Abstract
Aims
The objective of this study was to examine baseline frailty status (including cognitive deficits) and important clinical outcomes, to inform shared decision-making in older adults receiving transcatheter aortic valve implantation (TAVI).
Methods and results
We conducted a prospective, observational study of 82 TAVI patients, recruited 2013 to 2015, with 2-year follow-up. Mean age was 83 years (standard deviation (SD) 4.7). Eighteen percent of the patients were frail, as assessed with an 8-item frailty scale. Fifteen patients (18%) had a Mini-Mental Status Examination (MMSE) score below 24 points at baseline, indicating cognitive impairment or dementia and five patients had an MMSE below 20 points. Mean New York Heart Association (NYHA) class at baseline and 6 months was 2.5 (SD 0.6) and 1.4 (SD 0.6), (p < 0.001). There was no change in mean Nottingham Extended Activities of Daily Living (NEADL) scale between baseline and 6 months, 54.2 (SD 11.5) and 54.5 (SD 10.3) points, respectively, mean difference 0.3 (p = 0.7). At 2 years, six patients (7%) had died, four (5%, n = 79) lived in a nursing home, four (5%) suffered from disabling stroke, and six (7%) contracted infective endocarditis.
Conclusions
TAVI patients had improvement in symptoms and maintenance of activity of daily living at 6 months. They had low mortality and most patients lived in their own home 2 years after TAVI. Complications like death, stroke, and endocarditis occurred. Some patients had cognitive impairment before the procedure which might influence decision-making. Our findings may be used to develop pre-TAVI decision aids.
Similar content being viewed by others
Introduction
Transcatheter aortic valve implantation (TAVI) is an established treatment for severe and symptomatic aortic stenosis in patients not eligible for open heart surgery, and it improves symptoms and increase life expectancy [1, 2]. While indication for TAVI has expanded to also include younger and lower risk groups, the majority of TAVI patients are older and have significant comorbidity and frailty that contraindicated surgery. The Valve Academic Research Consortium-2 (VARC 2) consensus document recommends evaluation of independence in activity of daily living before the procedure as risk stratification [3]. However, few studies have focused on independence in activity of daily living as an outcome measure [4, 5].
Among older adults who are seriously ill, death might not be feared as the worse outcome. For many, reduced quality of life and functional or cognitive impairment [6, 7], are relatively greater concerns. Dementia is highly prevalent in older adults [8] and is the leading cause of dependency in older age [9]. Shared decision-making is the favoured model for health care decisions, enhancing treatment choices to reflect patients’ values and preferences [10]. However, the context of cognitive impairment or dementia makes it more difficult for TAVI candidates to participate in the decision-making process [11].
Thus, the aim of this study was to examine baseline frailty status including cognition and outcomes important to decision-making prior to TAVI.
Methods
Study design
This is a single-centre prospective, observational cohort study of 82 elective TAVI patients, with 2-year follow-up. Ninety-four patients were eligible for inclusion, five refused to participate and seven were not included due to logistical reasons. The patients were recruited consecutively from 2013 to 2015.
Participants
Patients ≥ 70 years with symptomatic and severe aortic stenosis accepted for TAVI at Haukeland University Hospital in Western Norway were included. The hospital has a tertiary function for TAVI and serves a population of 1.1 million inhabitants. Severe aortic stenosis was defined by echocardiography according to the European Society of cardiology (ESC) guidelines [1]. Before accepting patients for TAVI, a heart team including interventional cardiologists, cardiac surgeons and imaging specialists, had declined them for surgical aortic valve replacement due to high risk. At the time of the study, there was no screening for frailty preceding the intervention, and the frailty score of the study patients was not known to the treatment team. The number of patients selected for conservative treatment is not known but suspected to be small. Nursing home patients and patients with severe dementia are rarely referred for valve intervention in Norway. Exclusion criteria were inability to understand or speak Norwegian.
Procedural characteristics
TAVI was delivered by different routes, seventy five (92%) trans-femoral, five trans-subclavian and two with direct aortic access. Two different valves were used, the Medtronic Core Valve in 52 (63%) and Boston Scientific LOTUS Valve in 30 (37%) patients.
Measurements
Baseline
Mini-Mental Status Examination (MMSE) assesses cognition as a scale that ranges from 0 to 30, with higher scores indicating better cognition [12]. The cut-off for normal cognitive function is usually set at 24, with a sensitivity of 0.85 and a specificity of 0.90 for identifying anyone with dementia [13].
