Abstract
Families of children with disabilities in rural areas face challenges accessing services due to location and lack of health-care providers. Telehealth-based intervention can mitigate challenges in accessing services. The present study sought to replicate and extend the telehealth-based, behavioral parent-training program, the Online and Applied System for Intervention Skills (OASIS), utilizing a multiple-baseline approach. Four parent–child dyads participated, with all children diagnosed with autism spectrum disorder. All dyads resided in rural/underserved areas. All dyads demonstrated an improvement on skill and knowledge assessments. The mean gain from baseline-to-treatment completion on skills assessments was 80.9% (range: 67.6%–95.5% points). The mean gain on knowledge assessments was 35.3% (range: 19.0%–49.0% points). It should be noted that parent skill gains were maintained over time. The present results provided additional empirical evidence demonstrating the effectiveness of OASIS, a telehealth-based parent-training model.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Roughly 97% of the landmass in the United States is designated as rural, yet only 19% of the population (approximately 60 million people, or 1 in 5 Americans) live in rural areas (U.S. Census Bureau, 2010). When compared to those living in urban areas, individuals living in rural areas tend to suffer more adverse health outcomes and engage in more unhealthy behaviors (Befort et al., 2012; Boring et al., 2017; Cossman et al., 2017). Disparities in care exist for children with autism spectrum disorder (ASD) in rural locations beginning with diagnosis (Antezana et al., 2017), with some states reporting both child location in the state and availability of services in their location as crucial challenges in service delivery (Mauch et al., 2011). In addition, Mello et al., (2016) found that only 44.2% of surveyed rural families had any applied behavior analytic (ABA) services for their child with ASD, compared to 51.4% of nonrural families. Furthermore, only 59.6% of rural children had home-based behavior support when compared to 82.2% of urban children. In order to ameliorate disparities in treatment and outcomes, telehealth services have begun bridging the gaps by bringing professionals to rural areas through technological means.
Telehealth services (for the purposes of this article) are synchronous services delivered to individuals separated from providers by physical distance via an internet connection that allows for video and audio communication. A variety of telehealth-based studies specifically related to ASD have been conducted. Telehealth use has increased for varied professions, including ABA services, with the onset of the COVID-19 pandemic (Koonin et al., 2020). The increase in use of telehealth-delivered ABA services also prompted the Council of Autism Service Providers (2021) to delineate guidelines to assist practitioners in practicing in an effective and ethical manner following the expansion of telehealth coverage.
Ferguson et al., (2019) conducted a systematic review of literature pertaining to telehealth and ABA, finding that 100% of reviewed studies (n = 28) indicated positive outcomes in relation to identified participants. The authors further stated that research related to comprehensive treatment packages delivered via telehealth is an underdeveloped area. Within a randomized controlled trial design, Lindgren et al., (2020) utilized a telehealth-delivery model for teaching parents to use functional communication training to reduce problem behavior displayed by their children. Results indicated increases in functional communication, decreases in moderate to severe child problem behavior, and high treatment acceptability only following implementation of functional communication training. Changes in important behavioral outcomes (e.g., increased child skill, increased parent skill) following both in-person parent training and online parent training are apparent (e.g., Crone & Mehta, 2016; Fisher et al., 2020; Jang et al., 2012; Koegel et al., 2002). Telehealth training, similar to in-person parent training, has also focused on training specific programs or models (as seen in Solomon et al., 2008), as well as training general components of early intervention procedures (e.g., Crone & Mehta, 2016). A recent study by Fisher et al., (2020) assessed the utility of a virtual parent-training program in a randomized clinical trial. Authors utilized online modules in addition to scripted role play situations to teach and evaluate implementation of skills displayed by parents. Authors found high parent satisfaction as well as statistically significant improvements in parents in the intervention group (compared to the waitlist control group). Overall, research on telehealth practices, increased internet access, and increased availability of electronic tools (e.g., computer-based cameras, video capabilities, and even cellular phones) have made dissemination of evidence-based practice to rural areas much more reasonable. Given the essential nature of effective parent training in ABA services (Jang et al., 2012), research on virtually delivered, comprehensive training has become crucial.
One parent-training model that was developed for delivery via telehealth is the Online and Applied System for Intervention Skills parent training program (OASIS; Heitzman-Powell et al., 2014). The OASIS program is a holistic approach to parent training that teaches parents both basic skills (e.g., reinforcement, prompting) and behavioral concepts/principles (e.g., functions of behavior, extinction) to utilize and understand when working with their child (see Heitzman-Powell et al., 2014, Table 1, for a breakdown of module goals and content). In addition, the OASIS training program addresses currently identified gaps in the telehealth literature, such as teaching discrete trial instruction (Ferguson et al., 2019) as a component of intervention. OASIS was designed for telehealth delivery to reach a wider range of parents who might otherwise not contact evidence-based treatment services for their children due to their location.
Heitzman-Powell et al. (2014) provided the OASIS training to a total of seven parents across four families. The parents’ education levels ranged from a high school diploma to graduate degree. All parents were required to complete online training modules and online coaching sessions. Parents were taught specific behavioral techniques and were required to correctly utilize those skills prior to progressing through training. Parents completed the online activities before scheduled telehealth-delivered coaching sessions. Children were present for all telehealth-delivered coaching sessions. Gains across all skills averaged 41.2% (range: 28.0%–59.0%) for all participants. Knowledge gains on a 48-item assessment averaged 39.1% (range: 12.5%–90.0%) for all participants. Parents also reported their satisfaction with the training program, indicating overall that each major component of training (i.e., online modules and telehealth coaching sessions) was both important and satisfactory. Moreover, the researchers calculated that the use of telehealth procedures saved the participants from driving a total of 9,052 miles total across all live coaching sessions. Implications of the study are clear: parents can be effectively and efficiently trained to conduct basic procedures of ABA with their child with autism via a structured telehealth training program. In addition, allowing parents to access the full training remotely saves time and resources. Despite the promising outcomes from the original study, limitations were apparent. In particular, parents were required to drive from their home to a telehealth site instead of having access directly from home, and parent outcomes were reported as overall changes in parent behavior (pre/post-assessment) rather than as gradual changes over time (repeated measures of parent behavior throughout the course of participation).
The purpose of the present study was to replicate and extend the findings of Heitzman-Powell et al., (2014) that demonstrated increases in parent knowledge and skills following completion of the OASIS parent-training program. In particular, the present study replicated and extended methodology of the seminal OASIS study (Heitzman-Powell et al., 2014) with parents who resided in rural or service-impoverished geographic locations by (1) delivering the program to parents in their own homes via telehealth (rather than at a remote site) and (2) measuring parent behavior change (i.e., comprehensive skill assessment) throughout training within a repeated measures design (rather than solely pre-/post-data).
Methods
Participants
Parent–child dyads were considered eligible for participation if the following criteria were met: (1) the child in the dyad was diagnosed with an ASD; (2) the primary parent had not previously received structured parent training (e.g., any training with a behavior analyst or autism specialist, coursework or online work specifically reviewing ABA concepts, individualized instruction with their child); (3) the parent(s) and child were available for a 1.5-hr meeting per week for 16–21 weeks; (4) the parent had access to the internet and a device (e.g., tablet, laptop) capable of running a video chat application; (5) the child was between the ages of 2–13 years; and (6) the child was not currently receiving home or clinic based ABA therapy (to ensure additional learning did not occur outside of OASIS sessions). Although the requirement for the child to not be engaged in home or clinic-based services was limiting for the family, none of the participants who were recruited had access to ABA services for their child during the timeframe in which they completed the study. Parents were asked to not speak to other research participants about the training program or their progress.
