Abstract
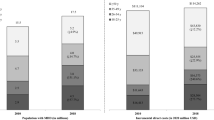
The gap in fatal opioid overdose rates has been closing between non-Hispanic Black and non-Hispanic White individuals. The rising opioid-involved mortality rates among non-Hispanic Black adults has been identified by SAMHSA as a critical public health issue. However, further research is needed that utilizes comprehensive surveillance data on both fatal and non-fatal opioid-involved overdoses to better assess the changing trends and evaluate factors contributing to changing disparities. We conducted an analysis of medical examiner and hospital data for years 2016–2021 from the largest county in Illinois (Cook) to (1) evaluate disparities in non-fatal and fatal opioid-involved overdoses between middle-aged non-Hispanic Black adults and Black adults of other age groups stratified by sex, (2) to assess if disparities exist across middle-aged adults of different race-ethnicities specifically non-Hispanic White and Hispanic-Latino adults, and (3) evaluate factors contributing to the disparities. Fatal opioid overdose rates among middle-aged Black men 45–64 years old were on average 5.3 times higher than Black men of other age groups, and 6.2 times higher than middle-aged non-Black men. Similarly, fatal opioid overdose rates among middle-aged Black women were on average 5.0 times higher than Black women of other age groups, and 4.9 times higher than middle-aged non-Black women. Hospital utilization rates for opioid-involved overdoses showed similar disparities between age groups and race-ethnicities. Findings indicate that stark disparities in rates of opioid-involved overdoses among middle-aged Black men and women are likely attributed to exposure to more lethal opioids, drug variability in local markets, differences in concurrent drug exposures, and lower access to harm reduction, emergent and preventative health services.


Similar content being viewed by others
Data Availability
All medical examiner data are publicly available at https://datacatalog.cookcountyil.gov. The hospital data are restricted access and requires a data use agreement. The authors will provide aggregated hospital data upon request.
References
Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 1999–2020 on CDC WONDER Online Database. Data are from the Multiple Cause of Death Files, 1999–2020, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Available at http://wonder.cdc.gov/mcd-icd10.html. Last accessed on July 25, 2022.
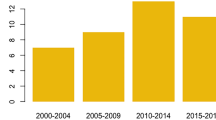
Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and Geographic Patterns in Drug and Synthetic Opioid Overdose Deaths - United States, , 2013-2019. MMWR Morb Mortal Wkly Rep. 2021;70(6):202–7. https://doi.org/10.15585/mmwr.mm7006a4.
James K, Jordan A. The opioid crisis in black communities. J Law Med Ethics. 2018;46(2):404–21. https://doi.org/10.1177/1073110518782949.
Furr-Holden D, Milam AJ, Wang L, Sadler R. African Americans now outpace whites in opioid- involved overdose deaths: a comparison of temporal trends from 1999 to 2018. Addiction. 2021;116(3):677–83. https://doi.org/10.1111/add.15233.
Hoopsick RA, Homish GG, Leonard KE. Differences in Opioid Overdose Mortality Rates Among Middle-Aged Adults by Race/Ethnicity and Sex, 1999–2018. Public Health Rep. 2021;136(2):192–200. https://doi.org/10.1177/0033354920968806.
Shiels MS, Freedman ND, Thomas D. Berrington de Gonzalez A (2018) Trends in US Drug Overdose Deaths in Non-Hispanic Black, Hispanic, and Non-Hispanic White Persons, 2000-2015. Ann Intern Med. 2018;168(6):453–5. https://doi.org/10.7326/M17-1812.
Mason M, Soliman R, Kim HS, Post LA. Disparities by Sex and Race and Ethnicity in Death Rates Due to Opioid Overdose Among Adults 55 Years or Older, 1999 to 2019. JAMA Netw Open. 2022;5(1):e2142982. https://doi.org/10.1001/jamanetworkopen.2021.42982.
Wu ZH, Yong Q, Walker JM, Grady JJ, Laurencin CT. Fentanyl, Heroin, and Cocaine Overdose Fatalities are Shifting to the Black Community: An Analysis of the State of Connecticut. J Racial Ethn Health Disparities. 2022;9(2):722–30. https://doi.org/10.1007/s40615-021-01007-6.
