Abstract
Background
Unplanned emergency department (ED) visits of nursing home residents (NHR) are common, with many transfers not leading to hospitalization. However, there is little research on what diagnostic and therapeutic measures are performed during visits.
Aims
We analyzed underlying diagnoses, characteristics and performed medical procedures of unplanned outpatient ED visits by NHR.
Methods
We conducted a multi-center study of 14 nursing homes (NHs) in northwestern Germany in 03/2018–07/2019. Hospital transfers were documented by nursing staff using a standardized questionnaire for 12 months. In addition, discharge letters were used to collect information about the respective transfer, its reasons and the extend of the medical services performed in the ED.
Results
A total of 161 unplanned ED visits were included (mean age: 84.2 years; 68.3% females). The main transfer reasons were trauma (59.0%), urinary catheter and nutritional probe problems (overall 10.6%; male NHR 25.5%) and altered mental state (9.9%). 32.9% where discharged without imaging or blood test prior. 67.4% of injured NHR (n = 95) required no or only basic wound care. Catheter-related problems (n = 17) were mainly treated by changing an existing suprapubic catheter (35.3%) and by flushing the pre-existing catheter (29.4%).
Discussion
Our data suggest that the diagnostic and therapeutic interventions performed in ED, often do not exceed general practitioner (GP) care and many ED visits seem to be unnecessary.
Conclusion
Better coordination and consultation with GPs as well as better training of nursing staff in handling catheter problems could help to reduce the number of ED visits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of emergency department (ED) visits rises with age and is particularly high among nursing home residents (NHR). These patients are a vulnerable, frail and multimorbid group, who suffer from numerous medical comorbidities leading to increased medical complexity [1, 2]. It is often argued that due to limited access to general practitioners (GPs) and specialists, NHR are often transferred to EDs if their condition deteriorates [3]. However, transfers can be burdensome to NHR, because it puts them at risk for in-hospital complications such as pressure ulcers, delirium, iatrogenic infections, and increased mortality [4,5,6]. Especially those ED visits which do not lead to hospitalization are described as avoidable or inappropriate by many authors [7,8,9].
Overall, about half of all ED visits by NHR do not lead to hospital admission [10]. This is especially remarkable considering that NHR are more than twice as likely as community dwelling older adults to be admitted to the hospital, once presenting in the ED [11]. The most common reasons for such transfers are trauma (often fall-related), altered mental state and infections [8] and we recently found that 75.0% of NHR not subsequently hospitalized were diagnosed with traumatic injuries [12]. However, little is known about the underlying pathways that led to the transfer decision and the extent of treatment in ED in those not being hospitalized. Recent data suggests that in two-thirds of the transfers the GP was not involved in the decision making [13]. Burke et al. found that 19.0% of the NHR discharged from the ED did not have any diagnostic testing prior [11].
Hence the purpose of this study was to gather information from discharge letters to explore the underlying diagnoses and characteristics of unplanned outpatient ED visits of NHR and the extent of medical services performed.
Materials and methods
Study design
This study is part of the HOspitalisations and eMERgency department visits of Nursing home residents (HOMERN) project [14]. In brief, we conducted a multi-center study, including a convenience sample of 14 NHs in northwestern Germany with a total of 802 residents. The included facilities offer full inpatient care by trained nurses and care assistants. As usual in Germany, a GP is not permanently employed by the NHs and, therefore, only available on request. Regarding their location (urban and rural), size (number of beds) and sponsorship (non-profit and private for-profit), the facilities were heterogeneous. Specialized care facilities (e.g., for dementia residents only) and care units that offer short-term care only were excluded. Data was collected between March 2018 and July 2019 for 12 months in each NH. For each hospital transfer (ED visits and hospital admissions, scheduled and unplanned), nursing staff assessed information via questionnaires and were asked to include the related and anonymised discharge letter. There was no need for active participation and informed consent of the residents, because the study relied entirely on information from current medical records and the perceptions of the NH staff. The study was approved by the ethics committee of the Medical Association in Bremen (RA/RE-613, 16 February 2018).
