomas: a clinical review. Clin Med Insights Endocrinol Diabetes 13:1179551420932921. https://doi.org/10.1177/1179551420932921
Freda PU, Bruce JN (2010) Risks of pituitary surgery in the elderly. Nat Rev Endocrinol 6(11):606–608. https://doi.org/10.1038/nrendo.2010.170
de Almeida Holanda MM, de Melo CIE, de Queiroz MYCF, da Silva TS, da Franca Pereira MA (2016) Perfil epidemiológico dos tumores de hipófise e avaliação dos resultados cirúrgicos na cidade de João Pessoa. Revista Saúde & Ciência Online 5(3):22–31
Stalldecker G, Ballarino C, Diez S, Mallea-Gil MS (2019) Adenomas hipofisarios en pacientes añosos. MEDICINA (Buenos Aires) 79(3):191–196
Solari D, Pivonello R, Caggiano C, Guadagno E, Chiaramonte C, Miccoli G et al (2019) Pituitary adenomas: what are the key features? What are the current treatments? Where is the future taking us? World Neurosurg 127:695–709. https://doi.org/10.1016/j.wneu.2019.03.049
Slavinsky P, Cervio A, Sevlever G, Arakaki N, Antico J, Katz D (2018) Adenomas no funcionantes: análisis retrospectivo de 202 pacientes. Rev Argent Endocrinol Metab 55(2):11–20
Tjörnstrand A, Gunnarsson K, Evert M, Holmberg E, Ragnarsson O, Rosén T et al (2014) The incidence rate of pituitary adenomas in western Sweden for the period 2001–2011. Eur J Endocrinol 171(4):519–526. https://doi.org/10.1530/eje-14-0144
Raappana A, Koivukangas J, Ebeling T, Pirilä T (2010) Incidence of pituitary adenomas in Northern Finland in 1992–2007. J Clin Endocrinol Metab 95(9):4268–4275. https://doi.org/10.1210/jc.2010-0537
Nilsson B, Gustavsson-Kadaka E, Bengtsson B-A, Jonsson B (2000) Pituitary adenomas in Sweden between 1958 and 1991: incidence, survival, and mortality1. J Clin Endocrinol Metab 85(4):1420–1425. https://doi.org/10.1210/jcem.85.4.6498
García Iñiguez JD, Barahona Ulloa WF (2018) Características de adenomas hipofisarios en el Hospital José Carrasco Arteaga”. Cuenca, 2012–2016.: Universidad de Cuenca
Daly AF, Rixhon M, Adam C, Dempegioti A, Tichomirowa MA, Beckers A (2006) High prevalence of pituitary adenomas: a cross-sectional study in the province of Liege, Belgium. J Clin Endocrinol Metab 91(12):4769–4775. https://doi.org/10.1210/jc.2006-1668
Fernandez A, Karavitaki N, Wass JA (2010) Prevalence of pituitary adenomas: a community-based, cross-sectional study in Banbury (Oxfordshire, UK). Clin Endocrinol 72(3):377–382. https://doi.org/10.1111/j.1365-2265.2009.03667.x
Salami A, Malomo AO, Shokunbi T, Akang E (2013) Immunohistochemical analysis of pituitary adenomas in a West African hospital. Afr J Neurol Sci 32(2):72–80
Gruppetta M, Mercieca C, Vassallo J (2013) Prevalence and incidence of pituitary adenomas: a population based study in Malta. Pituitary 16(4):545–553. https://doi.org/10.1007/s11102-012-0454-0
Aljabri KS, Bokhari SA, Assiri FY, Alshareef MA, Khan PM (2016) The epidemiology of pituitary adenomas in a community-based hospital: a retrospective single center study in Saudi Arabia. Ann Saudi Med 36(5):341–345. https://doi.org/10.5144/0256-4947.2016.341
da Cunha MLV, da Cunha MLV, Veríssimo DCA, Rehder R, Borba LAB, Boguszewski CL (2014) Ocorrência de adenomas pituitários correlacionados a idade e sexo em centros de referências para tratamento neurocirúrgico de patologia selar. Arquivos Brasileiros de Neurocirurgia Braz Neurosurg 33(01):13–16. https://doi.org/10.1055/s-0038-1626193
Day PF, Loto MG, Glerean M, Picasso MFR, Lovazzano S, Giunta DH (2016) Incidence and prevalence of clinically relevant pituitary adenomas: retrospective cohort study in a Health Management Organization in Buenos Aires, Argentina. Arch Endocrinol Metab 60:554–561
Osamura R, Grossman A, Korbonits M, Kovacs K, Lopes M, Matsuno A et al (2017) WHO classification of tumours of endocrine organs. IARC Lyon, France
Kizilgul M, Duger H, Nasiroglu NI, Sencar E, Hepsen S, Akhanli P et al (2022) Efficacy of cabergoline add-on therapy in patients with acromegaly resistance to somatostatin analogs treatment and the review of literature. 66(3):278–285. https://doi.org/10.20945/2359-3997000000481
Rindi G, Mete O, Uccella S, Basturk O, La Rosa S, Brosens LAA et al (2022) Overview of the 2022 WHO classification of neuroendocrine neoplasms. Endocr Pathol 33(1):115–154. https://doi.org/10.1007/s12022-022-09708-2
Drummond JB, Ribeiro-Oliveira Jr A, Soares BS (2018) Non-functioning pituitary adenomas. Endotext web
Chen Y, Wang CD, Su ZP, Chen YX, Cai L, Zhuge QC, Wu ZB (2012) Natural history of postoperative nonfunctioning pituitary adenomas: a systematic review and meta-analysis. Neuroendocrinology 96(4):333–342. https://doi.org/10.1159/000339823
Lenders N, McCormack A (2018) Malignant transformation in non-functioning pituitary adenomas (pituitary carcinoma). Pituitary 21(2):217–229. https://doi.org/10.1007/s11102-017-0857-z
Kuo JS, Barkhoudarian G, Farrell CJ, Bodach ME, Tumialan LM, Oyesiku NM et al (2016) Congress of neurological surgeons systematic review and evidence-based guideline on surgical techniques and technologies for the management of patients with nonfunctioning pituitary adenomas. Neurosurgery 79(4):E536–E538. https://doi.org/10.1227/neu.0000000000001390