Milam AJ, Furr-Holden D, Wang L, Simon KM. Health Data Disparities in Opioid-Involved Overdose Deaths From 1999 to 2018 in the United States. Am J Public Health. 2021;111(9):1627–35. https://doi.org/10.2105/AJPH.2021.306322.
Substance Abuse and Mental Health Services Administration: The Opioid Crisis and the Black/African American Population: An Urgent Issue. Publication No. PEP20-05-02-001. Office of Behavioral Health Equity. Substance Abuse and Mental Health Services Administration, 2020. Accessed Nov 28 2023. Available at: https://store.samhsa.gov/product/The-Opioid-Crisis-and-the-Black-African-American-Population-An-Urgent-Issue/PEP20-05-02-001.
Illinois Department of Public Health (IDPH). Illinois Health Facilities and Services Review. Hospital Data Profiles and Annual Bed Report. Available at: https://www2.illinois.gov/sites/hfsrb/InventoriesData/FacilityProfiles/Pages/default.aspx. Last accessed August 26, 2022.
Lale A, Krajewski A, Friedman LS. Undertriage of Firearm-Related Injuries in a Major Metropolitan Area. JAMA Surg. 2017;152(5):467–74. https://doi.org/10.1001/jamasurg.2016.5049.
Cook County Government Open Data, 2021. Cook County Medical Examiner Case Archive. Available at: https://datacatalog.cookcountyil.gov/Public-Safety/Medical-Examiner-Case-Archive/cjeq-bs86. Accessed April 26, 2022.
Council of State and Territorial Epidemiologists, 2019. Nonfatal Opioid Overdose Standardized Surveillance Case Definition. Ed. Michael Landen. https://www.cste.org/page/PositionStatements Accessed 28 Dec 2021.
Abasilim C, Holloway-Beth A, Friedman LS. Description of opioid-involved hospital deaths that do not have a subsequent autopsy. Epidemiology. 2023;34(1):111–118. https://doi.org/10.1097/EDE.0000000000001543
United States Census Bureau. American Community Survey, 2016–2020. Sex by Age by Race/Ethnicity (Black or African American Alone, Table B01001B; Hispanic or Latino, Table B01001I; White Alone, Not Hispanic or Latino, Table B01001H). https://data.census.gov/cedsci/advanced. Last accessed July 21, 2022.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. https://doi.org/10.1097/00005650-199801000-00004.
Substance Abuse and Mental Health Services Administration. Results from the 2020 National Survey on Drug Use and Health: Detailed tables. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Available at: https://www.samhsa.gov/data/sites/default/files/reports/rpt35323/NSDUHDetailedTabs2020v25/NSDUHDetailedTabs2020v25/NSDUHDetTabsSect1pe2020.htm. Last Accessed July 22, 2022a.
SAMHSA, Center for Behavioral Health Statistics and Quality, National Survey on Drug Use and Health, 2002-2014. Table 1.15A. Select Substance Use and Substance Use Disorders in Illinois among Persons Aged 12 or Older, by Race and Ethnicity: Numbers in Thousands andPercentages, Annual Averages Based on 2002-2014. Available at: https://www.samhsa.gov/data/all-reports. Last accessed July 22, 2022b.
Cunningham JK, Maxwell JC, Campollo O, Cunningham KI, Liu LM, Lin HL. Proximity to the US-Mexico border: a key to explaining geographic variation in US methamphetamine, cocaine and heroin purity. Addiction. 2010;105(10):1785–98. https://doi.org/10.1111/j.1360-0443.2010.03032.x.
Drug Enforcement Agency. Special Testing and Research Laboratory. Fentanyl Signature Profiling Program Report. DEA PRB 10–25–19–40. October 2019. Available at: https://www.dea.gov/documents/2019/2019-10/2019-10-28/fentanyl-signature-profiling-program-report. Last accessed July 26, 2022.
World Health Organization. WHO guidelines for the pharmacological and radiotherapeutic management of cancer pain in adults and adolescents. Table A6.2. Geneva: 2018. Licence: CC BY-NC-SA 3.0 IGO.
