Abstract
Background
China had already entered the aging society and taken up the largest number of elderly among the world.
Aims
We intend to estimate cardiometabolic comorbidities situation among elderly coming from rural China.
Methods
We conducted a survey during 2012 to 2013 which enrolled 1744 elderly from rural Northeast China. Data regarding the demographic and lifestyle characteristics and the blood biochemical indexes of these participants were collected by well-trained personnel.
Results
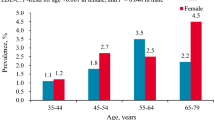
Data in this study shows that the prevalence of hypertension, diabetes, dyslipidemia, obesity, stroke and hyperuricemia was 74.8%, 14.9%, 67.4%, 39.9%, 18.9% and 13.1%, respectively. Female had significantly higher prevalence of dyslipidemia (79.3% vs. 55.9%), diabetes (18.4% vs. 11.4%) and obesity (42.1% vs. 37.7%) than male. Elder subjects (> 75 years) had higher prevalence of hypertension (80.4% vs. 73.4%) than younger ones (65–75 years) while obesity was more prevalent among younger subjects (41.4% vs. 34.1%). Multivariate logistic regression revealed that moderate physical activity and current smoking show beneficial effect on cardiometabolic comorbidities. Higher family income (> 20, 000 CNY/year) was risk factor of diabetes and obesity only while sleep duration between 7 and 8 h/day and married status were risk factors for hypertension only. Current drinking increases the risk of hypertension and dyslipidemia but as protective factor for obesity and stroke.
Conclusion
The prevalence of cardiometabolic comorbidities among was high among rural elderly from China. Physical activity, current smoking and drinking, family income, sleep duration and married status were associated with cardiometabolic comorbidities. Metabolic screen was recommended in the older subjects in rural China.


Similar content being viewed by others
References
Tucker KL, Buranapin S (2001) Nutrition and aging in developing countries. J Nutr 131:2417S–2423S
Peng X (2011) China’s demographic history and future challenges. Science 333:581–587
Wu YS, Dang JW (2013) China report of the development on aging cause. Social Sciences Academic Press, Beijing
Koch S (2010) Healthy ageing supported by technology—a cross-disciplinary research challenge. Inform Health Soc Care 35:81–91
Bao C, Mayila M, Ye Z et al (2015) Forecasting and analyzing the disease burden of aged population in China, based on the 2010 Global Burden of Disease Study. Int J Environ Res Public Health 12:7172–7784
Harlow SD, Linet MS (1989) Agreement between questionnaire data and medical records. The evidence for accuracy of recall. Am J Epidemiol 129:233–248
Kars-Marshall C, Spronk-Boon YW, Pollemans MC (1988) National Health Interview Surveys for health care policy. Soc Sci Med 26:223–233
Guo X, Li Z, Guo L et al (2014) An update on overweight and obesity in rural Northeast China: from lifestyle risk factors to cardiometabolic comorbidities. BMC PUBLIC HEALTH 14:1046
Sun GZ, Li Z, Guo L et al (2014) High prevalence of dyslipidemia and associated risk factors among rural Chinese adults. LIPIDS HEALTH DIS 13:189
Yu S, Yang H, Guo X, Zhang X et al (2015) Prevalence of hyperuricemia and its correlates in rural Northeast Chinese population: from lifestyle risk factors to metabolic comorbidities. Clin Rheumatol 35:1207–1215
Li Z, Guo X, Zheng L et al (2015) Grim status of hypertension in rural China: results from Northeast China Rural Cardiovascular Health Study 2013. J AM SOC HYPERTENS 9:358–364
Yu S, Guo X, Yang H et al (2014) An update on the prevalence of metabolic syndrome and its associated factors in rural northeast China. BMC PUBLIC HEALTH 14:877
O’Brien E, Petrie J, Littler W et al (1990) The British Hypertension Society protocol for the evaluation of automated and semi-automated blood pressure measuring devices with special reference to ambulatory systems. J Hypertens 8:607–619
Kim SM, Lee JS, Lee J et al (2006) Prevalence of diabetes and impaired fasting glucose in Korea: Korean National Health and Nutrition Survey 2001. Diabetes Care 29:226–231
World Health Organization and International Diabetes Fedaration (2006) Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation. WHO, Geneva, pp 1–3
James PA, Oparil S, Carter BL et al (2014) 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 311:507–520
World Health Organization (1996) Hypertension control: report of a WHO expert committee. World Health Organ Tech Rep Ser 862:1–83
Executive Summary of the Third Report of The National Cholesterol Education Program (NCEP) (2001) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 285 (19):2486–2497
Fang J, Alderman MH (2000) Serum uric acid and cardiovascular mortality the NHANES I epidemiologic follow-up study, 1971–1992. National Health and Nutrition Examination Survey. JAMA 283(18):2404–2410
Hu G, Tuomilehto J, Silventoinen K et al (2004) Joint effects of physical activity, body mass index, waist circumference and waist-to-hip ratio with the risk of cardiovascular disease among middle-aged Finnish men and women. Eur Heart J 25:2212–2219