The research team developed an 8-item frailty scale [14]. The total score is calculated by adding different domain scores: cognition (MMSE ≥ 27 = 0 points, MMSE 20–26 = 1 point, MMSE ≤ 19 = 2 points), instrumental activity of daily living (NEADL ≤ 43 = 1 point), nutrition (BMI < 20.5 = 1 point), modified SOF (low energy = 1 point, weight loss (reported, not measured weight loss; therefore, modified) = 1 point, chair stand, not able = 1 point) [15], Charlson Comorbidity Index (≥ 3 = 1 point) [16], and psychological factors (HADS ≥ 15 = 1 point) [17]. The score range from 0 to 9, were 9 represents the frailest patients. Patients were classified frail if they scored ≥ 4 points. This cut-off had a specificity of 80% and sensitivity of 60% at predicting 2-year mortality for this population. In a receiver operating curve, the area under the curve was 0.81 (95% confidence interval 0.71–0.90) [14].
Baseline and 6 months:
Nottingham Extended Activity of Daily living scale (NEADL) is a scale originally developed to assess activities of daily living (ADL) for stroke patients discharged to home, yet frequently used in non-stroke populations [18, 19]. The scale measures extended activities of daily living using a 22-item questionnaire, evaluating four different sections: mobility, kitchen, domestic and leisure. Patients are asked whether they perform the different activities, and the response categories are 0 = not at all, 1 = with help, 2 = on my own with difficulty, 3 = on my own. The different scores sums into a total score of 0 to 66 points, with higher scores indicating greater independence. A score ≤ 43 indicates dependence [19]. One study of stroke patients reported a valid and reliable change if the NEADL improved or deteriorated by 4.9 points or more, and clinically important if the mean change score was in the range from 2.4 to 6.1 points after treatment [20].
The New York Heart Association (NYHA) classification describes patients’ symptoms of heart failure [21] and has been applied to TAVI patients [3]. NYHA class I represents no symptoms of heart failure and no limitation of physical activity, while NYHA class IV represents symptoms of heart failure at rest. Despite limitations it’s widely used both in research and clinical practice.
Follow-up measurements
Baseline NEADL and NYHA were assessed and then repeated at 6 months. Due to some patients living far from the hospital, we performed telephone interviews at 6 months, and MMSE and frailty testing were, therefore, not conducted. For the first 2 years, we recorded composite endpoints as recommended by the Valve Academic Research Consortium-2 (VARC-2) consensus document. We collected data of admission to long-term nursing homes for the first 2 years.
Statistical analyses
We present the data as means and standard deviations (SD), counts and percentages. Changes from baseline to 6 months are analysed using paired t-tests. There were little missing data so we have used complete case analysis and report the number of observations each analysis is based on. Statistical analysis was carried out in IBM SPSS Statistic 24 and R version 3.6.0 [22]. p values < 0.05 were considered statistically significant.
Results
Baseline data
General characteristics
We examined 82 patients with severe and symptomatic aortic stenosis, 39 (48%) women. Mean age was 83 years (SD 4.7), two patients were over 90 years, the oldest 95 years old, and there were six patients under 75 years. Most patients (62%) lived with their spouse. A majority (55%) had only primary school, while 20% had a university degree.
Geriatric characteristics
Fifteen patients (18%) had an MMSE score < 24, suggesting they were cognitively impaired. One fifth of the patients had a low NEADL score (≤ 43), implying dependence in at least one instrumental activity of daily living. As expected, NEADL and MMSE was correlated (Spearman’s rho = 0.47, p < 0.001). Eleven patients had a low BMI, however, 27 (33%) reported weight loss last year. Charlson comorbidity index was ≥ 3 in 36 (44%) of the patients, demonstrating a high burden of comorbidity. Six (7%) patients had a score ≥ 15 on the Hospital Anxiety and Depression Scale; i.e., few patients had severe anxiety or depression. For 80 patients, baseline 8-item frailty scale was calculated, and 14 patients (18%) were defined as frail.
Cardiovascular characteristics
Logistic EuroSCORE [23] was below 10 (predicting low surgical risk) in 20 (24%) and over 20 (high surgical risk) in 19 (23%) of the patients. Almost half (48%) of the patients had NYHA ≥ 3 at baseline, indicating a significant burden of symptoms. Few patients (11%) had a pacemaker before TAVI, and 26 (32%) had atrial fibrillation at baseline (Table 1).