Wu LT, Zhu H, Swartz MS. Treatment utilization among persons with opioid use disorder in the United States. Drug Alcohol Depend. 2016;169:117–27. https://doi.org/10.1016/j.drugalcdep.2016.10.015.
Appiah L, John D, Owoade DR, Mendenhall J, Appiah D. Factors Influencing Racial and Ethnic Differences in Prescription Opioid Misuse Among Young Adolescents in the USA, 2009–2019. J Racial Ethn Health Disparities. 2021 Nov 29. https://doi.org/10.1007/s40615-021-01194-2
Maguire DR, Minervini V. Interactions between opioids and stimulants: Behavioral pharmacology of abuse-related effects. Adv Pharmacol. 2022;93:1–33. https://doi.org/10.1016/bs.apha.2021.10.002.
Leri F, Bruneau J, Stewart J. Understanding polydrug use: review of heroin and cocaine co-use. Addiction. 2003;98(1):7–22. https://doi.org/10.1046/j.1360-0443.2003.00236.x.
Pérez-Mañá C, Papaseit E, Fonseca F, Farré A, Torrens M, Farré M. Drug Interactions With New Synthetic Opioids. M Front. Pharmacol. 2018; 9:1145 (1–17). https://doi.org/10.3389/fphar.2018.01145
Zhao JK, Kral AH, Wenger LD, Bluthenthal RN. Characteristics Associated with Nonmedical Methadone Use among People Who Inject Drugs in California. Subst Use Misuse. 2020;55(3):377–86. https://doi.org/10.1080/10826084.2019.1673420.
Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, Ferri M, Pastor-Barriuso R. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;26(357):j1550. https://doi.org/10.1136/bmj.j1550.PMID:28446428;PMCID:PMC5421454.
Chang JE, Franz B, Cronin CE, Lindenfeld Z, Lai AY, Pagán JA. Racial/ethnic disparities in the availability of hospital based opioid use disorder treatment. J Subst Abuse Treat. 2022;138:108719. https://doi.org/10.1016/j.jsat.2022.108719.
Schuler MS, Dick AW, Stein BD. Growing racial/ethnic disparities in buprenorphine distribution in the United States, 2007–2017. Drug Alcohol Depend. 2021;223:108710. https://doi.org/10.1016/j.drugalcdep.2021.108710.
Grogan CM, Andrews C, Abraham A, Humphreys K, Pollack HA, Smith BT, Friedmann PD. Survey Highlights Differences In Medicaid Coverage For Substance Use Treatment And Opioid Use Disorder Medications. Health Aff (Millwood). 2016;35(12):2289–96. https://doi.org/10.1377/hlthaff.2016.0623.
Gao YA, Drake C, Krans EE, Chen Q, Jarlenski MP. Explaining Racial-ethnic Disparities in the Receipt of Medication for Opioid Use Disorder During Pregnancy. J Addict Med. 2022. https://doi.org/10.1097/ADM.0000000000000979
Kilaru A.S., Xiong A., Lowenstein M., Meisel Z.F., Perrone J., Khatri U.…Delgado M.K. Incidence of treatment for opioid use disorder following nonfatal overdose in commercially insured patients. JAMA Network Open. 2020;3(5). https://doi.org/10.1001/jamanetworkopen.2020.5852.
Reddy NG, Jacka B, Ziobrowski HN, Wilson T, Lawrence A, Beaudoin FL, Samuels EA. Race, ethnicity, and emergency department post-overdose care. J Subst Abuse Treat. 2021;131:108588. https://doi.org/10.1016/j.jsat.2021.108588.
Mallow PJ, Mercado M, Topmiller M. Disparities in Opioid Use Disorder Treatment Admissions. J Health Econ Outcomes Res. 2020;7(1):85–93. https://doi.org/10.36469/jheor.2020.13266.
