Abstract
Purpose
To evaluate self-perceived pain levels in the Hyrax compared to other types of maxillary expansion (ME) appliances in growing patients.
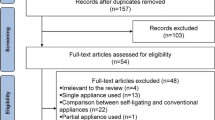
Methods
An unrestricted search of indexed databases and manual searching were performed up to October 2022. Randomized controlled trials (RCTs) comparing the Hyrax appliance with other ME appliances were included. Data screening, extraction, and Risk of Bias (RoB) assessment with the Cochrane tool were performed by two authors.
Results
Six RCTs were included. The number of participants in the included RCTs ranged between 34 to 114 and included both male and female growing patients. Various tools were used to measure self-perceived pain including the Graphic Rating Scale for Pain, the Wong–Baker Faces Pain Scale, the Numerical Rating Scale, the visual analogue scale, and a questionnaire. One RCT reported that pain intensity in patients treated with the Hyrax was higher than in the Haas appliance, with a statistically significant difference limited to the first day. Two RCTs reported that pain intensity in patients treated with the Leaf expander was lower than in the Hyrax during the first 7 days of treatment. Two RCTs reported no significant differences in pain intensity between the Hyrax and other ME appliances. One RCT reported that pain intensity in patients using the computer-guided skeletal ME appliance was higher than in the Hyrax appliance at the first day after expansion. Four RCTs had a high RoB, and two RCTs had a moderate RoB.
Conclusions
Within the limitations of the present systematic review and based on the currently available evidence, it is challenging and inconclusive to identify the best maxillary expansion appliances, regarding pain levels for growing patients.

Similar content being viewed by others
Data availability
All data are incorporated into the article and related tables and figures.
References
Allen D, Rebellato J, Sheats R, Ceron AM. Skeletal and dental contributions to posterior crossbites. Angle Orthod. 2003;73:515–24.
Altieri F, Cassetta M. The impact of tooth-borne vs computer-guided bone-borne rapid maxillary expansion on pain and oral health-related quality of life: a parallel cohort study. Am J Orthod Dentofacial Orthop. 2020;158:e83–90.
Baldini A, Nota A, Santariello C, Assi V, Ballanti F, Cozza P. Influence of activation protocol on perceived pain during rapid maxillary expansion. Angle Orthod. 2015;85:1015–20.
Bartzela TN, Senn C, Wichelhaus A. Load-deflection characteristics of superelastic nickel–titanium wires. Angle Orthod. 2007;77:991–8.
Betts N, Vanarsdall R, Barber H, Higgins-Barber K, Fonseca R. Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthodon Orthognath Surg. 1995;10:75–96.
Beyer JE, Wells N. The assessment of pain in children. Pediatr Clin North Am. 1989;36:837–54.
Bishara SE, Staley RN. Maxillary expansion: clinical implications. Am J Orthod Dentofac Orthop. 1987;91:3–14.
Braun S, Bottrel JA, Lee K-G, Lunazzi JJ, Legan HL. The biomechanics of rapid maxillary sutural expansion. Am J Orthod Dentofac Orthop. 2000;118:257–61.
Cleall JF, Bayne DI, Posen JM, Subtelny JD. Expansion of the midpalatal suture in the monkey. Angle Orthod. 1965;35:23–35.
de Araújo MC, Bocato JR, Berger SB, Oltramari PVP, de Castro Ferreira Conti AC, de Almeida MR, Freire Fernandes TM. Perceived pain during rapid maxillary expansion in children with different expanders. Angle Orthod. 2021;91:484–9.
Erverdi N, Okar I, Kücükkeles N, Arbak S. A comparison of two different rapid palatalexpansion techniques from the point of root resorption. Am J Orthod Dentofac Orthop. 1994;106:47–51.
Feldmann I, Bazargani F. Pain and discomfort during the first week of rapid maxillary expansion (RME) using two different RME appliances: a randomized controlled trial. Angle Orthod. 2017;87:391–6.
Gecgelen M, Aksoy A, Kirdemir P, Doguc D, Cesur G, Koskan O, Ozorak O. Evaluation of stress and pain during rapid maxillary expansion treatments. J Oral Rehabil. 2012;39:767–75.
George MS, Kusai A-MM. An assessment of efficiency of application of erbium-yag laser with rapid palatal expansion in decreasing pain resulted from active treatment: an in vivo study. Int J Dent Health Sci. 2016;3(2):336–48.