Participants (a parent and child dyad) were recruited from rural areas (as indicated by the U.S. Census Bureau, 2010), or areas that had decreased access to services due to their geographic location (locations with one or less service provider and no access to immediate services). Recruitment was conducted in a variety of ways. First, an agency that provided ABA services and diagnostic assessments in rural and underserved areas of Kansas contacted families that were on their waitlist (agreeing or declining to participate did not affect their position on the waitlist for comprehensive services, except for the family being informed that they were not permitted to have comprehensive home-based services during the study). Parents whose children were evaluated in the agency’s diagnostic clinic were also given information for participation at the same time they were given a referral packet. Second, flyers were distributed via social media and in Kansas and Southern Illinois based groups (e.g., parent support groups, autism networks). Potential participants contacted the researcher via email and were then screened for eligibility via a Zoom meeting and/or email. During the screening, families were required to provide documentation of their child’s autism diagnosis and confirm they had never received parent training in the past (see inclusion criteria below). Each family’s physical location was also reviewed to ensure they met the rural and/or underserved area qualification. After determining eligibility, informed consent included a meeting via telehealth with the parent and the researcher to review all components of the study, including assessments, time commitments, training requirements, and meeting times.
Dyad 1 consisted of a 5-year-old boy (Kal) and his mother (Lyanne; 30 years old). They lived in a rural area, with Lyanne reporting that she did not know where to access services. They heard about the study via a local parent support group. Lyanne was white, had an associate’s degree, was married, and both spouses earned an income totaling $66,000–$75,000 per year. Kal attended a local preschool program where he received special education services. He was a nonvocal communicator (he only clearly vocalized and repeated a limited number of words) and utilized an iPad with a communication application to communicate with others. Per parent report, Kal engaged in very limited problem behaviors (e.g., get upset, cry); however, over the course of training it was observed that Kal frequently screamed, cried, and protested when demands (including low response effort demands) were placed on him. His problem behavior occurred at an intensity and frequency that was problematic (per parent report) in the household and consistently interfered with his participation in a variety of daily tasks.
Dyad 2 consisted of a 2-year-old boy (Benjy) and his mother (Shay; 29 years old). They lived in an area with only one service provider and limited access to resources, with Shay reporting that they were on a waitlist for in-home services with an agency that was approximately 45 min away (one way). The family heard about the study via a diagnostic clinic (the same agency where they were on a waitlist). Shay was white, had a master’s degree, was married, and both spouses earned an income totaling $96,000–$105,000 per year. Benjy attended an in-home daycare but had previously been dismissed from other center-based daycare settings due to problem behavior, specifically biting his peers. He communicated vocally but had a very limited repertoire for spoken language and other modes of communication (i.e., gestures, simple signs). Most of his language was limited to simple one-word requests with full words or approximations. Benjy was reported to engage in a variety of problem behaviors, including aggression (e.g., hitting, biting), property destruction (e.g., throwing toys), tantrum behaviors (e.g., screaming, crying, flopping on the floor), and other general task refusals (e.g., saying “no,” leaving the teaching area, laying on the floor instead of working).
Dyad 3 consisted of a 4-year-old boy (Jorah) and his mother (Rose; 43 years old). They lived in a rural area, with Rose reporting that they were on a waitlist for in-home services with an agency approximately 2 hr away (one way). They heard about the study via a local parent support group. Rose was white, had a high school diploma, was married, and both spouses earned an income totaling $56,000–$65,000 per year. Jorah attended a local preschool program where he received special education services. He was a vocal communicator with some language delays and articulation errors; however, his language repertoire was similar to same-aged peers and familiar adults and family members were able to understand what he said. Rose reported that Jorah escalated if he was unable to make his meaning clear when attempting to communicate. Jorah engaged in a variety of varying intensity problem behaviors, including tantrums (e.g., screaming, yelling, crying, dropping to the floor, physical resistance to prompting, elopement) and general noncompliant behavior throughout his day (e.g., arguing with parents and caregivers, verbal refusal to follow instructions), with some instances of problem behavior lasting 20 or more min.
Dyad 4 consisted of a 3-year-old girl (Kalee) and her mother (Sasha; 39 years old). They lived in a rural area, with Sasha reporting that she did not know where to access services. They heard about the study via Lyanne from Dyad 1. Sasha was Asian, had some college, was single, and had a single income household of less than $10,000 per year. Kalee attended a local preschool program where she received special education services. She was a nonvocal communicator and was waiting for an iPad with a communication application (LAMP Words for Life) at the onset of the study. Sasha reported that she knew what Kalee wanted based on gestures and some very simple sign language (e.g., milk, eat). Kalee was reported and observed to engage in a variety of problem behaviors, including skin scratching/picking, nail biting, crying, and task refusal (e.g., wafting hand at materials or tasks, crying and nonresponding).
Setting
Participants were encouraged to use the same room of their home and the same devices for all coaching sessions. Dyad 1 completed sessions in their dining room or in the child’s bedroom, Dyad 2 completed sessions in the child’s bedroom, Dyad 3 completed sessions in a small room dedicated to instruction, and Dyad 4 completed sessions in the child’s bedroom. Family participants were encouraged to have a quiet and dedicated environment to minimize distractions and potential interruptions, but interruptions from other family members (e.g., siblings, spouses) or for child needs (e.g., toileting, snacks) occurred frequently throughout live coaching sessions.
OASIS Materials
Parent Materials
Parent materials included online tutorials, printed data sheets for incidental teaching and problem behavior information, and a parent binder that contained information related to each coaching session (e.g., materials needed, content covered). Online materials were available through a variety of platforms (e.g., phone, tablet), locations, and times allowing for easy access for the parents. The online materials were broken into eight modules. All coaching sessions between the researcher and parent–child dyads were conducted via a Zoom account that met Health Insurance Portability and Accountability Act (HIPAA) compliance standards. In total, training required a minimum of 15 Zoom-based coaching sessions, with one coaching session for all of Module 1, and two coaching sessions for the remainder of the modules (e.g., Module 2’s Zoom-based coaching sessions were broken into “Module 2.1” and “Module 2.2”).
Child Materials
Materials for child participants included various toys, preferred items, and materials related to tasks (e.g., cause and effect, blocks). Materials for each child varied based on their preferences, skill level, and available resources of the family.
OASIS Coach and Coach Materials
The first author worked with each parent–child dyad for all baseline, training, and follow-up sessions. Sessions were conducted from the same computer each time. The researcher had both the OASIS Coach Protocol (a booklet that contained scripts and prompts) and the family’s assessment protocol (a booklet that contained data collection sheets for parent behaviors and general training requirements). The researcher also had access to the OASIS online platform in which parents took quizzes and submitted problem behavior recording forms (PBR) and incidental teaching checklists (ITC).