Hadland SE, Wharam JF, Schuster MA, Zhang F, Samet JH, Larochelle MR. Trends in Receipt of Buprenorphine and Naltrexone for Opioid Use Disorder Among Adolescents and Young Adults, 2001–2014. JAMA Pediatr. 2017;171(8):747–55. https://doi.org/10.1001/jamapediatrics.2017.0745.
Lagisetty PA, Ross R, Bohnert A, Clay M, Maust DT. Buprenorphine Treatment Divide by Race/Ethnicity and Payment. JAMA Psychiat. 2019;76(9):979–81. https://doi.org/10.1001/jamapsychiatry.2019.0876.PMID:31066881;PMCID:PMC6506898.
Lapham G, Boudreau DM, Johnson EA, Bobb JF, Matthews AG, McCormack J, Liu D, Samet JH, Saxon AJ, Campbell CI, Glass JE, Rossom RC, Murphy MT, Binswanger IA, Yarborough BJH, Bradley KA. PROUD Collaborative Investigators. Prevalence and treatment of opioid use disorders among primary care patients in six health systems. Drug Alcohol Depend. 2020;207:107732. https://doi.org/10.1016/j.drugalcdep.2019.107732.
Stahler GJ, Mennis J, Baron DA. Racial/ethnic disparities in the use of medications for opioid use disorder (MOUD) and their effects on residential drug treatment outcomes in the US. Drug Alcohol Depend. 2021;226:108849. https://doi.org/10.1016/j.drugalcdep.2021.108849.
Dunphy CC, Zhang K, Xu L, Guy GP Jr. Racial-Ethnic Disparities of Buprenorphine and Vivitrol Receipt in Medicaid. Am J Prev Med. 2022;S0749-3797(22):00299–9. https://doi.org/10.1016/j.amepre.2022.05.006.
Gaither JR, Gordon K, Crystal S, Edelman EJ, Kerns RD, Justice AC, Fiellin DA, Becker WC. Racial disparities in discontinuation of long-term opioid therapy following illicit drug use among black and white patients. Drug Alcohol Depend. 2018;192:371–6. https://doi.org/10.1016/j.drugalcdep.2018.05.033.
Lappan SN, Brown AW, Hendricks PS. Dropout rates of in-person psychosocial substance use disorder treatments: a systematic review and meta-analysis. Addiction. 2020;115(2):201–17. https://doi.org/10.1111/add.14793.
Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Smedley BD, Stith AY, Nelson AR, editors. Washington (DC): National Academies Press (US); 2003. https://doi.org/10.17226/12875.
Blair IV, Havranek EP, Price DW, Hanratty R, Fairclough DL, Farley T, Hirsh HK, Steiner JF. Assessment of biases against Latinos and African Americans among primary care providers and community members. Am J Public Health. 2013;103(1):92–8. https://doi.org/10.2105/AJPH.2012.300812.
Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care. Soc Sci Med. 2008;67(3):478–86. https://doi.org/10.1016/j.socscimed.2008.03.019.
Larney S, Bohnert AS, Ganoczy D, Ilgen MA, Hickman M, Blow FC, Degenhardt L. Mortality among older adults with opioid use disorders in the Veteran’s Health Administration, 2000–2011. Drug Alcohol Depend. 2015;147:32–7. https://doi.org/10.1016/j.drugalcdep.2014.12.019.
Molist G, Brugal MT, Barrio G, Mesías B, Bosque-Prous M, Parés-Badell O, de la Fuente L. Spanish Working Group for the Study of Mortality among Drug Users. Effect of ageing and time since first heroin and cocaine use on mortality from external and natural causes in a Spanish cohort of drug users. Int J Drug Policy. 2018;53:8–16. https://doi.org/10.1016/j.drugpo.2017.11.011.
Dennis F. Drug fatalities and treatment fatalism: Complicating the ageing cohort theory. Sociol Health Illn. 2021;43(5):1175–90. https://doi.org/10.1111/1467-9566.13278.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Friedman, L.S., Abasilim, C., Karch, L. et al. Disparities in fatal and non-fatal opioid-involved overdoses among middle-aged non-Hispanic Black Men and Women. J. Racial and Ethnic Health Disparities (2023). https://doi.org/10.1007/s40615-023-01877-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-023-01877-y