Abstract
Introduction
The measurement of minimal residual disease (MRD) with clonoSEQ® can be used in the assessment of B-cell lymphoid tumor burden throughout treatment with accuracy, sensitivity and standardization when compared to traditional cytomorphology. With the approval of novel treatments, standardized MRD assessment with improved performance is increasingly important. The aim of this analysis is to estimate the cost-effectiveness of MRD testing with clonoSEQ® compared to no MRD testing for patients with multiple myeloma (MM) on maintenance therapy in Germany.
Methods
The cost impact of clonoSEQ® was analyzed from the German statutory insurance perspective. Clinical data were derived from the literature and expert opinions. Cost input was utilized based on publicly available data and literature. Patients in the MRD arm were tested every 6 months. The deterministic Markov model consists of six health states, and every patient begins at the start of maintenance. Included therapies are lenalidomide for maintenance and carfilzomib, lenalidomide and dexamethasone for relapse.
Results
For a time horizon of 10 years, the deterministic cost impact analysis shows total cost of €279,483 for patients using clonoSEQ® in comparison to €356,623 for simulated patients without MRD testing. The main drivers of the cost differences are saved cost of drug holiday. The savings per patient in 1 year are €18,396. Savings after 3 years are €69,991 per patient. Savings after 10 years are €77,140 per patient.
Conclusions
Based on the underlying model, clonoSEQ® can support German health insurance funds to use high-cost drugs more efficiently in the treatment of myeloma.
Similar content being viewed by others
The focus of therapy decisions in B-cell lymphoid malignancies is currently on the long-term outcomes and the quality of life of the patients. |
Knowing the minimal residual disease (MRD) status of a patient with multiple myeloma can help to find the right therapy and to improve overall and progression-free survival. |
Minimal residual disease testing by next-generation sequencing techniques can help to reduce the cost pressure on health insurance companies by saving costs for potentially unnecessary high-priced drugs, especially over a long therapy period of 10 years. |
Introduction
Multiple myeloma (MM) is a malignant proliferation of antibody-producing plasma cells, mostly with its origin in the bone marrow. Often several disease foci are formed with corresponding complications, such as bone fractures and pain or blood count changes. The risk of disease increases significantly with age [1]. For Germany, the Robert Koch Institute (RKI) reported a total incidence of 6910 patients (male 3910, female 3000) and a standardized rate of 6.1 for males and 3.8 for females per 100,000 inhabitants [2]. The 5-year prevalence is reported to be 20,300 patients. The numbers of new cases and deaths have risen slightly in the last 10 years. Cases of illness rose by 2.8% per year in men and 0.8% per year in women. Deaths increased by 1.9% per year in men and 0.7% per year in women. This increase might be explained by an increasingly older population [1].
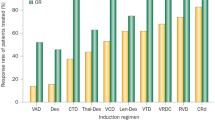
A permanent cure for MM is likely not to be expected [2]. However, the disease can run with manageable symptoms for a relatively long time, and given the availability of numerous novel effective drugs over the last 15 years, patients with newly diagnosed MM have average overall survival (OS) of over 10 years [2, 3]. The modern therapy schemes enable a complete response for up to 80% of patients with MM. Furthermore, longer times without worsening of the disease, so-called progression-free survival (PFS), can be achieved. The therapy for MM is divided into (high-dose) induction, autologous transplantation, consolidation, and maintenance at the initial diagnosis of patients suitable for transplantation. High-dose induction therapy consists of the RVD scheme (R, Revlimid®-lenalidomide; V, Velcade®-bortezomib; D, dexamethasone). Other possible triplet combinations for induction therapy are bortezomib/cyclophosphamide/dexamethasone and bortezomib/thalidomide/dexamethasone. The combination bortezomib/dexamethasone can also be used for induction, but response rates are lower than with triplet therapy. Autologous transplantation involves the transfer of the patient's own bone marrow or blood stem cells which were previously collected from the patient during the remission phase. Frequently, the collection of stem cells takes place after four cycles of induction therapy, which should not exceed six cycles. The autologous stem cell transplantation (SCT) should be performed promptly after successful stem cell collection. After high-dose therapy with autologous stem cell transplantation, consolidation can be carried out with combinations such as bortezomib/lenalidomide/dexamethasone or bortezomib/thalidomide/dexamethasone. For maintenance therapy after SCT, usually lenalidomide is given over a certain period, for example for 1 year after consolidation. Bortezomib and thalidomide can also be used for maintenance therapy. In the case of relapse, a second line of therapy with different triplet combinations like carfilzomib/lenalidomide/dexamethasone may be indicated [1,2,3,4,5,6].