Data collection and assessed variables
A paper-based, four-page questionnaire developed by a multidisciplinary team was used to document data for each hospital transfer. From that, residents sociodemographic and health characteristics, e.g., dementia diagnosis (yes/no) and stage (three groups), and performance in daily activities of daily living using the modified Barthel Index (BI) developed by Shah et al. [15], were assessed. We used the surprise question (“Would you be surprised if this resident died within the next 6 months?”) to identify NHR reaching the end of life [16]. Moreover, the NH staff was asked if the resident was carrying an advance directive (AD) and stated the details by adjusting the emergency advance directive called the patient directive for life sustaining measures (PALMA) [17]. Further information about the decision-making process (final decision maker, previous contact with other health care specialists) and the respective transfer (date and time slot) were gathered and have been published in detail elsewhere [13].
In addition, the discharge letters were used to collect information about: (a) the transfer and its reasons, (b) the extent of treatment and use of medical resources in the ED, (c) recommendations for further care, and (d) the quality of medical documentation. Regarding the transfer, we recorded the admission mode (walk-in, ambulance, ambulance with prehospital emergency physician). Reasons for ED visit (presenting chief complaints) consisted of the most common reasons for ED transfer according to literature recently found in a systemic review by Lemoyne et al. [8].
Additional notes were made on whether the trauma was fall related. Diagnoses were recorded according to the German modification of the International Classification of Diseases, 10th Revision (ICD-10-GM), whereby only the first two digits were coded (e.g., “Open wound of the eyebrow” = S01). Concerning treatment and resources used, we evaluated the type of diagnostic testing in the ED, including physical examination, blood and urine testing, electrocardiography (ECG), and imaging tests. We collected information about procedures performed in the ED which were categorized in drug administration (e.g., intravenous hydration, sedatives, opioid and non-opioid analgesics), wound care (two groups: ‘basic’ including cooling, wound cleansing, dressing, tetanus vaccination, fibrin glue and wound closure strips and ‘advanced’ including casting and suturing) and treatment of catheter and probe associated problems. Moreover, the indication for catheter/probe treatment was recorded (change of existing catheter/probe or initial installation). Furthermore, we assessed whether and which recommendations for further outpatient care after ED visit were available. Each variable could be rated as ‘not assessable’ if no corresponding data was found in the discharge letters or the questionnaires, which were handled as missing values.
Furthermore, we evaluated the quality of medical documentation using a completeness score, based on the recommendations of the implementation guide for discharge letters used by the German Association of IT Manufacturers for the Healthcare Sector (VHitG) [18]. The score consisted of the five items current anamnesis, essential findings, diagnosis, therapy and further procedure, which are described by the VHitG as standard requirements for discharge letters. Points were awarded for each item so that a maximum score of five could be achieved. Any result below five points was considered incomplete. In addition, structural characteristics of the letters were recorded, such as the length of the documents (based on a DIN A4 page) and whether they were machine or handwritten.
Statistical analyses
We restricted our analysis to unplanned ED visits by NHR which did not lead to hospitalization and for which a discharge letters were available. Analyses were performed using descriptive statistics. Data were presented as frequency and percentage, and for continuous variables we stated the mean with standard deviation (SD). Because of missing values, denominators differed between variables. We categorized the resident’s age at time of transfer into four groups (≤ 69, 70–79, 80–89 and ≥ 90 years). The Barthel Index (BI) was grouped into five categories according to ICD-10-GM (slight/no dependency; mild dependency; moderate dependency; severe dependency; total dependency). Data was entered into IBM SPSS Statistics for Windows, Version 25.0 (Armonk, NY: IBM Corp.) for statistical analysis.
Results
Characteristics of unplanned transferred nursing home residents
A total of 240 ED transfers occurred, which did not lead to hospitalisation. 68 questionnaires were returned without a discharge letter and, therefore, excluded. On closer inspection of the discharge letters, eleven transports turned out to be planned visits for X-ray and pacemaker checks and dialysis appointments. These events were also excluded. The final analysis included 161 ED transfers, ranging from 1 to 28 per NH.
