Abstract
Objectives
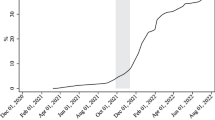
The COVID-19 pandemic has revealed significant differences in COVID-19 vaccination rates, with African Americans reporting lower rates compared to other racial and ethnic groups. The purpose of these analyses was to assess whether COVID-19 vaccination status differed according to age in a sample of 1,240 African American adult congregants of faith-based organizations ages 18 years or older, and to examine whether this association was moderated by gender.
Design
We developed and administered a 75-item cross-sectional survey, the Triad Pastor’s Network COVID-19 and COVID-19 Vaccination survey, to assess experiences and perceptions regarding the COVID-19 virus and vaccines. We assessed the association between age and having received > 1 dose of a COVID-19 vaccine using unadjusted and multivariable binary logistic regression models, and the interaction of age and gender with COVID-19 vaccination status in a multivariable model.
Results
Approximately 86% of participants reported having received ≥ 1 dose of a COVID-19 vaccine. The mean age (standard deviation) of the sample was 51.33 (16.62) years, and 70.9% of the sample was comprised of women. The age by gender interaction term in the multivariable model was significant (p = 0.005), prompting additional analyses stratified by gender. In women, increased age was significantly associated with higher odds of COVID-19 vaccination (odds ratio = 1.09; 95% Confidence Interval 1.06, 1.11; p < 0.001). In men, the association was not significant (p = 0.44).
Conclusions
Older age was positively associated with COVID-19 vaccination in African American women, but not African American men, which may inform strategies to increase vaccination rates.


Similar content being viewed by others
Data Availability
Data and materials from this research are available contingent upon approval of Principal Investigator Goldie S. Byrd, Ph.D.
Code Availability
Code from this research is available contingent upon approval of Principal Investigator Goldie S. Byrd, Ph.D.
References
Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta bio-medica : Atenei Parmensis. 2020;91(1):157–60.
Organization WH. WHO COVID-19 Dashboard 2020 [Available from: https://covid19.who.int/
Prevention CfDCa. COVID Data Tracker Atlanta, GA: Department of Health and Human Services; 2022 [cited 2022 December 21]. Available from: https://covid.cdc.gov/covid-data-tracker
Willis DE, Andersen JA, Bryant-Moore K, Selig JP, Long CR, Felix HC, et al. COVID-19 vaccine hesitancy: race/ethnicity, trust, and fear. Clin Transl Sci. 2021;14(6):2200–7. https://doi.org/10.1111/cts.13077.
Brown IM, Khan A, Slocum J, Campbell LF, Lacey JR, Landry AM. COVID-19 Disparities and the Black Community: a health equity-informed rapid response is needed. Am J Public Health. 2020;110(9):1350–1. https://doi.org/10.2105/AJPH.2020.305804.
Lauring AS, Tenforde MW, Chappell JD, Gaglani M, Ginde AA, McNeal T, et al. Clinical severity of, and effectiveness of mRNA vaccines against, covid-19 from omicron, delta, and alpha SARS-CoV-2 variants in the United States: prospective observational study. BMJ. 2022;376:e069761. https://doi.org/10.1136/bmj-2021-069761.
Lewis NM, Self WH, Gaglani M, Ginde AA, Douin DJ, Keipp Talbot H, et al. Effectiveness of the Ad26.COV2.S (Johnson & Johnson) Coronavirus Disease 2019 (COVID-19) Vaccine for Preventing COVID-19 Hospitalizations and Progression to High Disease Severity in the United States. Clin Infect Dis. 2022;75(Supplement_2):S159-s66.
Fitzpatrick MCM, Seyed M, Pandley, Abhisheck, Galvani, Alison P. Two years of US COVID-19 Vaccines Have Prevented Millions of Hospitalizations and Deaths [Internet]. New York City, NY, USA: Commonwealth Fund. 2022. [cited 2022]. Available from: https://www.commonwealthfund.org/blog/2022/two-years-covid-vaccines-prevented-millions-deaths-hospitalizations
Response NCDoHaHSC-. Vaccinations Dashboard Raleigh, NC: NC Department of Health and Human Services; 2022 [cited 2022 December 21]. Available from: https://covid19.ncdhhs.gov/dashboard/vaccinations
Falsey AR, Frenck RW Jr, Walsh EE, Kitchin N, Absalon J, Gurtman A, et al. SARS-CoV-2 Neutralization with BNT162b2 Vaccine Dose 3. N Engl J Med. 2021;385(17):1627–9.