These therapies can result in high drug costs for the statutory health insurance companies, especially when they are no longer effective.
The determination of measurable or minimal residual disease (MRD) in hematopoietic malignancies is an assessment of the tumor burden at the time of patient diagnosis and during therapy. In the context of lymphoid cancers, MRD refers to the presence of malignant B or T cells that may, despite the efforts to improve healing and survival chances, remain in a patient's body during and after treatment of the malignant tumor. Regarding the development of new therapeutic strategies and diagnostic tools, the focus of treatment now is on long-term control, quality of life, and cure rather than short-term control. MRD testing can be a decision support tool in long-term therapy control. Treatment decisions, especially consolidation and maintenance therapy, may be taken considering the MRD positivity or negativity. Several studies indicate that in newly diagnosed MM, the presence of MRD is associated with worse outcomes in PFS and OS, whereas clinical outcomes are better in the absence of MRD. Thus, achieving negative MRD status has become increasingly important in MM treatment in recent years [3, 7, 8].
The clonoSEQ® assay is the only CE-marked in vitro diagnostic tool that uses next-generation sequencing (NGS) to enumerate, specify, and quantify each B cell. When a unique DNA sequence residing within a malignant clone is identified, it is assessed, tracked, and monitored to determine changes in tumor burden. Therefore, the clonoSEQ® assay provides sensitive, standardized, specific, and consistent performance to determine MRD in lymphoid malignancies to assess response to treatment and predict clinical outcomes [9].
The clonoSEQ® assay is powered by NGS technology and differentiated from other NGS assays by advances in biochemistry and proprietary bioinformatics. It is the first MRD assay to leverage a proprietary synthetic immune repertoire to address the inherent bias that occurs when DNA sequences are amplified using a non-standardized multiplex polymerase chain reaction (PCR). These synthetic molecules enable highly accurate and reproducible quantitation of residual disease [10, 11].
After one or more dominant sequence(s) have been identified in a baseline sample, subsequent samples from the same patient have the complete B-cell repertoire profiled, but in addition, MRD is determined, and a “tracking” report is issued. MRD is expressed as a frequency that quantifies the level of residual disease based on the number of remaining copies of the initially dominant sequence(s) relative to the total number of nucleated cells in the sample.
A valid tracking report can result in two possible outcomes:
• When clones associated with a prior clonality test are identified, the result is a quantitative report of residual sequences. When residual sequences are detected, frequency is indicated per million total cells, and a 95% confidence interval is provided.
• When no clones associated with a prior clonality test are identified in a tracking sample, the result is that no residual sequences were detected [9].
Unlike in the USA [12], in Germany there are no health-economic analyses available to date for the use of MRD testing. Thus, the primary aim of this analysis is to estimate the cost saving potential of MRD testing with the clonoSEQ® assay compared to no MRD testing for patients with MM on maintenance drug therapy in Germany.
Methods
IFM Study
As this is a health-economic analysis and no interventional study was conducted, compliance with ethics guidelines is not applicable. As a result of a targeted literature research, the evidence for the developed health-economic model is based mainly on the Intergroupe Francophone du Myélome (IFM) 2009 Study (NCT01191060), which was a randomized, open-label, phase 3 trial, conducted at 69 centers in France, Belgium, and Switzerland with recruitment of patients with symptomatic, measurable, newly diagnosed MM from November 2010 to November 2012 [5].