NHR were on average 84.2 years (SD: 9.2) and considerably more often female (68.3%) (see Table 1). Only 10.7% presented with slight/no dependency regarding BI. More than half (59.4%) of the NHR had a dementia diagnosis (81.1% of them in a moderate or severe stage). The nursing staff assessed 32.1% of the NHR as palliative cases with a significantly reduced life expectancy (surprise question, estimating 6-month mortality); however, the resident’s wish for end-of-life care was unknown in 54.0%. From the available ADs 21.1% wanted to be treated exclusively in the NH and not be transferred to hospital.
The age distribution between men and women was similar. Some characteristics differed between the sexes. On the one hand, women had a higher BI than men. On the other hand, female NHR were more often diagnosed with dementia than men (64.5 vs. 48.0%), while men were more frequently in a severe stage.
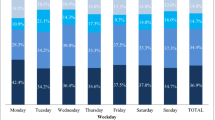
Characteristics of emergency department visits
The ED visits were relatively constant over the weekdays (11.3–18.8%). They most often occurred during office hours from 07:00 to 18:00 h (62.5%). According to the NH staff, about 70% of residents had an acute onset of symptoms with less than 4 h prior to the unplanned ED visit. The GP was not contacted in advance in 75.8% of the transfers, in 26.1%, because he could not be reached by phone. Most often, the final transfer decision was made by the nursing staff (52.2%).
According to the discharge letters, three quarters were admitted by ambulance (71.4%). Most common reasons for ED transfers were trauma (59.0%), which were often fall-related, urinary catheter and nutritional probe problems (overall 10.6%, male NHR 25.5%) and altered mental state (9.9%). Of the 161 letters evaluated, 156 contained diagnoses explaining the presenting chief complaint (see Table 2). Of them, 69.2% were injuries, poisoning and other consequences of external causes (S00-T98, n = 108), with 43.5% being head or neck injuries (S00-S19). Although injuries, poisoning and other consequences of external causes were diagnosed in seven out of 10 transfers in both sexes, categories differed. Female NHR more often had injuries of the extremities (35.1% vs. 5.9%) and those involving several body regions (14.9% vs. 5.9%). In males, 32.4% were complications due to urinary catheters (T83; 4.1% in females).
Extent of treatment and use of medical resources in the emergency department
Most NHR were treated by surgeons (59.0%) (see Table 3). In 93.2% (n = 150) of the discharge letters, information was found on diagnostic procedures performed, whereby the most frequently performed measure was physical examination (94.7%). Blood tests were performed in 26.7% (n = 40), with the most common requests being a small blood count (52.5%). Over half of the NHR received imaging (58.0%, n = 87), whereas an X-ray image was taken most often (52.0%). Other diagnostic measures such as ECG (14.0%) and urine tests (2.7%) were rarely used. 32.9% of the NHR where discharged from ED without imaging or blood test.
A total of 85.1% received treatment in the ED, 41.6% by administration of drugs. 10.6% of the discharge letters stated explicitly that there was no need for therapeutic action at the time of examination. Almost a third received non-opioid analgesics, 19.3% were given sedative drugs. Moreover, 17.0% received intravenous volume substitution.
In the subgroup of NHR presenting due to trauma (n = 95), overall 42.1% (n = 40 of 95) did not receive imaging and 67.4% (n = 64 of 95) required basic or even no wound care (see Fig. 1). 22.1% (n = 21 of 95) received neither imaging nor advanced wound care. Of those receiving imaging (n = 55), 70.9% had an X-ray and 81.8% were discharged from the ED with basic or no wound care at all.
The presentations caused by catheter or probe related problems (n = 17) were either due to occlusion (41.2%) or dislocation (35.3%). These catheter-related problems were treated in 35.3% by changing an pre-existing suprapubic catheter and 29.4% by flushing the pre-existing catheter (see Table 3).