Feikin DR, Higdon MM, Abu-Raddad LJ, Andrews N, Araos R, Goldberg Y, et al. Duration of effectiveness of vaccines against SARS-CoV-2 infection and COVID-19 disease: results of a systematic review and meta-regression. The Lancet. 2022;399(10328):924–44.
Semelka CT, DeWitt ME, Blevins MW, Holbrook BC, Sanders JW, Alexander-Miller MA. Frailty impacts immune responses to Moderna COVID-19 mRNA vaccine in older adults. Immunity & Ageing. 2023;20(1):4.
Latkin CA, Dayton L, Yi G, Colon B, Kong X. Mask usage, social distancing, racial, and gender correlates of COVID-19 vaccine intentions among adults in the US. PLoS ONE. 2021;16(2):e0246970.
Szilagyi PG, Thomas K, Shah MD, Vizueta N, Cui Y, Vangala S, et al. Likelihood of COVID-19 vaccination by subgroups across the US: post-election trends and disparities. Hum Vaccin Immunother. 2021;17(10):3262–7.
Mondal P, Sinharoy A, Su L. Sociodemographic predictors of COVID-19 vaccine acceptance: a nationwide US-based survey study. Public Health. 2021;198:252–9.
Zhang W, Wu YY, Wu B. Racial/Ethnic Disparities in Getting COVID-19 Vaccine: Do Age, Gender, and Education Matter? Health equity. 2022;6(1):500–7.
Prevention CfDCa. COVID Data Tracker Atlanta, GA: Department of Health and Human Services; 2023 [cited 2022 December 21]. Available from: https://covid.cdc.gov/covid-data-tracker.
Ferdinand KC, Nedunchezhian S, Reddy TK. The COVID-19 and Influenza “Twindemic”: Barriers to Influenza Vaccination and Potential Acceptance of SARS-CoV2 Vaccination in African Americans. J Natl Med Assoc. 2020;112(6):681–7.
Callaghan T, Moghtaderi A, Lueck JA, Hotez PJ, Strych U, Dor A, et al. Correlates and disparities of COVID-19 vaccine hesitancy. 2020.
Galasso V, Pons V, Profeta P, Becher M, Brouard S, Foucault M. Gender differences in COVID-19 attitudes and behavior: panel evidence from eight countries. Proc Natl Acad Sci USA. 2020;117(44):27285–91. https://doi.org/10.1073/pnas.2012520117.
Wu YY, Zhang W. Demographic disparities in COVID-19 vaccine hesitancy among U.S. adults: Analysis of household pulse survey data from Jul 21 to Oct 11 in 2021. Vaccine. 2022;40(52):7510–4.
Yasmin F, Najeeb H, Moeed A, Naeem U, Asghar MS, Chughtai NU, et al. COVID-19 Vaccine Hesitancy in the United States: A Systematic Review. Front Public Health. 2021;9:770985.
Baptist AHWF. Triad Pastoral Network Winston-Salem, NC: Atrium Health Wake Forest Baptist; 2023 [cited 2023 January 27]. Available from: https://school.wakehealth.edu/research/institutes-and-centers/clinical-and-translational-science-institute/maya-angelou-center-for-health-equity/community-engagement/triad-pastoral-network.
Prevention CfDCa. Vaccine Confidence Survey Question Bank Atlanta, GA: Centers for Disease Control and Prevention; 2022 [Available from: https://www.cdc.gov/vaccines/covid-19/vaccinate-with-confidence/rca-guide/downloads/CDC_RCA_Guide_2021_Tools_AppendixD_Surveys-508.pdf.