Patients in the two treatment groups first received induction therapy with three 21-day cycles of RVD, consisting of lenalidomide (25 mg, administered orally on days 1 through 14), bortezomib (1.3 mg per square meter of body surface area, administered intravenously on days 1, 4, 8, and 11), and dexamethasone (20 mg, administered orally on days 1, 2, 4, 5, 8, 9, 11, and 12). Following induction, stem cell mobilization with cyclophosphamide and granulocyte colony-stimulating factor was performed in all patients. For consolidation, one group (RVD-alone group) received five cycles of RVD with a reduced daily dose of dexamethasone of 10 mg. The other group (transplantation group) received melphalan at a dose of 200 mg/m2 plus autologous stem cell transplantation followed by two cycles of RVD with a reduced daily dose of dexamethasone of 10 mg. Maintenance therapy was performed with lenalidomide (10 mg per day for the first 3 months, with a possible dose increase to 15 mg thereafter, depending on side effects) for both groups within the first 3 weeks after the completion of consolidation therapy. Maintenance therapy was continued for 1 year or until disease progression or unacceptable adverse events occurred. It would also be stopped when patients withdrew their consent. For patients in the RVD-alone group, salvage transplantation was recommended at the time of disease progression.
The primary endpoint of the study was PFS. Secondary endpoints were response rate, time to disease progression, OS, and adverse event rates. A total of 350 patients were assigned to each treatment group. In the RVD-alone group, 331 patients (95%) entered the consolidation phase and 321 (92%) the maintenance phase. For 323 patients (92%) in the transplantation group, transplantation was performed, 315 (90%) began to receive RVD therapy after transplantation, and 311 (89%) entered the maintenance phase.
Median PFS was 36 months in the RVD-alone group versus 50 months in the transplantation group. In patients with no detection of MRD, PFS was longer than in those patients in whom MRD was detected. There was no significant difference between the two groups in OS rates at 4 years, with 82% in the RVD-alone group and 81% in the transplantation group. Patients in whom MRD was not detected had longer OS than those patients with detection of MRD [5].
Economic Analysis
The German statutory health insurance (SHI) has an interest in the implementation of good health care for the approximately 88% of residents insured under the SHI system. Nevertheless, as resources are limited, the SHI also wants to keep costs of drug therapies as low as possible. In 2019, €41 billion was spent on drugs, accounting for 17.1% of the total German SHI expenditure. Since 2014, drug expenses have increased €7.6 billion (22.8%) [13]. Using NGS testing could contribute to achieving the goal of cost saving. The interventions assessed in this analysis are MRD testing with the clonoSEQ® assay and no MRD testing during maintenance therapy in patients with MM. MRD testing can provide guidance in therapy decision-making. A second-line therapy can be started earlier in the case of MRD-confirmed relapse, and ineffective therapies can be stopped when the MRD test result is positive. MRD tests can help save unnecessary therapy prolongation while avoiding unnecessary drug costs when these results are negative. Thus, the cost impact of clonoSEQ® was analyzed from the German SHI perspective.
Clinical data were derived from a targeted literature search as described above in the “Methods” section (IFM study), and where missing information was identified, experts were consulted.
Model Structure
To calculate the economic impact of MRD testing with clonoSEQ® from a German payer’s perspective, a Markov cohort model was developed. A Markov model represents stochastic or random processes that occur over a certain time period and is particularly suited to model disease and consider both the costs associated with treatment and interventions and the outcomes [14]. As this is a health-economic analysis and no interventional study was conducted, compliance with ethical guidelines was not required.
The patient pathway for the model is shown in Fig. 1. The deterministic Markov model consists of the six health states: MRD-positive on treatment, MRD-positive off treatment, MRD-negative on treatment, MRD-negative off treatment, relapse, and death. As outcomes are best for the treatment option induction plus stem cell transplantation [5], every patient is assumed to begin after the induction therapy and is at the start of their maintenance therapy. Markov transitions occur monthly, and their probabilities are dependent on the status of the patient in each decision node. The treatment decisions in the decision tree are based on the IFM study by Attal et al. [5]. The average patient is assumed to be 73 years old, and 45% of the patients are assumed to be female [1]. Seventy-five percent of patients are assumed to be diagnosed with a positive MRD test at baseline [15]. In a one-way deterministic sensitivity analysis, the cost impact for varied proportions of MRD-positive patients at baseline was analyzed. Patients are assumed to be tested every 6 months, following European Medicines Agency (EMA) recommendations for repeated MRD testing [16]. In a probabilistic sensitivity analysis, the impact of different time intervals for the MRD assessment on the costs was analyzed. The possible patient pathway always begins with an MRD test, which is either positive or negative. Patients would be either with or without treatment at the time of testing. It is possible for patients to move from any MRD test result on treatment to any MRD result off treatment and vice versa. Patients can move from any MRD state to relapse or death. A return to the previous health state is not possible. OS is assumed to be the same before a possible relapse for both MRD-positive and MRD-negative patients, based on the IFM study. Patients with a negative MRD result had longer PFS [5].