Recommendations for further procedure and care
Regarding the further procedure (follow-up and outpatient treatment recommendation), 25.5% of the letters contained no information. Follow-up at the hospital (planned or if deteriorating) was recommended in 16.1% of NHR, in 29.8% by the GP.
72.7% of the letters contained recommendations for further outpatient treatment (n = 117). The most frequent suggestion was symptomatic treatment (41.8%). 19.7% of the letters stated that no further outpatient follow-up treatment was necessary.
Quality of medical documentation
The discharge letters were on average one page long (SD 0.72), with the shortest 0.25 and the longest 3.75 pages (Median 0.75). 84.5% of the letters were machine and 15.5% were handwritten. The average completeness score was 4.18 (SD 0.99), although only 50.3% of the discharge letters achieved a score of 5, thereby meeting the minimum requirements of the VHitG.
Discussion
In this study, most of the unplanned ED transfers happened during working hours, but the GP was rarely contacted in advance. The most common reasons for transfer were trauma, most often resulting in injuries of the head or neck, and catheter or probe problems. Injuries were often reasons in female and catheter-related problems in male NHR. Our study showed that two thirds of injured NHR discharged from the ED required no or only basic wound care beforehand. Overall, almost a third of the NHR where discharged from the ED without imaging or blood test. The most frequent suggestion for further outpatient treatment was symptomatic and follow-up by the GP.
Consistent with current research [5, 8, 19], the most common reason for unplanned outpatient ED visits was fall-related trauma. Compared to peers living at home, the incidence of falls is two to three times higher among NHR [20]. However, it is estimated that only one in ten falls causes a serious injury requiring hospital treatment [21]. Our study results show that in fact only one third of injured NHR require advanced wound care in the ED, with the majority of these treated by suturing, which would also be possible in an outpatient setting by GPs. A third was discharged from ED without any wound care at all. This finding is also confirmed by a study by Burke et al. [11], calling the need for such visits into question. However, assessing the need for further evaluation after falls is particularly difficult, because less than 30% of NHR can provide an accurate summary of the accident sequence and struggle to describe their symptoms clearly [22]. Our data suggest that injuries of the head and neck were over 40% of the fall consequences. Even if there are no obvious injuries to the head, involvement can often not be ruled out with certainty, especially because elderly show atypical neurological findings in the case of intracranial haemorrhages and increased intracranial pressure [23]. The Glasgow Coma Scale (GCS) often underestimates the extent of the damage [24]. Therefore, some authors call for older patients to always undergo a CT scan after a fall—even if haemodynamics, level of consciousness and GCS value are normal [25, 26]. This leads to radiological overdiagnosis, often without consequences, as it is estimated that in elderly patients less than 5% develop CT findings requiring neurosurgical intervention after a fall on the head [26]. Established diagnostic tests can reduce the number of unnecessary CT scans [27], yet they are often only applicable to NHR to a limited extent. The underlying reasons are pre-existing abnormal neurological findings for example due to existing dementia or increased bleeding risk due to therapy with oral anticoagulants. So far, there are no concrete guidelines in Germany on how to deal with elderly fall patients. In its guideline, the German College of General Practitioners and Family Physicians (DEGAM) recommends ruling out injuries after falls with ‘sufficient certainty’ and treating them ‘adequately’ [28]. However, in our study, only 25% of the NHR received a CT of the head after a fall. As treatment in ED usually does not exceed care by a GP, NHR with traumatic injuries should primarily be seen by a GP. Overall, these results highlight the need for establishing algorithms or guidelines especially for elderly patients to support a targeted differentiation of fall severity and the associated assessment of the need for treatment in the ED. Identifying the group of NHR who do not need further diagnostics already in the NH, could avoid many transfers.