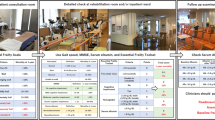
Follow-up
One patients was lost to follow-up at the telephone interview and three had died. For three patients, information was missing on whether they lived at home or in nursing home at 2-year follow-up. VARC 2 composite endpoint is presented in Table 2, and endocarditis is separately presented in Table 3 with complementary data.
Mortality and morbidity
Two patients (2%) died early (< 30 days), and one had a disabling stroke. At 1 year, four patients (5%) had died and 4 (5%) had a disabling stroke. After 2 years, 6 (7%) patients had died, five of cardiovascular and one of non-cardiovascular cause. Four patients lived in nursing homes. There were no new disabling stroke from one to 2 years. Six patients (7%) had endocarditis during the first 2 years. Thirty-two patients (39%) got a new pacemaker perioperative (during the hospital stay).
Patient-reported outcome measures at 6 months
NEADL
The NEADL score was available in 78 patients at 6 months. All patients were reached in person except for one, where the spouse provided information. For one patient, only NEADL at 6 months was available. There was no change in mean NEADL (n = 77) at baseline and 6 months with 54.2 (SD 11.5) and 54.5 (SD 10.3), respectively, mean difference 0.3 (p = 0.7). Even so, 13 patients (17%) improved 5 points or more at the NEADL from baseline to 6 months, and 14 patients (18%) deteriorated 5 points or more. We did not find an association between frailty status and deterioration in NEADL score. For example, the proportion of patients who deteriorated in NEADL score was similar in the frail and the non-frail group (42% and 55%, respectively, p = 0.53, Fisher’s exact test).
NYHA class
After 6 months, the majority was in NYHA I (68%), about a quarter were in NYHA II (27%) and a few in NYHA III (5%). No patients were in NYHA IV. Mean NYHA (n = 78) at baseline and 6 months was 2.5 (SD 0.6) and 1.4 (SD 0.6), respectively, a significant improvement (p < 0.001). Four patients had missing NYHA class at 6 months (three dead, one lost to follow-up) (Fig. 1).
Individual changes in NYHA class from baseline (n = 82) to 6 months (n = 78). The height of each bar is proportional to the number of patients with the corresponding NYHA class, and the width of the ends of each flow line is proportional to the number of patients with the given pattern of change of NYHA class
Discussion
This prospective observational study of 82 patients documents symptom improvement and maintenance of activities of daily living 6 months after TAVI. They had low mortality and most patients lived in their own home 2 years after TAVI. At baseline, 18% had an MMSE score, indicating cognitive impairment or dementia. We found a higher frequency of endocarditis than expected. According to the basic principles of shared decisions-making, balanced information regarding risks and benefits, and exploring patients’ values and goals are important. Physicians should be aware that patients’ cognitive impairment or dementia might affect the ability to participate in the decision-making process and give an informed consent.
Mortality at one (5%) and 2 years (7%) after TAVI was low in this cohort, where mean age is over 80 years and there is a substantial burden of comorbidity and frailty. We found a substantial improvement in NYHA class from baseline to 6 months. Based on the improvement of symptoms we expected to find an improvement in NEADL. However, we found no change in mean NEADL. There was a variation on an individual level. Some patients improved their independence and others deteriorated, although for most patients, the change in NEADL was minor. Other factors, like frailty and dementia, probably have more impact on the level of independence than the aortic stenosis per se [4], and 6 months follow-up is probably too short to establish deterioration due to other causes. There was no difference between the frail and robust patients regarding change in NEADL from baseline to 6 months.
At baseline, 15 patients had an MMSE below 24, indicating possible cognitive impairment or dementia [13]. Five patients had an MMSE less than 20, which increases the probability of incapacity, and likely reduces their power of judgement during the decision-making processes before TAVI [11]. Several studies have suggested that a low MMSE score at baseline predicts poor outcomes after TAVI [4, 24]. However, there are also studies demonstrating cognitive improvement after TAVI when impairment is caused by the aortic stenosis itself [25]. For patients with established dementia, surviving to end stage dementia might not be what the patient would choose autonomously. These are difficult issues to discuss with patients with dementia and their families, both due to patients’ anosognosia (a physiological damage to the brain, where patients have no awareness of their disease) [26], and also health care professionals’ fear of patients losing hope when focusing on the deterioration and increased dependence expected after a diagnosis of dementia [27]. It is important to point out that an MMSE < 24 is not diagnostic of dementia, and sensitivity and specificity for MMSE cut-offs in a TAVI population, might be different than in the general population. Suspicion of dementia should, therefore, lead to further investigations.