Markov model for MRD testing vs. no MRD testing. It is possible for patients to move from any MRD test result on treatment to any MRD result off treatment and vice versa; patients can move from any MRD state to relapse or death; a return to the previous health status is not possible. MRD minimal residual disease, MTX maintenance therapy
Therapies included in the model are lenalidomide for maintenance therapy, and carfilzomib, lenalidomide, and dexamethasone for the treatment of a relapse (second-line therapy).
Health outcomes calculated in the model are OS and PFS, shown in the form of curves. Input values for both outcome curves with the related negative exponential coefficient and the exponential intercept, expressed in months, were chosen for MRD positivity, negativity, and relapsed state, and are shown in Tables 1 and 2.
Cost Input Data
Cost input data were utilized based on publicly available data and literature resources. Table 3 shows an overview of the cost input data. Costs for the outpatient services visit at an outpatient physician’s practice (€49.17) and specimen collection by puncture (€15.24) were taken from the Uniform Assessment Scale (Einheitlicher Bewertungsmaßstab, EBM) of the National Association of Statutory Health Insurance Physicians (Kassenärztliche Bundesvereinigung, KBV) [19] as amended with effect from 1 July 2021. The cost of the medicinal products concerned (lenalidomide, dexamethasone, and carfilzomib) were taken from the Lauer-Taxe, version 4.0 [20], with data status as of 15 August 2021, and are shown as direct costs and as monthly treatment costs with the corresponding therapy regimes.
The economic analysis included total costs for MRD testing and no MRD testing (deterministic model—Fig. 2). The total and total incremental costs are shown for the comparison of MRD testing with no MRD testing (probabilistic model—Fig. 3). The consideration of the total costs refers mainly to a period of 10 years, as effects on health outcomes in this disease area can only be observed over a long period of time. Thus, PFS in MRD-negative patients can extend up to 56 months, and OS up to 112 months [8]. For comparison purposes, individual analyses were also carried out for 1 and 3 years. A discount rate of 3% for costs and health outcomes was chosen based on the methodology for the evaluation of benefit–cost ratios in the German statutory health insurance system [23, 24].
Results
Results from Deterministic Analysis
For a time horizon of 10 years, the deterministic cost impact analysis shows total costs of €279,483 for patients with MRD testing using clonoSEQ® in comparison to €356,623 for simulated patients without an MRD test (Fig. 2). The main drivers of the cost differences are the saved cost of drug therapy holiday. The cost savings per patient in 1 year are €18,396. Cost savings after 3 years are calculated to be €69,991 per patient. Cost savings after 10 years are €77,140 per patient.
Results from Probabilistic Analysis
Over a period of 10 years, mean total costs for MRD testing amount to €392,592, with a range from €237,115 as lowest to €482,138 as highest possible costs. For no MRD testing, mean total costs are €452,626, with a range from €293,009 as lowest to €482,138 as highest costs. Mean incremental costs for MRD testing using clonoSEQ® versus no MRD testing over 10 years are −€60,033, with a range from −€92,080 to −€35,731 (Fig. 3 and Table 1a, see Supplementary Material). The mean incremental costs per patient in 1 year are -€17,553, with a range from −€24,052 to −€11,862. For a period of 3 years, mean incremental costs are −€54,654, with a range from −€84,756 to −€32,883. For the time horizons of 1 and 3 years, the mean totals costs for no MRD testing lie outside the confidence range (Table 1a, see Supplementary Material).