The second most common transfer reason was problems with catheters, which are responsible for over a quarter of all ED visits in the group of male NHR. Over half of these catheter-related visits were due to occlusion and were mostly treated by changing an existing catheter or flushing the pre-existing one. NHR are often catheterized for weeks to months or longer, while the indications for insertion of a urinary catheter are wide-ranging [29]. Within Europe, the proportion of NHR with indwelling urinary catheters (IUCs) varies from 0 to 23%, with significantly more male than female NHR. In Germany, it is estimated that over 15% of male NHR are supplied with IUC, which is the second highest rate in Europe [30]. Men are more likely to have suprapubic catheter and women more likely to have transurethral catheter [29,30,31]. In most cases, women’s IUCs are changed by the nursing staff on site, while men—regardless of whether suprapubic or transurethral—are not [32]. In many NHs there is an internal policy that catheters are not placed or changed in men, although there is no stipulation for this. On the contrary, the National Association of Statutory Health Insurance Physicians even demands that the nursing facility must ensure the change, insertion or removal of a transurethral IUC as well as the care of a suprapubic catheter [33]. When NHR are taken to hospital for changing or flushing an IUC, usually by ambulance, it is not only burdensome for the NHR, but also incurs high costs. Better coordination and consultation with GPs, as well as improved training of nurses in the management transurethral and suprapubic IUCs could reduce the number of ED visits, especially for male NHR.
Limitations and strengths
This is one of the first studies combing information from questionnaires and discharge letters regarding unplanned ED visits by NHR, which did not lead to hospitalization. The data examined were taken from a convenience sample of 14 NHs in northwestern Germany. Therefore, selection bias, which can affect the generalizability of all German NHs, cannot be exempted. However, regarding facility sizes, regions (urban and rural) and sponsorships (non-profit and private-for-profit), we tried to include a heterogeneous sample of NHs. Beyond that, no structural data on the organisation of NHs, such as composition and qualification of NH staff, was available. It is possible that personnel differences influenced the transfer decision.
Furthermore, it is possible that not all transfers carried out during study period were reported by NH staff (under-reporting). A social desirability bias can arise when estimating 6-month mortality, i.e., nursing staff may present themselves or their facility more favourably. However, questionnaires were evaluated completely anonymously to reduce this kind of response. Even though most of the information regarding the NHR characteristics should have been assessed by NH staff relying on existing medical records, a further possible limitation is a recall bias.
About the evaluation of the discharge letters, a limitation is that they were only coded by one person. Furthermore, it is possible that more medical procedures were carried out than subsequently documented in the discharge letters. This is especially true for blood tests, as the corresponding laboratory results were sometimes sent incompletely or possibly not at all.
To assess this possible impact, we evaluated the completeness of the letters using a score.
Conclusions
Falls and IUCs are main causes for unplanned ED visits. Our data suggest that the diagnostic and therapeutic interventions performed in the ED, often do not exceed GP care and many ED visits might, therefore, be unnecessary. Our results indicate that both GPs and EDs are not adequately fulfilling their mandate to provide care to NHR. A large proportion of NHR were send back with no examination or very limited one and with discharge letter not including all basic information. In addition, better training of nurses in the use of IUCs and a revision of internal algorithms in NHs on how to deal with falls and IUCs, could avoid outpatient ED transfers, especially for male NHR. The reinsertion of a transurethral catheter or even the flushing of a suprapubic catheter could be done safely by qualified nursing staff. However, there is a need for more studies looking at IUC use and its management in NHR.