Castellanos-Bueno R, Abreu-Lomba A, Buitrago-Gómez N, Patiño-Arboleda M, Pantoja-Guerrero D, Valenzuela-Rincón A et al (2021) Clinical and epidemiological characteristics, morbidity and treatment based on the registry of acromegalic patients in Colombia: RAPACO. Growth Hormone IGF Res. 60:101425. https://doi.org/10.1016/j.ghir.2021.101425
Katznelson L, Laws ER Jr, Melmed S, Molitch ME, Murad MH, Utz A et al (2014) Acromegaly: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 99(11):3933–3951. https://doi.org/10.1210/jc.2014-2700
Shanik MH, Cao PD, Ludlam WH (2016) Historical response rates of somatostatin analogues in the treatment of acromegaly: a systematic review. Endocr Practice 22(3):350–356. https://doi.org/10.4158/ep15913.Ra
Nieman LK, Biller BM, Findling JW, Murad MH, Newell-Price J, Savage MO et al (2015) Treatment of Cushing’s syndrome: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 100(8):2807–2831. https://doi.org/10.1210/jc.2015-1818
Pivonello R, De Martino MC, De Leo M, Simeoli C, Colao A (2017) Cushing’s disease: the burden of illness. Endocrine 56(1):10–18. https://doi.org/10.1007/s12020-016-0984-8
Störmann S, Schopohl J (2018) New and emerging drug therapies for Cushing’s disease. Expert Opin Pharmacother 19(11):1187–1200. https://doi.org/10.1080/14656566.2018.1504021
Kreutzer J, Buslei R, Wallaschofski H, Hofmann B, Nimsky C, Fahlbusch R et al (2008) Operative treatment of prolactinomas: indications and results in a current consecutive series of 212 patients. Eur J Endocrinol 158(1):11–18. https://doi.org/10.1530/eje-07-0248
Mann WA (2011) Treatment for prolactinomas and hyperprolactinaemia: a lifetime approach. Eur J Clin Invest 41(3):334–342. https://doi.org/10.1111/j.1365-2362.2010.02399.x
Melmed S, Casanueva FF, Hoffman AR, Kleinberg DL, Montori VM, Schlechte JA et al (2011) Diagnosis and treatment of hyperprolactinemia: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 96(2):273–288. https://doi.org/10.1210/jc.2010-1692
Chen L, White WL, Spetzler RF, Xu B (2011) A prospective study of nonfunctioning pituitary adenomas: presentation, management, and clinical outcome. J Neurooncol 102(1):129–138. https://doi.org/10.1007/s11060-010-0302-x
Molitch ME (2017) Diagnosis and treatment of pituitary adenomas: a review. JAMA 317(5):516–524. https://doi.org/10.1001/jama.2016.19699
Woodmansee WW, Carmichael J, Kelly D, Katznelson L (2015) American Association of Clinical Endocrinologists and American College of Endocrinology Disease State Clinical Review: postoperative management following pituitary surgery. Endocr Pract 21(7):832–838. https://doi.org/10.4158/EP14541.DSCR
Pelsma ICM, Verstegen MJT, de Vries F, Notting IC, Broekman MLD, van Furth WR et al (2020) Quality of care evaluation in non-functioning pituitary adenoma with chiasm compression: visual outcomes and timing of intervention clinical recommendations based on a systematic literature review and cohort study. Pituitary 23(4):417–429. https://doi.org/10.1007/s11102-020-01044-0
Ramírez C, Cheng S, Vargas G, Asa SL, Ezzat S, González B et al (2012) Expression of Ki-67, PTTG1, FGFR4, and SSTR 2, 3, and 5 in nonfunctioning pituitary adenomas: a high throughput TMA, immunohistochemical study. J Clin Endocrinol Metab 97(5):1745–1751. https://doi.org/10.1210/jc.2011-3163
Acknowledgements
Thank you to the endocrinology, statistics, and pathology departments of San José Hospital in Bogotá, Colombia, which allowed us to access the information, and Odds Epidemiology for the support in the editorial process.
Funding
None.
Author information
Authors and Affiliations
Contributions
CEJC and WR were directly involved to the conception and design of the work. CECJ, ST, DA and IR collected the data and were involved in the revision of the manuscript drafts. CEJC, WR, DA, IR, ST and LAVZ wrote the manuscript and contributed to critical review of the manuscript drafts, analysis and interpretation of data for the work with the assistance of RM and AC towards finalization. CEJC is the guarantor of the paper. We confirm that all authors read and approved the final manuscript. We further confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We confirm that the manuscript has been submitted solely to this journal and is not published, in press, or submitted elsewhere.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare no competing interests.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this study, formal consent is not required, the HSJ provided institutional informed consent prior to use of the data from medical records.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jimenez-Canizales, C.E., Rojas, W., Alonso, D. et al. Clinical presentation and recurrence of pituitary neuroendocrine tumors: results from a single referral center in Colombia. J Endocrinol Invest 46, 2275–2286 (2023). https://doi.org/10.1007/s40618-023-02080-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02080-w