Results from One-Way Deterministic Sensitivity Analysis
Analyzing the cost impact of MRD testing in MM patients with the assumption of a lower proportion of positive MRD test results at baseline shows higher cost savings compared to no MRD testing. Given an MRD positivity rate of 70% at baseline, cost savings over 10 years are €86,684 per patient, rising to €96,228 per patient at an MRD positivity rate of 65%. When assuming a higher rate of MRD-positive patients at baseline, the cost savings over 10 years decrease to €67,596 (80% MRD positivity) and €58,052 (85% MRD positivity) per patient. An increase of 5% in the baseline MRD positivity rate leads to an increase of about €10,880 in total costs for MRD testing per patient and to an increase of about €1,330 in total costs for no MRD testing. The decrease in total incremental costs is about €9,500 per 5% increase in MRD positivity rate (Table 4 and Fig. 1a, see Supplementary Material). For a period of 3 years, the cost impact depending on the MRD positivity baseline rate is not as great as after 10 years but is still relevant. An increase of 5% in the baseline MRD positivity rate leads to an increase of about €8,900 in total costs for MRD testing per patient and to an increase of about €100 in total costs for no MRD testing. The decrease in total incremental costs is about €8,800 per 5% increase in the MRD positivity rate (Table 1b, see Supplementary Material).
Results from Probabilistic Sensitivity Analysis
When changing the time interval for the MRD assessment, which is set at every 6 months in the base-case analysis, to a shorter frequency of 3 months, cost savings compared to no MRD testing decrease by about €10,000 to €51,000 per patient over 10 years. When assuming a longer MRD assessment interval of 9 months, the cost savings over 10 years remain at a similar level of €61,394 per patient and at €60,363 per patient with an assumed assessment interval of 12 months. A prolongation of the interval of MRD assessment from 3 to 6 months leads to a decrease of about €8,500 in total costs for MRD testing per patient. Total costs for no MRD testing remain on a stable level of about €452,000 to €453,000 at all assessment intervals (Table 1c, see Supplementary Material). For a period of 3 years, the cost impact depending on the MRD assessment interval shows the same pattern. The prolongation of the assessment interval from 3 to 6 months leads to a decrease of about €9,100 in total costs for MRD testing per patient. The total costs for no MRD testing remain on a level of €256,000 to €257,000 for all assessment intervals but lie outside the confidence range (Table 1d, see Supplementary Material).
Discussion
In Germany, there are no significant out-of-pocket costs that would prevent a patient’s access to adequate therapy. Nonetheless, the average cost per patient of new drugs introduced in 2019 has risen by 65% in comparison to the average cost of all new drugs in the last 10 years, as the AMNOG report 2020 shows [25]. Drugs account for approximately 60% of direct follow-up costs in patients with hematologic neoplasms [26]. Costs in MM therapy in particular result from high drug expenditure for ineffective or unnecessary treatment prolongation. Based on decisions by the Federal Joint Committee (Gemeinsamer Bundesausschuss, G-BA), the authors calculated an amount of up to €208,000 per year for drug costs, depending on the choice of medication and therapy scheme [27]. This is consistent with a recently published budget impact analysis. Basic et al. predicted a total volume of €5950 million within 3 years only for drug acquisition in therapy schemes for treatment of MM relapse [28]. The clonoSEQ® assay determines MRD using multiplex PCR and next-generation sequencing (NGS), which are the most specific and standardized sequencing techniques. MRD testing can help detect a relapse sooner and start second-line therapy earlier as well as discontinue ineffective treatment. Thus, costs for drugs that are not needed can be saved and used for other necessary therapies. This economic analysis shows that the mean incremental costs per patient for MRD testing using the clonoSEQ® assay versus no MRD testing in patients with MM are −€18,000 per year. Per-patient costs of €70,000 could be saved in a 3-year time frame, increasing to €80,000 after 10 years. The deterministic one-way sensitivity analysis shows that a strong influencing factor on the cost impact of MRD testing is the baseline proportion of MRD-positive patients: the lower this number, the higher the cost savings after 3 years, which is even more significant after 10 years, as more patients can benefit from the treatment guidance by the MRD test and drug costs can be saved. This also shows the long-term effects in this disease area, which could explain why shorter intervals for the regular MRD assessments are not as cost-effective as longer intervals. The probabilistic sensitivity analysis shows a benefit for a longer time interval (≥ 6 months) in controlling residual disease, which is significant over a period of 10 years.