Availability of data and materials
The datasets supporting the conclusions of this article are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
de Souto BP, Lapeyre-Mestre M, Vellas B et al (2014) Multimorbidity type, hospitalizations and emergency department visits among nursing home residents: a preliminary study. J Nutr Health Aging 18:705–709. https://doi.org/10.1007/s12603-014-0030-6
Falconer M, O’Neill D (2007) Profiling disability within nursing homes: a census-based approach. Age Ageing 36:209–213. https://doi.org/10.1093/ageing/afl185
Schröder A-K, Fassmer AM, Allers K et al (2020) Needs and availability of medical specialists’ and allied health professionals’ visits in German nursing homes: a cross-sectional study of nursing home staff. BMC Health Serv Res 20:332. https://doi.org/10.1186/s12913-020-05169-7
Dwyer R, Gabbe B, Stoelwinder JU et al (2014) A systematic review of outcomes following emergency transfer to hospital for residents of aged care facilities. Age Ageing 43:759–766. https://doi.org/10.1093/ageing/afu117
Briggs R, Coughlan T, Collins R et al (2013) Nursing home residents attending the emergency department: clinical characteristics and outcomes. QJM 106:803–808. https://doi.org/10.1093/qjmed/hct136
Bo M, Bonetto M, Bottignole G et al (2016) Length of stay in the emergency department and occurrence of delirium in older medical patients. J Am Geriatr Soc 64:1114–1119. https://doi.org/10.1111/jgs.14103
Caffrey C (2010) Potentially preventable emergency department visits by nursing home residents: United States, 2004. NCHS Data Brief 33:1–8
Lemoyne SE, Herbots HH, De Blick D et al (2019) Appropriateness of transferring nursing home residents to emergency departments: a systematic review. BMC Geriatr 19:17. https://doi.org/10.1186/s12877-019-1028-z
Unroe KT, Carnahan JL, Hickman SE et al (2018) The complexity of determining whether a nursing home transfer is avoidable at time of transfer. J Am Geriatr Soc 66:895–901. https://doi.org/10.1111/jgs.15286
Wang HE, Shah MN, Allman RM et al (2011) Emergency department visits by nursing home residents in the United States. J Am Geriatr Soc 59:1864–1872. https://doi.org/10.1111/j.1532-5415.2011.03587.x
Burke RE, Rooks SP, Levy C et al (2015) Identifying potentially preventable emergency department visits by nursing home residents in the united states. J Am Med Dir Assoc 16:395–399. https://doi.org/10.1016/j.jamda.2015.01.076
Seeger I, Luque Ramos A, Hoffmann F (2018) Outpatient emergency treatment of nursing home residents: analysis of insurance claims data. Z Gerontol Geriatr 51:650–655. https://doi.org/10.1007/s00391-017-1293-4
Pulst A, Fassmer AM, Schmiemann G (2020) Unplanned hospital transfers from nursing homes: who is involved in the transfer decision? Results from the HOMERN study. Aging Clin Exp Res. https://doi.org/10.1007/s40520-020-01751-5
Fassmer AM, Pulst A, Schmiemann G et al (2020) Sex-specific differences in hospital transfers of nursing home residents: results from the HOspitalizations and eMERgency department visits of nursing home residents (HOMERN) project. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17113915
Shah S, Vanclay F, Cooper B (1989) Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol 42:703–709. https://doi.org/10.1016/0895-4356(89)90065-6
White N, Kupeli N, Vickerstaff V et al (2017) How accurate is the ‘surprise question’ at identifying patients at the end of life? A systematic review and meta-analysis. BMC Med 15:139. https://doi.org/10.1186/s12916-017-0907-4
Gerth MA, Schäufele M, Mohr M et al (2012) Notfallsituationen und Patientenverfügungen aus der Sicht des Palliativpatienten—Ergebnisse einer Befragung (emergency situations and advance directives from the patient’s point of view—results of a survey among terminally ill patients). Zeitschrift für Palliativmedizin 13:91–96. https://doi.org/10.1055/s-0031-1298849
Kai U. Heitmann, Andreas Kassner, Erich Gehlen et al (2006) Implementierungsleitfaden arztbrief HL7 clinical document Architecture, 2nd edn. Verband der Hersteller von IT-Lösungen für das Gesundheitswesen
Brownell J, Wang J, Smith A et al (2014) Trends in emergency department visits for ambulatory care sensitive conditions by elderly nursing home residents, 2001 to 2010. JAMA Intern Med 174:156–158. https://doi.org/10.1001/jamainternmed.2013.11821