Dependent Variable
Comprehensive Skill Assessment
A comprehensive skill assessment, that measured 13 overall parent target skills taught throughout training, functioned as the primary dependent measure (see Table 1 for specific target skills and the number of included micro skills) and provided a granular analysis of parent behavior. Target skills were operationally defined in individual micro skills for scoring purposes. The number of micro skills varied on each skill. The comprehensive skill assessment included a total of 67 individual micro skills across 13 target skills. The setup of the comprehensive skill assessment allowed for repeated measures on parent target skills as training progressed and provided a method of reviewing not only performance on overall hands-on target skills but also performance on the individual micro skills required for overall target skills (e.g., if a parent scored less than 100% on target skills, such as a preference assessment, the first author reviewed which individual micro skills of the target skill were being missed). Comprehensive skill assessments were conducted less frequently during baseline (i.e., probes) to reduce response effort and frustration for parents. During intervention, comprehensive skill assessments occurred on a biweekly basis after every other intervention session (i.e., following the meetings for Modules 2.1, 3.1, 4.1, 5.1, 6.1, 7.1, and 8.1), for a total of seven measurements of the primary dependent variable during intervention.
Lay terms were used when prompting the parents to engage in each activity during the skills assessment to reduce confusion related to the technical language the parent learned during training. For example, instead of saying “show me a preference assessment,” the researcher said, “show me how you would find something that your child would work for or earn.” Parents were observed after each prompt and if they engaged in any micro skill of the target skill being assessed a “+” was recorded on the data sheet. After the parent indicated they were finished or stopped responding for approximately 10 s, the researcher scored any micro skills that were not exhibited or exhibited incorrectly as a “-” and moved on to the next target skill. Scores were calculated by taking the total number of correctly completed micro skills across all 13 target skills divided by total possible micro skills (67) across all 13 target skills and multiplied by 100%.
Knowledge Assessment
A knowledge assessment was also provided to parents during each skills assessment and functioned as a secondary dependent variable. Knowledge assessments were an online test administered through an online survey platform (Qualtrics) that randomly pulled 60 questions from an overall pool of 159. The question pool contained all possible questions that had been developed for the existing OASIS online module quizzes (i.e., the quizzes the parents were required to take in the online modules/system). Questions from the OASIS modules were based off the information presented in each module. In addition, the pool of questions was the same pool of questions utilized in the OASIS pre- and posttest embedded in the training. Knowledge assessments were conducted less frequently during baseline (i.e., probes) to reduce response effort for parents. During intervention, knowledge assessments occurred on a biweekly basis after every other intervention session (i.e., following the meetings for Modules 2.1, 3.1, 4.1, 5.1, 6.1, 7.1, and 8.1), for a total of seven measurements of the secondary dependent variable during intervention. Scores were calculated automatically by Qualtrics by taking the total number of correctly answered questions divided by the total number of questions presented (60) and multiplied by 100%.
Interobserver Agreement
Interobserver agreement (IOA) was collected via video review for 43.0% of all opportunities in baseline, intervention, and follow-up for the comprehensive skills assessment across all four dyads. IOA was calculated on the comprehensive skill assessment by totaling the number of items to be scored in which two raters had an agreement, divided by the total number of items to be scored, and multiplied by 100%. The average IOA for the comprehensive skills assessments were as follows: Dyad 1 at 92.0% (range: 82%–100.0%), Dyad 2 at 93.0% (range: 81.0%–97.0%), Dyad 3 at 85.0% (range: 81.0%–88.0%), and Dyad 4 at 88.0% (range: 82%–100%).
For the knowledge assessments, IOA was calculated for 43.0% of all opportunities in baseline, intervention, and follow-up across all four dyads. IOA was calculated on the knowledge assessment by two raters checking both the accuracy of the calculated score from the Qualtrics report and the accuracy of the score being transferred onto the graphs. The average IOA for the knowledge assessment was 100% across all reviews and all dyads.
Experimental Design
A concurrent multiple baseline across parent–child dyads was used in the present study. A multiple baseline design across participants has been used frequently in other parent-training studies (e.g., Vismara et al., 2012; Vismara et al., 2013; Wainer & Ingersoll, 2013, 2015) though single subject data were not published on the seminal OASIS study. Weeks on the x-axis represent concurrent weeks from September 2019 (start of baseline for Dyad 1) until June 2020 (final follow-up for Dyad 4). Parent training sessions occurred once per week and typically occurred on the same day of the week and at the same time unless a parent requested to reschedule. Dyad 4 was recruited later than other dyads; therefore, Dyad 4’s baseline sessions do not overlap with Dyad 3’s baseline sessions.
OASIS Procedures
OASIS Coach Information
OASIS is a highly structured, manualized training program conducted by trained coaches. Coaches were trained to criterion utilizing a behavioral skills training model delivered at the University of Kansas Medical Center, where the OASIS parent training was developed. Coach training consisted of 40 hr of instruction and hands-on skill practice with feedback. Coaching sessions were scripted and manualized to ensure necessary content was reviewed with parents and to ensure consistent delivery across participants. Live coaching session information was contained in a booklet (OASIS “Coach Protocol”), with all scripts and information for each module and coaching session. A copy of a secondary booklet (“Assessment Protocol”) was provided to the coach for each family that participated in training. The Assessment Protocol served as the data sheet for each live coaching session and the booklet contained spaces for the coach to check off when specific activities were completed (e.g., check in, review of the online materials). Data collection on target skills being reviewed in each module were also located in the Assessment Protocol booklet. The coach was trained to use both booklets during the 40-hr training with 90% fidelity of implementation for all procedures (e.g., following the scripts, scoring parents accurately).
Parent Training Sequence
Parents were required to complete online modules that provided detailed information on techniques and strategies to be reviewed during live coaching sessions. Parents then attended scheduled live coaching sessions via Zoom. Due to the scripted nature of the training, parents followed the same sequence for live coaching sessions (see Table 2 for the general sequence of each live training session). For example, the beginning of Module 1 (Introduction to Autism and Behavioral Treatment) included a script of the goals for the session, a script to welcome the family to the session, a script to provide a brief overview of the session, prompts for the coach to review online materials, and prompts to engage in any hands-on activities. Although the scripted nature of the program attempted to limit variations in delivery of the training, the script cannot account for every aspect of a session, such as answering parent questions. Individualized content varied from participant to participant based on requests for additional information or questions.
Intake
Similar to Heitzman-Powell et al., (2014), varied intake measures were collected to determine if scores on each measure differed during intake and follow-up assessments based solely on the use of the OASIS program. Child intake measures included: The Childhood Autism Rating Scale-2 (CARS-2; Schopler et al., 1980), Vineland Adaptive Behavior Scales, Third Edition (Vineland-3; Sparrow et al., 2016), behavioral observations (parent checklist; child-parent interaction), Autism Treatment Evaluation Checklist (ATEC; Rimland & Edelson, 1999), and the Family Quality of Life (FQoL; Hu et al., 2011). Unlike Heitzman-Powell et al., (2014), the Child Behavior Checklist (CBCL; Achenbach, 1994) was added to the intake and follow-up measures. Basic demographic data were also collected.
Baseline
Parent dependent measures (comprehensive skill assessments and knowledge assessments) were collected during a small number of sessions (i.e., probes). Each baseline session lasted between 1.0 and 2.0 hr for the comprehensive skill assessment, dependent upon both parent preparedness and the child’s displays of problematic behavior. During the sessions, parents were presented with the prompts from the comprehensive skill assessment and asked to engage in each of the 13 target skills. For example, parents were told, “show me how you would find something that your child would work for or earn,” and then permitted time to respond as they felt appropriate. If they completed any of the micro skills under the “Preference Assessment” target skill, the micro skill was scored as a “+” on the data sheet by the first author. If they did not engage in steps or performed steps in error, the step was scored as a “-” on the data sheet by the first author. Parents were not provided with any feedback, prompts, or the results/scores of the assessments. The parent was permitted to request to end their time with each target skill. For example, one target skill prompt was for the parent to show the OASIS coach how to overteach something to their child. If the parent did not know what “overteach” meant, they were instructed to say “I don’t know” to move on to the next target skill prompt. Some encouragement was given to the parents by the OASIS coach saying something such as “try your best.” Following the end of the live baseline session, the parent was prompted to complete the knowledge assessment at their convenience and then emailed a direct link as an additional prompt.