Kincaid J, Fishburne R, Rogers R, Chissom BJMNAS. Research branch report 8–75. 1975.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
Howden LMM JA Age and Sex Composition: 2010: United States Census Bureau; 2011 [cited 2023 January 27]. Available from: https://www.census.gov/library/publications/2011/dec/c2010br-03.html.
Prevention CfDCa. Three Point Shot Atlanta, GA: Centers for Disease Control and Prevention; 2021 [cited 2023 January 17]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/past-reports/10012021.html.
Nguyen KH, Srivastav A, Razzaghi H, Williams W, Lindley MC, Jorgensen C, et al. COVID-19 Vaccination Intent, Perceptions, and Reasons for Not Vaccinating Among Groups Prioritized for Early Vaccination - United States, September and December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(6):217–22.
Inc. S. Educational attainment in North Carolina in 2021. Statistica 2022 [Available from: https://www.statista.com/statistics/306990/educational-attainment-north-carolina/.
Bureau USC. Census Bureau Releases New Educational Attainment Data Washington, DC: United States Census Bureau; 2022 [cited 2023 February 1]. Available from: https://www.census.gov/newsroom/press-releases/2022/educational-attainment.html#:~:text=Data%20Highlights-,Age,highest%20level%20of%20school%20completed.
Oster AM, Caruso E, DeVies J, Hartnett KP, Boehmer TK. Transmission Dynamics by Age Group in COVID-19 Hotspot Counties - United States, April-September 2020. MMWR Morb Mortal Wkly Rep. 2020;69(41):1494–6.
Wang VH-C, Silver D, Pagán JA. Generational differences in beliefs about COVID-19 vaccines. Preventive Medicine. 2022;157:107005.
Chandler R, Guillaume D, Parker AG, Mack A, Hamilton J, Dorsey J, et al. The impact of COVID-19 among Black women: evaluating perspectives and sources of information. Ethn Health. 2021;26(1):80–93.
Zarocostas J. How to fight an infodemic. Lancet. 2020;395(10225):676.
Aughinbaugh A, Robles O, Sun H. Marriage and divorce: patterns by gender, race, and educational attainment. Monthly Lab Rev. 2013;136:1.
Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021;39(7):1080–6.
Agaku IT, Adeoye C, Long TG. Geographic, Occupational, and Sociodemographic Variations in Uptake of COVID-19 Booster Doses Among Fully Vaccinated US Adults, December 1, 2021, to January 10, 2022. JAMA Netw Open. 2022;5(8):e2227680.
Winter SS, Page-Reeves JM, Page KA, Haozous E, Solares A, Nicole Cordova C, et al. Inclusion of special populations in clinical research: important considerations and guidelines. J Clin Trans Res. 2018;4(1):56–69.
James DCS, Harville C, Efunbumi O, Babazadeh I, Ali S. You Have to Approach Us Right: A Qualitative Framework Analysis for Recruiting African Americans Into mHealth Research. Health Educ Behav. 2017;44(5):781–90.
Atske SPA. Home broadband adoption, computer ownership vary by race, ethnicity in the U.S. Washington, D.C.: Pew Research Center; 2021 [cited 2023 January 17]. Available from: https://www.pewresearch.org/fact-tank/2021/07/16/home-broadband-adoption-computer-ownership-vary-by-race-ethnicity-in-the-u-s/.
Block R, Burnham M, Kahn K, Peng R, Seeman J, Seto C. Perceived risk, political polarization, and the willingness to follow COVID-19 mitigation guidelines. Soc Sci Med. 2022;305:115091.
Kays K, Gathercoal K, Buhrow W. Does survey format influence self-disclosure on sensitive question items? Comput Hum Behav. 2012;28(1):251–6.
Santibanez TA, Zhou T, Black CL, Vogt TM, Murthy BP, Pineau V, Singleton JA. Sociodemographic variation in early uptake of COVID-19 vaccine and parental intent and attitudes toward vaccination of children aged 6 months–4 years—United States, July 1–29, 2022. Morbidity and Mortality Weekly Report. 2022;71(46):1479.
Huang W, Dove-Medows E, Shealey J, Sanchez K, Benson L, Seymore DD, et al. COVID-19 vaccine attitudes among a majority black sample in the Southern US: public health implications from a qualitative study. BMC Public Health. 2023;23(1):88.