Panagiotakos DB, Pitsavos C, Chrysohoou C et al (2004) Epidemiology of overweight and obesity in a Greek adult population: the ATTICA Study. Obes Res 12:1914–1920
Ma L, Zhao X, Tang Z et al (2015) Epidemiological characteristics of hypertension in the elderly in Beijing, China. PLoS ONE 10:e135480
Wang J, Zhang L, Wang F et al (2014) Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens 27:1355–1361
Cano-Gutierrez C, Reyes-Ortiz CA, Samper-Ternent R et al (2015) Prevalence and factors associated to hypertension among older adults in Bogota. Colombia. J Aging Health 27:1046–1065
Mendes TA, Goldbaum M, Segri NJ et al (2013) Factors associated with the prevalence of hypertension and control practices among elderly residents of Sao Paulo city, Brazil. Cad Saude Publica 29:2275–2286
Liu J, Chen Z, Yang F et al (2014) Prevalence and influencing factors of dyslipidemia among the elderly in Changsha: a community-based study. Zhong Nan Da Xue Xue Bao Yi Xue Ban 39:797–801
Wang JH, Hu DY, Sun YH et al (2013) Prevalence of dyslipidemia and borderline dyslipidemia in aging residents from Beijing communities. Zhonghua Yi Xue Za Zhi 93:3675–3679
Zhao Y, Crimmins EM, Hu P et al (2016) Prevalence, diagnosis, and management of diabetes mellitus among older Chinese: results from the China Health and Retirement Longitudinal Study. Int J Public Health 6:3
Yang W, Lu J, Weng J et al (2010) Prevalence of diabetes among men and women in China. N Engl J Med 362:1090–1101
Lu X, Li X, Zhao Y et al (2014) Contemporary epidemiology of gout and hyperuricemia in community elderly in Beijing. INT J RHEUM DIS 17:400–407
Midthjell K, Holmen J, Bjørndal A et al (1992) Is questionnaire information valid in the study of a chronic disease such as diabetes? The Nord-Trøndelag diabetes study. J Epidemiol Community Health 46:537–542
Hegde SM, Solomon SD (2015) Influence of physical activity on hypertension and cardiac structure and function. Curr Hypertens Rep 17:77
Causland FR, Sacks FM, Forman JP (2014) Marital status, dipping and nocturnal blood pressure: results from the Dietary Approaches to Stop Hypertension trial. J Hypertens 32:756–761
Abete P, Della Morte D, Mazzella F (2006) Lifestyle and prevention of cardiovascular disease in the elderly: an Italian perspective. Am J Geriatr Cardiol 15:28–34
Gojanovic B (2015) Physical activity, exercise and arterial hypertension. Rev Med Suisse 11(481):1426–1433
Lysy Z, Booth GL, Shah BR et al (2013) The impact of income on the incidence of diabetes: a population-based study. Diabetes Res Clin Pract 99:372–379
Kim SR, Han K, Choi JY et al (2015) Age- and sex-specific relationships between household income, education, and diabetes mellitus in Korean adults: the Korea National Health and Nutrition Examination Survey, 2008–2010. PLoS ONE 10:e117034
Lipscombe LL, Austin PC, Manuel DG et al (2010) Income-related differences in mortality among people with diabetes mellitus. CMAJ 182:E1–E17
Wang Y, Mei H, Jiang YR et al (2015) Relationship between duration of sleep and hypertension in adults: a meta-analysis. J Clin Sleep Med 11:1047–1056
van den Berg JF, Tulen JH, Neven AK et al (2007) Sleep duration and hypertension are not associated in the elderly. Hypertension 50:585–589
Zhang M, Zhao J, Tong W et al (2011) Associations between metabolic syndrome and its components and alcohol drinking. Exp Clin Endocrinol Diabetes 119:509–512
Lee K (2012) Gender-specific relationships between alcohol drinking patterns and metabolic syndrome: the Korea National Health and Nutrition Examination Survey 2008. Public Health Nutr 15:1917–1924
Slagter SN, van Vliet-Ostaptchouk JV, Vonk JM et al (2014) Combined effects of smoking and alcohol on metabolic syndrome: the LifeLines cohort study. PLoS ONE 9:e96406
Kang JH, Song YM (2015) Association between cotinine-verified smoking status and metabolic syndrome: analyses of Korean National Health and Nutrition Examination Surveys 2008–2010. Metab Syndr Relat Disord 13:140–148
Zhang M, Jiang Y, Li Y et al (2014) Prevalence of overweight and obesity among Chinese elderly aged 60 and above in 2010. Zhonghua Liu Xing Bing Xue Za Zhi 35:365–369
Litvinova LS, Kirienkova EV, Mazunin IO et al (2015) Insulin resistance pathogenesis in metabolic obesity. Biomed Khim 61:70–82
Acknowledgements
This study was supported by Grants from the “Twelfth Five-Year” project funds (National Science and Technology Support Program of China, Grant # 2012BAJ18B02) and the Social Development Research Program of Liaoning Province (2013225089).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Ethics Committee of China Medical University (Shenyang, China, AF-SDP-07-1, 0-01). All procedures were performed in accordance with ethical standards.
Informed consent
Written consent was obtained from all participants after they had been informed of the objectives, benefits, medical items and confidentiality agreement regarding their personal information.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yu, S., Guo, X., Yang, H. et al. Cardiometabolic comorbidities and epidemiological features among rural Chinese elderly people. Aging Clin Exp Res 32, 1777–1788 (2020). https://doi.org/10.1007/s40520-019-01356-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01356-7