Intervention
Intervention sessions for each parent–child dyad were scheduled once per week for 16–21 weeks for 1.5–2.0 hr per week and were conducted via Zoom (i.e., live coaching sessions). Each intervention session followed the same general pattern as outlined in the OASIS training materials (see above; e.g., OASIS Coach Protocol). There were two main components to each intervention session, including the parent preparation and the live coaching session.
For parent preparation, parents were required to complete one of the online modules (an interactive PowerPoint) and reach the mastery criterion (80%) on the online module’s knowledge assessment prior to each live coaching session. Online modules and content were completed at a time most convenient for the parent, with the only requirement being that they complete it prior to the scheduled coaching session (e.g., if the coaching session was Sunday at 5:00 pm, the parent was permitted to complete the online content by 4:59 pm). There were eight online modules in total, with two intervention sessions occurring for Modules 2–8. Therefore, parents completed Module 1 content and knowledge assessment prior to meeting for the Module 1.0 live coaching session and for subsequent modules, parents completed the online module content and knowledge assessment but attended two live coaching sessions (e.g., parents completed Module 2, but then attended Module 2.1 and Module 2.2 coaching sessions prior to completing Module 3 online, and so on). All preparation activities (e.g., the modules, problem behavior forms) typically take approximately 1 hr, depending on the parent’s speed and if they chose to review content more than once.
During live coaching sessions, the OASIS coach progressed through the scripted information (see Table 2, starting at Step 1). Each session began by greeting the parent and child, reviewing the overall session goals and general sequence (e.g., “We’ll start today by reviewing the online materials and talking through some concepts with just you, and then later we’ll get to activities and interactions with [child’s name]”). Next, the online materials (e.g., quiz, problem behavior forms) were reviewed, followed by a scripted review of the module content and information. Following the review of content, the live coaching session then moved on to hands-on skills training with the parent and child (see Table 3 for a list of hands-on skill activities scripted into each OASIS module) with three attempts or opportunities to practice the target skill. Hands-on skills training was individualized to each module, with one to three target skills being taught directly with behavioral skills training. Major target skills from the OASIS modules also comprised the comprehensive skills assessment (i.e., the dependent measure). Additional coaching for hands-on skills was conducted if the parent was not at a score of 80% following the initial training component. Parents progressed through training based on their progress and scores in training, rather than progressing based on their scores on the comprehensive skills assessment (i.e., dependent measure). The live coaching session then included a 5-min unstructured activity with the parent and child (e.g., rapport building and child-led playtime). The live coaching session closed with probing for parent questions, discussing the next module content, and confirming the next appointment time.
Data collection occurred in the “Assessment Protocol” booklet for each dyad across all activities included in the live coaching session (e.g., a spot to record an X to indicate that each step of training occurred as outlined was provided in the Assessment Protocol booklet). In addition, data were collected in the Assessment Protocol booklet for the hands-on skills training in each module, including data on the individual micro skills of each target skill being taught. A “+” was recorded for accurate responding and a “–“ was recorded for incorrect responding or failing to engage in the micro skill. The parent handbook contained suggested activities based on beginner, intermediate, and advanced child skills for parents to select or modify based on the child’s skill level. For example, a beginner skill was one-step gross motor imitation and an advanced skill was drawing specific shapes. Parents were permitted to choose an activity they felt appropriate or worked with the OASIS coach to choose a skill they felt valuable for their child. Hands-on practice of target skills required the parent to obtain 80% mastery across all opportunities and to engage in accurate responding at least once across every micro skill (e.g., scoring a “–“ on the same micro skill all three times prevented parents from moving on with training). If the parent failed to score an 80%, additional training was provided for the target skill. If parents were still unable to appropriately complete the materials for a module, a second intervention session for the same material was scheduled within the same week to provide another opportunity to reach criterion. Parents were allowed to request a second session for any of the modules. None of the four dyads required or requested a second session for any of the modules.
In between live coaching sessions, parents were also required to fill out information related to their child’s problem behavior during naturalistic times throughout their week (i.e., Problem Behavior [PBR] Recording forms) and information related to teaching opportunities they engaged in outside of the live coaching sessions (i.e., Incidental Teaching Checklists [ITC]). The PBR forms were utilized as additional training for the parents by reviewing problematic behaviors displayed by the child that occurred in between live coaching sessions. Reviewing the display of problematic behavior and parent responses allowed time to discuss potential strategies as well as how to incorporate information from the modules into their day-to-day activities to help prevent the occurrence of problem behavior. The ITC forms were also utilized as additional teaching on the use of target skills outside of live coaching sessions. The ITC forms also served the purpose of checking in on parent’s generalization of training materials to naturalistic situations.
Follow-up
Follow-up sessions occurred at 1-, 3-, and 5 weeks after training and were identical to baseline sessions for dependent measures, with one exception. Standardized assessment measures presented initially during the intake process (e.g., the Vineland-3, CARS-2, and CBCL) were administered at the end of first follow-up session.
Treatment Fidelity
An independent observer watched videos of the live coaching sessions and recorded whether the OASIS coach (i.e., the first author) completed each section of information in the training as designed to ensure fidelity of implementation of the intervention. The independent observer scored each element of the training session as a + for occurring and – for not occurring. The total number of items delivered during training was divided by the total number of items outlined in the training protocol and then multiplied by 100%. All four dyads had 33.0% of their live coaching sessions reviewed for treatment fidelity, with 100% treatment fidelity reported across all four dyads.
Social Validity
All parents were also asked to complete a brief social validity survey following completion of intervention. Social validity was collected by presenting 24 questions (e.g., “I would be willing to use this outside of the training sessions”; “This was an acceptable training program for my child’s problem behavior”) and asking the parent to rate how much they agreed with each statement on a Likert scale of 1–5 (1 = strongly disagree, 5 = strongly agree).
Time and Cost Savings
Time and cost savings were calculated in the same manner as Heitzman-Powell et al., (2014). The OASIS parent-training program is relatively new, with few practitioners trained and approved to deliver services. Time was calculated by taking the drive time from each dyad’s city of residence to the main office of the agency that provides OASIS parent training. Cost savings were calculated for the total cost of travel from each dyad’s city of residence to the main office of the agency that provides OASIS parent training by taking the total number of miles and multiplying by the 2019 Internal Revenue Service (IRS) rates of $.575/mile (IRS, 2019). Cost and time savings were calculated for each dyad’s round trip to the office location for every session they attended during the intervention portion of training.