The wide range in the mean incremental costs can be explained by the use of different drug therapy schemes (e. g. different lengths of treatment cycles) and thus different levels of drug costs. Also, direct drug costs can vary depending on the manufacturer and package size. Besides the cost savings, MRD testing also has an influence on patient outcomes, where the available evidence leaves room for further research. Kunacheewa et al. found that genetic abnormalities are a more powerful prognostic indicator for MM patients, regardless of MRD test results. For newly diagnosed patients who received a triple-drug initial therapy and autologous stem cell transplantation, MRD-negative status did not improve the poor prognostic outcomes in high-risk MM patients [29]. Other publications show that MRD negativity predicts better OS and PFS for patients with MM. Munshi et al. showed in their meta-analysis that MRD negativity is associated with better PFS (HR, 0.41; 95% CI, 0.36–0.48; P < 0.001) and OS (HR, 0.57; 95% CI, 0.46–0.71; P < 0.001). Median PFS was 54 months for MRD-negative patients and 26 months for MRD-positive patients. Median OS was 98 and 82 months, respectively [8]. This could be an explanation for the greater increase in costs for MRD testing than in costs for no MRD testing when increasing the proportion of MRD-positive patients at baseline in our sensitivity analysis by steps of 5%, assuming that MRD-positive patients have a less favorable disease prognosis, need more frequent testing, and have higher medication consumption because therapy is more difficult to manage than in MRD-negative patients. Furthermore, MRD negativity was an indicator for the most appropriate maintenance therapy with thalidomide compared with no therapy. Patients changed from a positive test result to negative and remained at this status in later tests [8]. MRD testing can therefore be not only a cost saver but also an essential clinical decision component of effective MM treatment management.
Our results could be limited by several factors. The analysis was conducted from the view of the statutory health insurance; reimbursement by private insurance was not considered in the model. A starting point in the therapy line had to be defined for the Markov model, and thus only patients with non-refractory disease after induction therapy were analyzed. Demographic factors could have an influence on the treatment outcome and on the related costs, as elderly patients would need additional care with increasing age. However, this should only have an impact on the total costs and not on the incremental costs, as those patients would need additional care regardless of the MRD assessment. The same applies to other and concomitant diseases that could cause additional costs and influence the outcome in MM treatment. Also, other influencing factors in MM therapy were not considered in the model, such as the stem cell collection, which can be performed in either the outpatient or inpatient setting. Stem cell transplantation can be related to different lengths of stay in the hospital, which has an influence on the reimbursement. Also, the choice of the type of transplantation can play a role. Performing an allogeneic instead of an autologous stem cell transplantation for relapse treatment could result in a lower recurrence rate but has the risk of increased transplant-associated morbidity and mortality [1]. The setting we are considering in the model is the outpatient treatment of patients with MM at the general practitioners and oncologists. The clinical setting with different lengths of stay and the influence of MRD testing by clonoSEQ® assay on different therapeutic decisions are not integrated into the model. Despite the limiting factors, our analysis gives a good indication for more effective therapy for patients with MM and cost savings for the statutory health insurance in Germany.
Conclusions
Based on the underlying health-economic model, the clonoSEQ® MRD diagnostic can support health insurance funds in Germany toward the more efficient use of high-cost drugs in the treatment of MM. Therapy decisions can be better and more precisely controlled if the MRD status of patients is known before the next therapy phase. Avoiding unnecessary use of high-priced drugs in this sensitive disease area can result in significant cost savings per patient, especially over a long period of 10 years.
References
DGHO. Multiples Myelom. Leitlinie. Empfehlungen der Fachgesellschaft zur Diagnostik und Therapie hämatologischer und onkologischer Erkrankungen. Stand: Mai 2018. 2020. https://www.onkopedia.com/de/onkopedia/guidelines/multiples-myelom/@@guideline/html/index.html. Accessed 23 Aug 2021.
Robert Koch-Institut (RKI). Krebs in Deutschland für 2015/2016. 12. Ausgabe. Korrigierte Fassung vom 17.08.2020. 2020 23.08.2021]. 2021. https://www.krebsdaten.de/Krebs/DE/Content/Publikationen/Krebs_in_Deutschland/kid_2019/krebs_in_deutschland_2019.pdf;jsessionid=1705F8DC8A337899291C5126135C696E.2_cid372?__blob=publicationFile.
Landgren O, Devlin S, Boulad M, Mailankody S. Role of MRD status in relation to clinical outcomes in newly diagnosed multiple myeloma patients: a meta-analysis. Bone Marrow Transplant. 2016;51(12):1565–8.