We found a higher frequency of infective endocarditis (IE) than expected. In a recent meta-analysis with a mean follow-up at 3.4 years, the overall incidence of IE in TAVI was 2.0% [28]. In the present study, five of six patients with IE had a pacemaker or an ICD, which might be associated with an increased risk of IE [29]. Several single-centre studies finding higher incidences suggests that IE is underreported in large studies and registries [30, 31]. Diagnosing endocarditis is challenging, and the presentation might be uncharacteristic since the patients are old with comorbidities [28]. As endocarditis can occur later on, longer follow-up than 1 year seems important. Antibiotic prophylaxis during the TAVI procedure were administered to all patients. General practitioners were informed routinely on discharge about the risk of endocarditis and indications for prophylaxis.
Prior to TAVI, patients need to be informed of expected NYHA class improvement, survival benefit and maintenance of activities of daily living. Rare and severe complications, like death, stroke and infectious endocarditis, should also be part of the pre- TAVI discussion with the patient. Old patients with substantial comorbidity need to be informed that TAVI will not solve all their health problems. After the study period, written information about the procedure and risks and benefits was developed and administered to patients as part of the decision-making process. Our findings may be used when developing and improving decision aids for this treatment in older adults.
Strengths of the study
All hospitals in Western Norway use the same electronic medical records and VARC-2 endpoints are complete with no patients lost to follow-up. All deaths are automatically registered in the patients’ electronic journal. The same investigator (ES) performed the assessment at baseline and 6 months, increasing reliability.
Limitations of the study
This is a single centre study performed in the early era of TAVI and some of the results might not be transferable due to improvement of equipment, better patient selection and training of the interventional cardiologists performing the procedure. Most patients were independent before TAVI, and minor (nevertheless important to patients) improvements might not be revealed by the NEADL questionnaire. Due to the small sample size, it was not possible to analyse whether specific subgroups improved or deteriorated in NEADL. We performed only telephone interviews at 6 months, preventing us from assessing MMSE and frailty at follow-up. We assume that living in their own home 2 years after TAVI reflects independence of activities of daily living, however, we cannot exclude that some patients living at home were in need of extended care.
Conclusion
TAVI patients had symptom improvement and maintenance of activity of daily living at 6 months. They had low mortality, and most patients lived in their own home 2 years after TAVI. Severe complications, like death, stroke and endocarditis, occurred. Balanced information regarding these risks and benefits is needed to ensure informed consent prior to the procedure, and our findings may be used to develop and improve decision aids assisting this process. Clinicians should be aware that some patients have cognitive impairment before TAVI that might affect their power of judgement and decision-making.
References
Baumgartner H, Falk V, Bax JJ et al (2017) 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 38: 2739–2791
Leon MB, Smith CR, Mack M et al (2010) Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 363: 1597–1607
Kappetein AP, Head SJ, Genereux P et al (2012) Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document (VARC-2). Eur J Cardiothorac Surg 42: S45–60
Schoenenberger AW, Stortecky S, Neumann S et al (2013) Predictors of functional decline in elderly patients undergoing transcatheter aortic valve implantation (TAVI). Eur Heart J 34: 684–692
Eide LS, Ranhoff AH, Fridlund B et al (2016) Delirium as a predictor of physical and cognitive function in individuals aged 80 and older after transcatheter aortic valve implantation or surgical aortic valve replacement. J Am Geriatr Soc 64: 1178–1186
Fried TR, Bradley EH, Towle VR et al (2002) Understanding the treatment preferences of seriously ill patients. N Engl J Med 346: 1061–1066
Yellen SB, Cella DF, Leslie WT (1994) Age and clinical decision making in oncology patients. J Natl Cancer Inst 86: 1766–1770
Satizabal CL, Beiser AS, Chouraki V et al (2016) Incidence of dementia over three decades in the Framingham heart study. N Engl J Med 374: 523–532
World Health Organization and Alzheimer’s Disease International. Dementia: a public health priority. 2012 [cited 2019 Sep 25]; 112]. https://apps.who.int/iris/bitstream/handle/10665/75263/9789241564458_eng.pdf.