Results
Comprehensive Skill Assessment
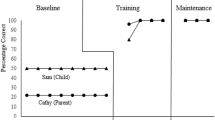
Scores for comprehensive skills checks for each dyad are displayed in Fig. 1. Overall, all four dyads demonstrated a gradual improvement in their use of target skills following the introduction of training. All four dyads had a sharp increase in scores from their final baseline to their first two data points in intervention, with three of the four dyads (Dyads 1, 3, and 4) accuracy decreasing slightly during the third (Dyad 3) or fourth (Dyads 1 and 4) intervention probes prior to continuing an upward trend for the remainder of intervention. Dyad 2 (e.g., Shay) was the only dyad to make continuous progress on an upward trend without evidence of skill regression. All four dyads’ accuracy peaked during the sixth intervention probe. During follow-up, three of the four dyads (Dyads 1, 2, and 3) showed stable and/or increasing maintenance. The fourth dyad (Dyad 4) showed stable maintenance during the first two probes before decreasing slightly during the third probe. All four dyads made gains in their applied skills over the course of training. The mean gain from the first baseline session to the first follow-up session was 80.9% (range: 67.6%–95.5%) Scores for pre- and post-comprehensive skill assessments are displayed in Table 4.
A secondary analysis of parent skill data was conducted by evaluating the scores on each target skill over time, as they occurred in the context of training. Although the primary dependent variable was the overall target skill score, an additional analysis of data is warranted given the present study sought to provide a preliminary but comprehensive analysis of the OASIS training program. As an example, Fig. 2 displays the data on each individual target skill for the parent in Dyad 2 (Shay) in the order in which the target skills were presented during live coaching sessions. Some target skills, such as reinforcement and structuring the environment, increased prior to the introduction of specific teaching; however, as previously noted, some micro skills in many target skills were likely prompted in a general manner during initial training sessions, leading to increases in scores prior to structured teaching on some of the target skills. For example, gaining attention may have been prompted during initial live coaching sessions to ensure the parent practiced a target skill, despite gaining attention not occurring as a micro skill until Module 3.2. The results displayed in Fig. 2 demonstrate skill acquisition and maintenance for targets that had not yet been introduced. In particular, during baseline Shay increased her scores on reinforcement and prompting (second panel) following stable low to moderate levels across four probes prior to the introduction of these target skills during live coaching sessions. Likewise, structuring the environment and attending (third panel) were variable or low during baseline initially, but then increased to 80%–100% accuracy prior to the introduction of these target skills during live coaching sessions. Skill acquisition was also observed for mass and interspersed trials (sixth panel) and overcorrection (eighth panel) following 0% accuracy across seven and eight probes, respectively, during baseline.
Similar results were observed for other participants during secondary analysis. Lyanne (Dyad 1) consistently displayed accuracy in reinforcement and attending behavior during baseline (the only two skills she displayed with 100% accuracy), which maintained at 100% accuracy in all dependent measure probes apart from one session for each target skill. In addition, Lyanne demonstrated an increase in accuracy with mass trial instruction, prompting, and structuring the environment prior to the introduction of structured teaching procedures. Roslin (Dyad 3) engaged in inconsistent accurate responding on target skills in baseline, except for teaching a new skill, which varied from 33% to 44%. During parent training, her accuracy across several target skills increased prior to the introduction of structured teaching procedures, including reinforcement, structuring the environment, generalization, mass trial instruction, interspersed trial instruction, and extinction. Sansa (Dyad 4) inconsistently displayed accuracy responding for all target skills throughout baseline. Similar to the other dyads, she demonstrated an increase in accuracy across a variety of target skills prior to their introduction in structured teaching procedures, including reinforcement, structuring the environment, attending, mass trial instruction, and extinction.
Knowledge Assessments
Scores for knowledge assessments (initial baseline data point, final data point in intervention, first data point in follow-up, and final data point in follow-up) are displayed in Table 4. All four parents displayed an increase in their knowledge from baseline and intervention, with sustained increases of at least 15% (range: 15%–56%) from the pretest to the final follow-up probe. The mean gain from pretest to the initial posttest was 35.3% (range: 19.0%–49.0%). Dyad 3 missed one knowledge assessment during intervention and Dyad 4 had multiple delays in completing knowledge assessments, leading to fewer assessments overall.
Pre- and Postintervention Standardized Assessments of Behavior Change
Data from pre- and postintervention standardized assessments of behavior change (e.g., CBCL, CARS-2) did not demonstrate any reliable changes in scores across all four child participants except for the ATEC, which can be used to monitor treatment efficacy and child progress over time. Scores on the ATEC changed in the expected direction for three of four child participants (Dyads 1–3, Kal, Benjy, Jorah), with a decrease in scores from pre- to postintervention for both the overall score and the four individual subscales of the ATEC. The fourth participant (Dyad 4, Kalee) was the only participant to have reported increases in the overall ATEC score, with stable data on two scores, an increase in scores on one subscale, and a decrease in scores on one subscale. Preintervention scores on the ATEC averaged 76.8 (range: 63.0–96.0), with scores of 63, 69, 79, and 96 for Dyads 1-4, respectively. Post-intervention scores averaged 62.3 (range, 39.0-106.0), with scores of 25, 49, 55, and 106 for Dyads 1–4, respectively. Decreasing scores on the ATEC for Dyads 1–3 suggested improvement in the parent-perceived level of concern on assessed behaviors, with the increasing score for Dyad 4 suggesting a worsening in the parent-perceived level of concern on assessed behaviors.
Social Validity
All four parents rated the OASIS program socially valid overall, with a total average score of 4.85/5.00. Dyad 1 (Lyanne) rated social validity at 4.83/5.00, Dyad 2 (Shay) rated social validity at 4.74/5.00, Dyad 3 (Rose) rated social validity at 4.83/5.00, and Dyad 4 (Sasha) rated social validity at 5.00/5.00. Parents rated all items at a 4 or 5 on the Likert scale, except for one item. “The training program is consistent with those I have used in the home setting” was scored a 3 by Dyad 1 and was marked “N/A” by Dyad 2. Dyad 1 had previously had birth-to-three services that did not incorporate a full parent training component.
Time and Cost Savings
Results for time and cost savings are displayed in Table 5. Intake, baseline, and follow-up were excluded in time and cost calculations for all four dyads because they do not occur during a parent-training only model. Three of the participants lived in the same town (Dyads 1, 3, and 4). The total round-trip mileage for Dyads 1, 3, and 4 was 242 miles. Dyads 1, 3, and 4 had 15 total sessions during intervention, requiring 3,630 miles total at a cost of $2,087.25, and 67.50 total hr of travel time (per dyad) if they had traveled to a treatment site. Dyad 2, the closest participant to the office location, had 16 total sessions during intervention. Travel costs required 1,504 miles total at a cost of $864.80, and 24 total hr of travel time if they had traveled to a treatment site.
Total time commitment from start to finish for participation in the study is important to note and is therefore included in Table 5 because cancellations for illness or holidays may affect how quickly parents progress through the entire training program. The OASIS program is designed to be completed in as little as 15 weeks. For the present study, the minimum number of weeks required for live coaching sessions was 15, with an additional 1 to 3 weeks of baseline, and 5 weeks of follow-up. In total, all parents should have completed the entire study in 21–23 weeks. Including baseline and follow-up measures, Dyad 1 required 29 calendar weeks to complete participation, Dyad 2 required 32 calendar weeks to complete participation, Dyad 3 required 31 calendar weeks to complete participation, and Dyad 4 required 26 calendar weeks to complete participation. Based on the number of baseline and follow-up sessions for each dyad, participation in the study took 8, 9, 8, and 3 additional weeks beyond the minimum number required for participation for Dyads 1–4, respectively. The additional weeks to complete the study resulted in increased total time commitments of 13%–39%.