DAG-KBT. LEITLINIEN zur autologen Stammzelltransplantation von der Deutschen Arbeitsgemeinschaft für Knochenmark- und Blutstammzelltransplantation (DAG-KBT). Version 1, Stand April 2018. 2018. https://www.dag-kbt.de/files/downloads/Leitlinien_auto_Kap-3_SZT%20und%20Mobilisation.pdf. Accessed 23 Aug 2021.
Attal M, Lauwers-Cances V, Hulin C, Leleu X, Caillot D, Escoffre M, et al. Lenalidomide, bortezomib, and dexamethasone with transplantation for myeloma. N Engl J Med. 2017;376(14):1311–20.
Roussel M, Lauwers-Cances V, Robillard N, Hulin C, Leleu X, Benboubker L, et al. Front-line transplantation program with lenalidomide, bortezomib, and dexamethasone combination as induction and consolidation followed by lenalidomide maintenance in patients with multiple myeloma: a phase II study by the Intergroupe Francophone du Myelome. J Clin Oncol. 2014;32(25):2712–7.
Davies FE. Is molecular remission the goal of multiple myeloma therapy? Hematology. 2017;2017:205–11.
Munshi NC, Avet-Loiseau H, Rawstron AC, Owen RG, Child JA, Thakurta A, et al. Association of minimal residual disease with superior survival outcomes in patients with multiple myeloma: a meta-analysis. JAMA Oncol. 2016;3(1):28–35.
Adaptive Biotechnologies. clonoSEQ® assay B-cell reagent set instructions for use PNL-10047-04. 2021. p. 63.
Robins HS, Carlson CS, Livingston RJ, Emerson RO, Sherwood AM, inventors; United States Patent No.: US 9,371,558 B2: Compositions and method for measuring and calibrating amplification basin multiplexed PCR reactions. US patent application. 2016.
Robins HS, Carlson CS, Livingston RJ, Emerson RO, Sherwood AM, inventors; United States Patent No.: US 9,150,905 B2: Compositions and method for measuring and calibrating amplification basin multiplexed Pcr reactions. US patent application. 2015.
Zimmermann M, Kirsch I, Eckert B, Carlson J. Measurable residual disease testing in multiple myeloma using an improved testing technology: population impact. A clinical and budget impact analysis. Blood. 2017;130:4685.
Verband der Ersatzkassen e. V. (vdek). 2021 vdek-Basisdaten des Gesundheitswesens in Deutschland. 2021. https://www.vdek.com/presse/daten/_jcr_content/par/publicationelement_1479644990/file.res/VDEK_Basisdaten2021_210x280_RZ_web.pdf. Accessed 23 Aug 2021.
Briggs A, Sculpher M. An introduction to Markov modelling for economic evaluation. Pharmacoeconomics. 1998;13:397–409.
Avet-Loiseau H, Ludwig H, Landgren O, Paiva B, Morris C, Yang H, et al. Minimal residual disease status as a surrogate endpoint for progression-free survival in newly diagnosed multiple myeloma studies: a meta-analysis. Clin Lymphoma Myeloma Leuk. 2020;20(1):e30–7.
European Medicines Agency (EMA). Guideline on the use of minimal residual disease as a clinical endpoint in multiple myeloma studies. Draft. 2018. https://www.ema.europa.eu/en/documents/scientific-guideline/draft-guideline-use-minimal-residual-disease-clinical-endpoint-multiple-myeloma-studies_en.pdf. Accessed 23 Aug 2021.
Perrot A, Lauwers-Cances V, Corre J, Robillard N, Hulin C, Chretien ML, et al. Minimal residual disease negativity using deep sequencing is a major prognostic factor in multiple myeloma. Blood. 2018;132(32):2456–64.
Kumar S, Paiva B, Anderson KC, Durie B, Landgren O, Moreau P, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17(8):e328–46.
Kassenärztliche Bundesvereinigung (KBV). ONLINE-VERSION DES EBM. 2021. https://www.kbv.de/html/online-ebm.php. Accessed 23 Aug 2021.
LAUER-FISCHER GmbH. Lauer Taxe 4.0. 2021. https://www.cgm.com/lauer-fischer/loesungen_lf/lauer_taxe_lf/lauertaxe_online_4_0/online.de.jsp. Accessed 23 Aug 2021.