Elwyn G, Frosch D, Thomson R et al (2012) Shared decision making: a model for clinical practice. J Gen Intern Med 27: 1361–1367
Sessums LL, Zembrzuska H, Jackson JL (2011) Does this patient have medical decision-making capacity? JAMA 306: 420–427
Folstein MF, Folstein SE, McHugh PR (1975) "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12: 189–198
Creavin ST, Wisniewski S, Noel-Storr AH et al (2016) Mini-Mental State Examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Cochrane Database Syst Rev 13: CD011145
Skaar E, Eide LSP, Norekval TM et al (2019) A novel geriatric assessment frailty score predicts 2-year mortality after transcatheter aortic valve implantation. Eur Heart J Qual Care Clin Outcomes 5: 153–160
Ensrud KE, Ewing SK, Taylor BC et al (2008) Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med 168: 382–389
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic co-morbidity in longitudinal-studies—development and validation. J Chronic Dis 40: 373–383
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67: 361–370
Lincoln NB, Gladman JR (1992) The extended activities of daily living scale: a further validation. Disabil Rehabil. [Research Support, Non-U.S. Gov't] 14: 41–43
Kristjansson SR, Nesbakken A, Jordhoy MS et al (2010) Comprehensive geriatric assessment can predict complications in elderly patients after elective surgery for colorectal cancer: a prospective observational cohort study. Crit Rev Oncol Hematol 76: 208–217
Wu CY, Chuang LL, Lin KC et al (2011) Responsiveness, minimal detectable change, and minimal clinically important difference of the Nottingham Extended Activities of Daily Living Scale in patients with improved performance after stroke rehabilitation. Arch Phys Med Rehabil 92: 1281–1287
The Criteria Committee for the New York Heart Association (1964) Nomenclature and criteria for diagnosis of diseases of the heart and blood vessels. Little Brown, Boston
R Core Team (2019) Vienna, Austria [cited 2019]. R: A language and environment for statistical computing]. https://www.r-project.org/
Roques F, Michel P, Goldstone AR et al (2003) The logistic EuroSCORE. Eur Heart J 24: 881–882
Kim DH, Afilalo J, Shi SM et al (2019) Evaluation of changes in functional status in the year after aortic valve replacement. JAMA Intern Med 179: 383–391
Schoenenberger AW, Zuber C, Moser A et al (2016) Evolution of cognitive function after transcatheter aortic valve implantation. Circ Cardiovasc Interv 9:e00359. https://doi.org/10.1161/CIRCINTERVENTIONS.116.003590
Salmon E, Perani D, Herholz K et al (2006) Neural correlates of anosognosia for cognitive impairment in Alzheimer's disease. Hum Brain Mapp 27: 588–597
Marzanski M (2000) On telling the truth to patients with dementia. West J Med 173: 318–323
Ando T, Ashraf S, Villablanca PA et al (2019) Meta-analysis comparing the incidence of infective endocarditis following transcatheter aortic valve implantation versus surgical aortic valve replacement. Am J Cardiol 123: 827–832
Kolte D, Goldsweig A, Kennedy KF et al (2018) Comparison of incidence, predictors, and outcomes of early infective endocarditis after transcatheter aortic valve implantation versus surgical aortic valve replacement in the United States. Am J Cardiol 122: 2112–2119
Puls M, Eiffert H, Hunlich M et al (2013) Prosthetic valve endocarditis after transcatheter aortic valve implantation: the incidence in a single-centre cohort and reflections on clinical, echocardiographic and prognostic features. EuroIntervention 8: 1407–1418
Rodriguez-Vidigal FF, Nogales-Asensio JM, Calvo-Cano A et al (2019) Infective endocarditis after transcatheter aortic valve implantation: contributions of a single-centre experience on incidence and associated factors. Enferm Infecc Microbiol Clin 37:428–434. https://doi.org/10.1016/j.eimc.2018.09.009
Acknowledgements
Open Access funding provided by University of Bergen. We would like to thank the participants of this study.
Funding
This work was supported by Grieg Foundation; and the Department of Heart Disease, Haukeland University Hospital, Bergen, Norway. The funding sources had no influence on the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Human and animal rights statement
All procedures performed in the study were in accordance with the ethical standards of the institution and the national research committee and with the 1964 Helsinki declaration and it’s later amendments. The regional Committee for medical research ethics approved the study (REK 2013/1310).
Informed consent
Written, informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Skaar, E., Øksnes, A., Eide, L.S.P. et al. Baseline frailty status and outcomes important for shared decision-making in older adults receiving transcatheter aortic valve implantation, a prospective observational study. Aging Clin Exp Res 33, 345–352 (2021). https://doi.org/10.1007/s40520-020-01525-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01525-z