Agarwal R, Dugas M, Ramaprasad J, Luo J, Li G, Gao GG. Socioeconomic privilege and political ideology are associated with racial disparity in COVID-19 vaccination. Proc Natl Acad Sci USA. 2021;118(33):e2107873118. https://doi.org/10.1073/pnas.2107873118.
Andersen JA, Gloster E, Hall S, Rowland B, Willis DE, Kraleti SS, McElfish PA. Associations between COVID-19 vaccine uptake, race/ethnicity, and political party affiliation. J Behav Med. 2023;46(3):525–31. https://doi.org/10.1007/s10865-022-00379-2.
Milligan MA, Hoyt DL, Gold AK, Hiserodt M, Otto MW. COVID-19 vaccine acceptance: influential roles of political party and religiosity. Psychol Health Med. 2022;27(9):1907–17.
Tavilani A, Abbasi E, Kian Ara F, Darini A, Asefy Z. COVID-19 vaccines: Current evidence and considerations. Metabolism Open. 2021;12:100124.
Latkin C, Dayton LA, Yi G, Konstantopoulos A, Park J, Maulsby C, et al. COVID-19 vaccine intentions in the United States, a social-ecological framework. Vaccine. 2021;39(16):2288–94.
CDC COVID-19 Response Team. SARS-CoV-2 B.1.1.529 (Omicron) Variant - United States, December 1-8, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(50):1731–4. https://doi.org/10.15585/mmwr.mm7050e1.
Webb Hooper M, Marshall V, Pérez-Stable EJ. COVID-19 Health Disparities and Adverse Social Determinants of Health. Behav Med. 2022;48(2):133–40.
Ballard EL, Gwyther LP, Edmonds HL. Challenges and opportunities: recruitment and retention of African Americans for Alzheimer disease research: lessons learned. Alzheimer Dis Assoc Disord. 2010;24 Suppl(0):S19–23. https://doi.org/10.1097/WAD.0b013e3181f12432.
Majee W, Anakwe A, Onyeaka K, Harvey IS. The Past Is so Present: Understanding COVID-19 Vaccine Hesitancy among african american adults using qualitative data. J Racial Ethn Health Disparities. 2023;10(1):462–74.
Lloyd SL, Foy CG, Caban-Holt A, Gwathmey T, Williams KL, Starks TD, Mathews A, Vines AI, Richmond A, Byrd GS. Assessing the role of trust in public health agencies and COVID-19 vaccination status among a community sample of African Americans in North Carolina. J Racial Ethn Health Disparities. 2023:1–11. https://doi.org/10.1007/s40615-023-01646-x.
Acknowledgements
The authors would like to acknowledge the support of several individuals. First, the authors thank the respondents to the survey, who dedicated their time to share their experiences and perceptions. Also, the authors thank the members of the Triad Pastors Network Ecclesiastical Council, who informed their congregants of the opportunity to participate in this project. We also thank several MACHE team members who provided technical assistance for this project, including Mr. Jarrell Clark, Ms. Dorey Thomas, Ms. Sarah Langdon, Ms. LaToya Yarber, and Ms. Shelby Henderson.
Funding
This research was funded by the University of North Carolina at Chapel Hill [Increasing Trustworthiness through Engaged Action and Mobilization (I-TEAM), 1OT2HL156812-01], Westat, Inc.(#6793–02-S010), Research Triangle Institute (#17–312-0217571-66099L), and National Institutes of Health (NIH)/ National Heart, Lung, and Blood Institute (NHLBI; OTA-20-011B) NC Community-Engagement Research Alliance Against COVID-19 in Disproportionately Affected Communities (CEAL), NIH CEAL Alliance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the Wake Forest University School of Medicine Institutional Review Board (IRB00068318).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not applicable.
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Foy, C.G., Lloyd, S.L., Williams, K.L. et al. Gender, Age and COVID-19 Vaccination Status in African American Adult Faith-Based Congregants in the Southeastern United States. J. Racial and Ethnic Health Disparities (2023). https://doi.org/10.1007/s40615-023-01744-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-023-01744-w