European Medicines Agency (EMA). EPAR—Product information. 2020. https://www.ema.europa.eu/en/documents/product-information/revlimid-epar-product-information_de.pdf. Accessed 23 Aug 2021.
Amgen GmbH. Fachinformation (Zusammenfassung der Merkmale des Arzneimittels). Kyprolis® 10 mg/30 mg/60 mg Pulver zur Herstellung einer Infusionslösung. Stand. 2021. https://fachkreise.amgen.de/x_download.php?t=f&n=1&id=526. Accessed 23 Aug 2021.
Attema AE, Brouwer WBF, Claxton K. Discounting in economic evaluations. Pharmacoeconomics. 2018;36(7):745–58.
Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG). Entwurf einer Methodik für die Bewertung von Verhältnissen zwischen Nutzen und Kosten im System der deutschen gesetzlichen Krankenversicherung. 2009. https://www.iqwig.de/methoden/09-03-18_entwurf_methoden_kosten-nutzen-bewertung_version_2_0.pdf?rev=180506. Accessed 23 Aug 2021.
Greiner W, Witte J, Gensorowsky D, Pauge S. AMNOG-Report 2020. In: Storm A, editor. Beiträge zur Gesundheitsökonomie und Versorgungsforschung (Band 32). Heidelberg: medhochzwei Verlag GmbH; 2020.
Hörster L, Neusser S, Trautner A, Pahmeier K, Lax H, Merkel-Jens A, et al. Kosten der Nachsorge von Patienten mit hämatologischen Neoplasien. Gesundheitsökonomie Qualitätsmanagement. 2021;26(04):207–14.
Gemeinsamer Bundesauschuss (G-BA). Tragende Gründe zum Beschluss des Gemeinsamen Bundesausschusses über eine Änderung der Arzneimittel-Richtlinie (AM-RL): Anlage XII - Beschlüsse über die Nutzenbewertung von Arzneimitteln mit neuen Wirkstoffen nach § 35a SGB V – Daratumumab (neues Anwendungsgebiet; Neubewertung eines Orphan Drugs nach Überschreitung der 50 Mio. Euro Grenze). Vom 15. 2018. https://www.g-ba.de/downloads/40-268-4804/2018-02-15_AM-RL_XII_Daratumumab_D-310_TrG.pdf. Accessed 23 Aug 2021.
Basic E, Kappel M, Misra A, Sellner L, Ratsch BA, Ostwald DA. Budget impact analysis of the use of oral and intravenous therapy regimens for the treatment of relapsed or refractory multiple myeloma in Germany. Eur J Health Econ. 2020;21(9):1351–61.
Kunacheewa C, Lee H, Patel K, Thomas S, Amini B, Srour S, et al. Minimal residual disease negativity does not overcome poor prognosis in high-risk multiple myeloma: a single-center retrospective study. Clin Lymphoma Myeloma Leuk. 2020;20(5):e221–38.
Acknowledgements
Funding
The manuscript and the journal’s Rapid Service Fee were funded by Adaptive Biotechnologies.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Stefan Walzer, Sebastian Krenberger, and Lutz Vollmer were responsible for the conceptualization, adaptation and execution of the German model, the analyses, and the draft of the manuscript; Tony Hewitt and Benjamin Eckert monitored the conceptualization and execution of the analyses and critically reviewed the manuscript draft. All authors made critical comments on the developing manuscript draft and approved the final version of the manuscript for submission and agreed to be responsible for all aspects of the work.
Disclosures
Stefan Walzer, Sebastian Krenberger, and Lutz Vollmer work for MArS Market Access & Pricing Strategy GmbH which received funding for the conceptualization, adaptation, development, and execution of the German analyses. Tony Hewitt and Benjamin Eckert are employed by Adaptive Biotechnologies.
Compliance with Ethics Guidelines
As this is a health-economic analysis and no interventional study was conducted, compliance with ethics guidelines is not applicable.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Walzer, S., Krenberger, S., Vollmer, L. et al. A Cost Impact Analysis of clonoSEQ® as a Valid and CE-Certified Minimal Residual Disease (MRD) Diagnostic Compared to No MRD Testing in Multiple Myeloma in Germany. Oncol Ther 9, 607–619 (2021). https://doi.org/10.1007/s40487-021-00169-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40487-021-00169-x