Discussion
The present study replicated the primary outcomes of seminal research on OASIS. Most notable is that parent target skills increased to 80%–100% on comprehensive skills checks and were maintained at high levels for all four participants following treatment (see Fig. 1). Target skill gains in the present study (80.9%) were higher than the 2014 evaluation of OASIS (41.2%). Overall, parents were consistently able to implement necessary skills when working one-on-one with their child. This led to more productive teaching sessions and more potential for parent skill gains despite instruction and feedback being given via Zoom rather than in-person. Skill gains maintained following treatment for all four dyads, despite inconsistencies they may have displayed during treatment. The maintenance of these skills also ensured parents were able to continue effective treatment procedures in the absence of the OASIS coach, an important finding as many parents can be the main and most natural treatment provider for their child.
As dyads progressed through OASIS training modules their skill gains were demonstrated on comprehensive skills assessments. By the first comprehensive skill assessment in training, parents had completed the first module (Module 1: Introduction to Autism and Behavioral Treatment) and the first half of the second module (Module 2.1: Defining and Observing Behavior); however, neither module contained a target skill from the comprehensive skill assessment. The first target skill probed on the comprehensive skill assessment (preference assessment) was not introduced until Module 3.1: Principles of Behavior. At first, increases in comprehensive skill check scores did not come from the first few target skills taught during training (see Fig. 3 for data related to the first two skills). Parents were required to engage in structured activities with their child prior to Module 3.1, with micro skill gains likely occurring, which account for the increase in overall scores during the first comprehensive skills assessment conducted during intervention. Micro skills were the individual steps within each of the 13 target skills. For example, the target skill of “Teaching a New Skill” contained nine individual steps including gaining the child’s attention, giving the instruction in statement format once, and pairing praise with reinforcement. Although a parent was not taught how to teach a new skill in initial sessions, prompts to gain attention or deliver praise and reinforcers occurred as they began working with their child in the first few training sessions. Feedback received in those first few training sessions likely led to parent gains on micro skills, accounting for increases in their total comprehensive skill scores. Gains on micro skills occurred in several instances prior to the introduction of specific teaching to any target skill, such as “Teaching a New Skill.”
Results from the parent knowledge assessments replicated the gains observed in the 2014 evaluation of OASIS with a mean gain of 37.3 points in the present study and a mean gain of 39.1 points in the seminal publication (Heitzman-Powell et al., 2014). The online delivery of instructional modules was an effective method of increasing parent knowledge. Basic knowledge of procedures can facilitate hands on learning experiences, which appears to have occurred during training sessions. It should be noted that parents in all four dyads referenced specific information from the modules or by asking clarifying questions when attempting to implement skills directly with their child (e.g., stating what they had read and then asking how it applied to the task they were performing). Knowledge changes may also increase parental acceptance of behavioral procedures because they have been provided background information that explains why or how a particular skill or procedure is effective or important. Knowledge checks potentially served as a form of written instructions that may typically be seen in a behavior skills training model (e.g., Sarokoff & Sturmey, 2008), which may have facilitated skill gains on comprehensive skill assessments. Parent knowledge final scores were not as high as the final scores on skills, nor did knowledge scores maintain as well as the skills scores. Lower scores on the knowledge assessment may have been due to a variety of factors, including inattention during the online test, lack of generalization of the questions from the format of the modules to the format of the online test, testing environment, or the parents general test taking skills and behaviors. The highest knowledge assessment scores were seen with Dyad 2 (Shay), who also had the highest education level (graduate degree). Despite the lower knowledge scores, parents all increased their fluency in applying skills and maintained their ability to implement behavior-analytic strategies at follow-up measures. Low knowledge scores are likely to not have as great an impact because low skill scores because the parents are far more likely to engage in activities related to their hands on skills on a consistent basis then to apply general knowledge and background information.
The present study had two important differences compared to Heitzman-Powell et al., (2014). First, the present study was conducted with parents located in their homes and using personal electronic devices, rather than the parents being required to drive to a telehealth-capable site. Remaining in their homes for training was of particular importance given that they lived in rural or underserved areas and treatment locations were up to 2 hr, 10 min away (one way). The parents all had access to Zoom on their personal devices and were able to connect with the OASIS coach consistently. Parents were able to successfully access online training, resulting in significant behavior change, by use of iPads or desktop computers (live coaching sessions occurred via tablet or cell phone). This increased accessibility of OASIS training is important for individuals living in rural and remote areas because travel may be a barrier to treatment access. Second, rather than an analysis of pre/post skill data, the present study utilized a granular measure of behavior change within a single-subject design (i.e., multiple baseline) by collecting data throughout the 16 weeks of parent training sessions. A granular measure of behavior change allowed for a more precise analysis of how parents developed and maintained their skills over time. In particular, although some variability occurred in skill acquisition, parent skills on all tasks consistently increased and maintained by the end of training and into the maintenance condition. The repeated measures analysis of the intervention allowed for more confidence that the intervention was effective because: (1) immediate increases in skills were observed when the intervention was introduced for each participant; (2) continued increases occurred throughout training; and (3) skill gains were maintained after treatment was terminated.
Implications for Clinicians
In a changing treatment landscape, telehealth has gained momentum as an alternative to face-to-face treatment and has continued to expand with the development of technology that increases accessibility, reaching larger pools of people in more underserved areas (e.g., Baggett et al., 2010). Given current global health concerns, telehealth has become an increasingly relevant issue for a variety of health professionals, with the CDC urging use of telework to mitigate community spread of illness (e.g., COVID-19; National Center for Immunization and Respiratory Diseases, 2020). Telehealth as a treatment delivery mechanism may also increase the reach and scope of behavior analytic services. Unfortunately, the use of telehealth in behavior analytic services lagged behind its use in other helping professions (Tomlinson et al., 2018), despite the benefits of increased access to treatment services, such as the use of telehealth to support and train parents. However, with the onset of the COVID-19 pandemic in 2020, the research related to telehealth feasibility and the available information regarding implementation of ABA services via telehealth has been on an increasing trend (Ellison et al., 2021).
Parents are a critical and integral part of their child’s treatment services (e.g., Jang et al., 2012) and research related to increasing their participation in their child’s treatment is critical, though some limitations have existed in reviews of parent training literature. In particular, Schultz et al., (2011) noted that only 3 of 30 reviewed studies mentioned teaching behavior analysis in particular. Furthermore, Ferguson et al., (2019) found that despite articles being related to behavior analysis and telehealth, only 7% indicated providing comprehensive knowledge and skills. The OASIS program offers the structure and support needed to teach parents how to provide behavior-analytic services effectively and efficiently to their child in the absence of other intervention options. The OASIS program also provides a more comprehensive approach to parent training, teaching skills across both behavior acquisition and behavior reduction, further filling a gap in the current literature.
Telehealth-based parent training has additional benefits for families. Travel time and cost savings from remaining at home for training can help offset the health-care costs of having a child with autism (estimated at $22,772 in Medicaid costs; Wang & Leslie, 2010). The families in the present experiment had cost savings of $864.80-$2,087.25 in travel costs alone for approximately 6 months of participation. Two parents had other children in the home during training times. Although at times they had to step away from training to engage the additional children in tasks or activities, there was minimal interference. Both parents were able to engage in training without requiring childcare for other children in their care, leading to not only more cost savings but also more flexibility in meeting with the researcher. Furthermore, the training is also provided in the child’s natural environment with their toys and items (not requiring generalization training in the home). In addition, parents accessed services while on a waitlist for additional services. Agencies that are unable to provide comprehensive services (e.g., lack of direct service providers, consultants with short-term availability) may turn to parent training as a means of providing services to wait listed families until other treatment options or slots open. Parent training via telehealth is particularly important in rural areas where there may be no in-person service options or long drive times to the nearest treatment location.