Wv R-K (2004) Medizin des Alterns und des alten Menschen. Steinkopff-Verlag, Heidelberg. https://doi.org/10.1007/978-3-662-12446-8
Zeyfang A, Hagg-Grün U, Nikolaus T (2013) Basiswissen Medizin des Alterns und des alten Menschen. Springer-Verlag, Berlin. https://doi.org/10.1007/978-3-642-28905-7
Nelson D, Washton D, Jeanmonod R (2013) Communication gaps in nursing home transfers to the ED: impact on turnaround time, disposition, and diagnostic testing. Am J Emerg Med 31:712–716. https://doi.org/10.1016/j.ajem.2012.11.024
Rakier A, Guilburd JN, Soustiel JF et al (1995) Head injuries in the elderly. Brain Inj 9:187–193. https://doi.org/10.3109/02699059509008191
Kehoe A, Rennie S, Smith JE (2015) Glasgow Coma scale is unreliable for the prediction of severe head injury in elderly trauma patients. Emerg Med J 32:613–615. https://doi.org/10.1136/emermed-2013-203488
Oberhofer E (2018) Senior gestürzt: grundsätzlich ein Kopf-CT? Orthop Rheuma 21:12. https://doi.org/10.1007/s15002-018-1286-8
Sartin R, Kim C, Dissanaike S (2017) Discussion of: “is routine head CT indicated in awake stable older patients after a ground level fall?” Am J Surg 214:1055–1058. https://doi.org/10.1016/j.amjsurg.2017.07.038
Foks KA, van den Brand CL, Lingsma HF et al (2018) External validation of computed tomography decision rules for minor head injury: prospective, multicentre cohort study in The Netherlands. BMJ 362:k3527–k3527. https://doi.org/10.1136/bmj.k3527
Familienmedizin DGfAu (2004) Ältere Sturzpatienten. DEGAM-Leitlinie Nr. 4. Düsseldorf (DEGAM)
Geng V, Cobussen-Boekhorst H, Farrell J, et al (2012) Catheterisation. Indwelling catheters in adults. Urethral and suprapubic. Evidence-based guidelines for best practice in urological health care. European Association of Urology Nurses (EAUN)
Sørbye LW, Finne-Soveri H, Ljunggren G et al (2005) Indwelling catheter use in home care: elderly, aged 65+, in 11 different countries in Europe. Age Ageing 34:377–381. https://doi.org/10.1093/ageing/afi094
Gibson KE, Neill S, Tuma E et al (2019) Indwelling urethral versus suprapubic catheters in nursing home residents: determining the safest option for long-term use. J Hosp Infect 102:219–225. https://doi.org/10.1016/j.jhin.2018.07.027
Forde L, Barry F (2018) Point prevalence survey of indwelling urinary catheter use and appropriateness in patients living at home and receiving a community nursing service in Ireland. J Infect Prev 19:123–129. https://doi.org/10.1177/1757177417736595
Brandenburg KV Katheterisierung bei Pflegeheimbewohnern. https://www.kvbb.de/praxis/ansicht-news/article/katheterisierung-bei-pflegeheimbewohnern/507/ Accessed 27 Jan 2021
Acknowledgements
We thank the 14 nursing homes for their participation in our study.
Funding
Open Access funding enabled and organized by Projekt DEAL. The project on which this publication is based was funded by the Innovation Fund coordinated by the Innovation Committee of the Federal Joint Committee in Germany (Innovationsausschuss beim Gemeinsamen Bundesausschuss (G-BA); FKZ: 01VSF16055) which had no influence on the content of the paper and the publication process.
Author information
Authors and Affiliations
Contributions
SH and FH conceptualized the study. AMF coordinated the selection of participating nursing homes and the data collection in the facilities. SH evaluated the discharge letters. GS provided clinical expertise. SH and AMF conducted the analyses. All authors interpreted the data. The manuscript was written by SH and critically revised by AMF, GS and FH. All authors reviewed the manuscript drafts and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The study was approved by the ethics committee of the Medical Association in Bremen (RA/RE-613, 16 February 2018) and the data privacy management of the University of Bremen (06 March 2018).
Human and animal rights
This study does not contain any studies with animals performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heinold, S., Fassmer, A.M., Schmiemann, G. et al. Characteristics of outpatient emergency department visits of nursing home residents: an analysis of discharge letters. Aging Clin Exp Res 33, 3343–3351 (2021). https://doi.org/10.1007/s40520-021-01863-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-01863-6