Limitations
Several limitations occurred throughout the study. First, multiple technical issues occurred throughout the course of the study. Zoom closed unexpectedly and a baseline video for Dyad 2 was lost; however, this issue only occurred once across all sessions. Related to this, background noise in the room with participants at times made it difficult to hear what was being said. During some of Dyad 3’s sessions, other people in the household were heard, making training more difficult. In addition, the audio was sometimes delayed due to background noise reduction features built into Zoom, resulting in the coach and parent occasionally talking at the same time. Technical issues may be fixed by providing families with materials they need to have stable audio and visual connections in place of using a cell phone or tablet that must connect wirelessly. Second, getting required paperwork to/from families was difficult. Some dyads printed and scanned information that was sent via email whereas other dyads required mailed paperwork to send back. Regardless of the method for paperwork transmission, some paperwork was lost. Families were also required to complete the majority of received paperwork on their own, rather than face-to-face with a clinician or the researcher.
Future Directions
Continued research on the generality of OASIS is necessary for reaching more families affected by autism in resource-low areas, but also in areas where resources may be available but subject to wait lists, age limits, and a myriad of other factors. Future research should include variations of replications such as outcomes across different clinicians, outcomes across different client ages, outcomes based on time spent in each training module, and outcomes across different delivery modalities. Furthermore, extensions of the current and existing research should include better monitoring of child-specific outcomes related to both skills and problem behaviors. In the end, child behavior change is the goal of parent training programs like OASIS, and child outcomes should be both included in studies and verified experimentally. With a limited amount of time to provide training (e.g., the 16–21 weeks of OASIS), immediate child changes may not be evident. Individual skill acquisition targets may lend themselves better to consistent data collection during sessions as opposed to problem behavior and pre-/postmeasures may be more reflective of actual behavior change if included during a long-term follow-up. For example, in the present study child problem behavior was displayed intermittently during baseline/training sessions and no clear pattern or trend was evident in any of the dyads. However, Dyad 1 (Lyanne) and Dyad 2 (Shay) reported that their child was easier to work with as the training progressed and they felt they were better able to get their child to attend to and complete tasks during training sessions as time progressed. The amount of time parents spent outside of sessions working with their child is also worth investigation, as Dyad 1 and Dyad 2 may have had more exposure to training activities if items were completed more regularly in between meetings with the OASIS coach. Furthermore, pre-/postmeasures of training (e.g., the Vineland-3 and ATEC) may not indicate meaningful changes in the typical timeframe in which OASIS is delivered, and more directly observable measures that can be both reliable and readily implemented via telehealth may be a necessary component of parent training.
Additional research should also focus on data collection and analyses focused on more granular measures of treatment effects, similar to the secondary analysis presented in the present study. Parent training is a comprehensive service with numerous variables that may contribute to behavior change. Furthermore, skill gains (such as those taught in the current study) are not independent of one another. Gains in some areas can increase skills in other areas. For example, increasing reinforcement by the parent may also increase their scores on presenting mass or interspersed trials when reinforcement is included as a step in the overall skill. A granular analysis will assist in parsing apart the effects from specific components of training and will allow researchers to gain a better understanding of how behavior changes within complex teaching technologies. Furthermore, skill deficits that are identified in the granular analysis can be remedied through changes in the OASIS curriculum.
Parents increased hands-on skills and knowledge after completing OASIS training. Parents and families in rural and remote areas also accessed critical services and gained a better understanding of evidence-based practices. The present results provided additional empirical evidence demonstrating the effectiveness of OASIS, a telehealth-based parent-training model. Amid growing health crises, increasing prevalence rates of autism, and a lack of qualified providers, telehealth and parent training are poised to create large-scale changes in how services are accessed and provided.
References
Achenbach, T. M. (1994). Child behavior checklist and related instruments. In M. E. Maruish (Ed.), The use of psychological testing for treatment planning and outcome assessment (pp. 517–549). Lawrence Erlbaum Associates. https://doi.org/10.4324/9781410610614
Antezana, L., Scarpa, A., Valdespino, A., Albright, J., & Richey, J. A. (2017). Rural trends in diagnosis and services for autism spectrum disorder. Frontiers in Psychology, 8, 590. https://doi.org/10.3389/fpsyg.2017.00590
Baggett, K. M., Davis, B., Feil, E. G., Sheeber, L. B., Landry, S. H., Carta, J. J., & Leve, C. (2010). Technologies for expanding the reach of evidence-based interventions: Preliminary results for promoting social-emotional development in early childhood. Topics in Early Childhood Special Education, 29(4), 226–238. https://doi.org/10.1177/0271121409354782
Befort, C. A., Nazir, N., & Perri, M. G. (2012). Prevalence of obesity among adult from rural and urban areas of the United States: Finding from NHANES (2005–2008). Journal of Rural Health, 28(4), 392–397. https://doi.org/10.1111/j.1748-0361.2012.00411.x
Boring, M. A., Hootman, J. M., Liu, Y., Theis, K. A., Murphy, L. B., Barbour, K. E., Helmick, C. G., Brady, T. J., & Croft, J. B. (2017). Prevalence of arthritis and arthritis-attributable activity limitation by urban-rural county classification. Mortality & Morbidity Weekly Report, 66(20), 527–532. https://doi.org/10.15585/mmwr.mm6620a2
Cossman, J., James, W., & Wolf, J. K. (2017). The differential effects of rural health care access on race-specific mortality. SSM-Population Health, 3, 618–623. https://doi.org/10.1016/j.ssmph.2017.07.013
Council of Autism Service Providers. (2021). Practice parameters for telehealth-implementation of applied behavior analysis (2nd edn.). Retrieved from https://casproviders.org/asd-guidelines/
Crone, R. M., & Mehta, S. S. (2016). Parent training on generalized use of behavior analytic strategies for decreasing the problem behavior of children with autism spectrum disorder: A data-based case study. Education & Treatment of Children, 39(1), 64–94.
Ellison, K. S., Guidry, J., Picou, P., Adenuga, P., & Davis, T. E., III. (2021). Telehealth and autism prior to and in the age of COVID-19: A systematic and critical review of the last decade. Clinical Child and Family Psychology Review, 24, 599–630. https://doi.org/10.1007/s10567-021-00358-0
Ferguson, J., Craig, E. A., & Dounavi, K. (2019). Telehealth as a model for providing behavior analytic interventions to individuals with autism spectrum disorder: A systematic review. Journal of Autism & Developmental Disorders, 49, 582–616. https://doi.org/10.1007/s10803-018-3724-5
Fisher, W. W., Luczynski, K. C., Blowers, A. P., Vosters, M. E., Pisman, M. D., Craig, A. R., Hood, S. A., Machado, M. A., Lesser, A. D., & Piazza, C. C. (2020). A randomized clinical trial of a virtual-training program for teaching applied-behavior-analysis skills to parents of children with autism spectrum disorder. Journal of Applied Behavior Analysis, 53(4), 1856–1875. https://doi.org/10.1002/jaba.778
Heitzman-Powell, L. S., Buzhardt, J., Rusinko, L. C., & Miller, T. M. (2014). Formative evaluation of an ABA outreach training program for parents of children with autism in remote areas. Focus on Autism & Other Developmental Disabilities, 29(1), 23–38. https://doi.org/10.1177/1088357613504992
Hu, X., Summers, J. A., Turnbull, A., & Zuna, N. (2011). The quantitative measurement of family quality of life: A review of available instruments. Journal of Intellectual Disability Research, 55, 1098–1114. https://doi.org/10.1111/j.1365-2788.2011.01463.x
Internal Revenue Service. (2019). 2020 standard mileage rates. http://www.irs.gov/newsroom/irs-issues-standard-mileage-rates-for-2020
Jang, J., Dixon, D. R., Tarbox, J., Granpeesheh, D., Kornack, J., & de Nocker, Y. (2012). Randomized trial of an eLearning program for training family members of children with autism in the principles and procedures of applied behavior analysis. Research in Autism Spectrum Disorders, 6, 852–856. https://doi.org/10.1016/j.rasd.2011.11.004
Koegel, R. L., Symon, J. B., & Koegel, L. K. (2002). Parent education for families of children with Autism living in geographically distant areas. Journal of Positive Behavior Interventions, 4(2), 88–103. https://doi.org/10.1177/109830070200400204
Koonin, L. M., Hoots, B., Tsang, C. A., Leroy, Z., Farris, K., Jolly, T., Antall, P., McCabe, B., Zelis, C. B. R., Tong, I., & Harris, A. M. (2020). Trends in the use of telehealth during the emergence of the COVID-19 pandemic—United States, January–March 2020. Mortality & Morbidity Weekly Report, 69, 1595–1599. https://doi.org/10.15585/mmwr.mm6943a3externalicon
Lindgren, S., Wacker, D., Schieltz, K., Suess, A., Pelzel, K., Kopelman, T., Lee, J., Romani, P., & O’Brien, M. (2020). A randomized controlled trial of functional communication training via telehealth for young children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 50(12), 4449–4462. https://doi.org/10.1007/s10803-020-04451-1
Mauch, D., Pfefferle, S., Booker, C., Pustell, M., & Levin, J. (2011). Report on state services to individuals with autism spectrum disorders. Centers for Medicare & Medicaid ASD Services Project (S-10 CMS-33; No. 2). https://www.cms.gov/apps/files/9-state-report.pdf.
Mello, M. P., Goldman, S. E., Urbano, R. C., & Hodapp, R. M. (2016). Services for children with autism spectrum disorder: Comparing rural and non-rural communities. Education & Training in Autism & Developmental Disabilities, 51(4), 355–365.
National Center for Immunization and Respiratory Diseases. (2020). Implementation of mitigation strategies for communities with local COVID-19 transmission. Division of Viral Diseases https://www.cdc.gov/coronavirus/2019-ncov/downloads/community-mitigation-strategy.pdf
Rimland, B. & Edelson, S. M. (1999). Autism treatment evaluation checklist (ATEC). https://www.autism.org/autism-treatment-evaluation-checklist; https://doi.org/10.1037/t03995-000
Sarokoff, R. A., & Sturmey, P. (2008). The effects of instructions, rehearsal, modeling, and feedback on acquisition and generalization of staff use of discrete trial teaching and student correct responses. Research in Autism Spectrum Disorders, 2, 125–136. https://doi.org/10.1016/j.rasd.2007.04.002
Schopler, E., Reichler, R. J., DeVellis, R. F., & Daly, K. (1980). Toward objective classification of childhood autism: Childhood Autism Rating Scale (CARS). Journal of Autism & Developmental Disorders, 10(1), 91–103. https://doi.org/10.1007/BF02408436
Schultz, T. R., Schmidt, C. R., & Stichter, J. P. (2011). A review of parent education programs for parents of children with autism spectrum disorders. Focus on Autism & Other Developmental Disabilities, 26(2), 96–104. https://doi.org/10.1177/1088357610397346
Solomon, M., Ono, M., Timmer, S., & Goodlin-Jones, B. (2008). The effectiveness of parent-child interaction therapy for families of children on the autism spectrum. Journal of Autism & Developmental Disorders, 38(9), 1767–1776. https://doi.org/10.1007/s10803-008-0567-5
Sparrow, S. S., Cicchetti, D. V., & Saulnier, C. A. (2016). Vineland Adaptive Behavior Scales, Third edition (Vineland-3). Pearson https://www.pearsonassessments.com/store/usassessments/en/Store/Professional-Assessments/Behavior/Adaptive/Vineland-Adaptive-Behavior-Scales-%7C-Third-Edition/p/100001622.html?tab=resources
Tomlinson, S. R. L., Gore, N., & McGill, P. (2018). Training individuals to implement applied behavior analytic procedure via telehealth: A systematic review of the literature. Journal of Behavioral Education, 27, 172–222. https://doi.org/10.1007/s10864-018-9292-0
U.S. Census Bureau. (2010). https://www.census.gov/library/stories/2017/08/rural-america.html
Vismara, L. A., Young, G. S., & Rogers, S. J. (2012). Telehealth for expanding the reach of early autism training to parents. Autism Research & Treatment, 2012(2012), Article 121878. https://doi.org/10.1155/2012/121878
Vismara, L. A., McCormick, C., Young, G. S., Nadham, A., & Monlux, K. (2013). Preliminary findings of a telehealth approach to parent training in autism. Journal of Autism & Developmental Disorders, 43, 2953–2969. https://doi.org/10.1007/s10803-013-1841-8
Wainer, A. L., & Ingersoll, B. R. (2013). Disseminating ASD interventions: A pilot study of a distance learning program for parents and professionals. Journal of Autism & Developmental Disorders, 43, 11–24. https://doi.org/10.1007/s10803-012-1538-4
Wainer, A. L., & Ingersoll, B. R. (2015). Increasing access to an ASD imitation intervention via a telehealth parent training program. Journal of Autism & Developmental Disorders, 45, 3877–3890. https://doi.org/10.1007/s10803-014-2186-7
Wang, L., & Leslie, D. L. (2010). Health care expenditures for children with autism spectrum disorders in Medicaid. Journal of American Academy of Child Adolescent Psychiatry, 49(11), 1165–1171. https://doi.org/10.1016/j.jaac.2010.08.003
Data Availability
Data is available upon request. Specific materials for the OASIS training are proprietary and must be obtained by the original authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This project was considered exempt by the Southern Illinois University (Carbondale) Human Subject Committee (HSC: Protocol #19145), with the HSC reporting to researchers that the methods of parent training were considered part of typical clinical care and not subject to standard review.
Informed Consent
Informed consent was obtained for all participants per the guidelines of the SIU-C HSC.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
• Telehealth-based parent training is an effective tool in integrating parents into treatment services
• Manualized parent training can increase parent skills and knowledge
• Skill gains may occur quickly under the OASIS model, with skills maintaining over time
• Use of parent training can inform or strengthen delivery of more comprehensive treatment models
• The use of structured parent training may assist in treatment planning and authorization of services
This research was completed in partial fulfillment for the first author’s doctoral degree as a portion of dissertation requirements at Southern Illinois University.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Boydston, P., Redner, R. & Wold, K. Examination of a Telehealth-Based Parent Training Program in Rural or Underserved Areas for Families Impacted by Autism. Behav Analysis Practice 16, 795–811 (2023). https://doi.org/10.1007/s40617-022-00763-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40617-022-00763-z