Haas AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. Angle Orthod. 1961;31:73–90.
Habersack K, Karoglan A, Sommer B, Benner KU. High-resolution multislice computerized tomography with multiplanar and 3-dimensional reformation imaging in rapid palatal expansion. Am J Orthod Dentofac Orthop. 2007;131:776–81.
Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006;15:S17–24.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Lagravere MO, Major PW, Flores-Mir C. Long-term skeletal changes with rapid maxillary expansion: a systematic review. Angle Orthod. 2005;75:1046–52.
Lennard TA, Vivian DG, Walkowski SD, Singla AK. Pain procedures in clinical practice E-book. Amsterdam: Elsevier Health Sciences; 2011.
Linder-Aronson S. Adenoids. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the denition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl. 1970;265:1–132.
Ma LL, Wang YY, Yang ZH, Huang D, Weng H, Zeng XT. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res. 2020;7:7.
Mason C, Porter S, Madland G, Parry J. Early management of dental pain in children and adolescents. J Dent. 1997;25:31–4.
Maunuksela EL, Olkkola KT, Korpela R. Measurement of pain in children with self-reporting and behavioral assessment. Clin Pharmacol Ther. 1987;42:137–41.
Murray JMG, Cleall JF. Early tissue response to rapid maxillary expansion in the midpalatal suture of the rhesus monkey. J Dent Res. 1971;50:1654–60.
Myers DR, Barenie JT, Bell RA, Williamson EH. Condylar position in children with functional posterior crossbites: before and after crossbite correction. Pediatr Dent. 1980;2:190–4.
Needleman HL, Hoang C, Allred E, Hertzberg J, Berde C. Reports of pain by children undergoing rapid palatal expansion. Pediatr Dent. 2000;22:221–6.
Nieri M, Paoloni V, Lione R, Barone V, Marino Merlo Jr M, Giuntini V, Cozza P, Franchi L. Comparison between two screws for maxillary expansion: a multicenter randomized controlled trial on patient’s reported outcome measures. Eur J Orthod. 2021;43:293–300.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Moher D. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol. 2021;134:103–12.
Petrén S, Bondemark L, Söderfeldt B. A systematic review concerning early orthodontic treatment of unilateral posterior crossbite. Angle Orthod. 2003;73:588–96.
Phillips C, Medland W, Fields H Jr, Proffit W, White R Jr. Stability of surgical maxillary expansion. Int J Adult Orthodon Orthognath Surg. 1992;7:139–46.
Proffit W (2000) Treatment of orthodontic problems in preadolescent children (section VI). WR Proffit Contemporary Orthodontics, 3rd ed St Louis: Mosby. 2000:435–9.
Ramoglu SI, Sari Z. Maxillary expansion in the mixed dentition: rapid or semi-rapid? Eur J Orthodont. 2010;32:11–8.
Romanyk D, Lagravere M, Toogood R, Major P, Carey J. Review of maxillary expansion appliance activation methods: engineering and clinical perspectives. J Dent Biomech. 2010;2010:496906.
Sandhu SS, Sandhu J. Orthodontic pain: an interaction between age and sex in early and middle adolescence. Angle Orthod. 2013;83:966–72.
Sandikçiolu M, Hazar S. Skeletal and dental changes after maxillary expansion in the mixed dentition. Am J Orthod Dentofac Orthop. 1997;111:321–7.
Santos-Gallego CG, Requena-Ibanez JA, Badimon J. Per-protocol versus intention-to-treat in clinical trials: the example of GLOBAL-LEADERS trial. J Am Heart Assoc. 2022;11: e025561.
Schuster G, Borel-Scherf I, Schopf PM. Frequency of and complications in the use of RPE appliances—results of a survey in the Federal State of Hesse, Germany. J Orofac Orthoped Fortschr Kieferorthop. 2005;66:148–61.
Silveira GS, Abreu LG, Palomo JM, da Matta Cid Pinto LS, de Sousa AA, Gribel BF, Oliveira DD. Mini Hyrax vs Hyrax expanders in the rapid palatal expansion in adolescents with posterior crossbite: a randomized controlled clinical trial. Progr Orthod. 2021;22:1–13.
Silvestrini-Biavati A, Angiero F, Gambino A, Ugolini A. Do changes in spheno-occipital synchondrosis after rapid maxillary expansion affect the maxillomandibular complex? Eur J Paediatr Dent. 2013;14:63–7.
Swieboda P, Filip R, Prystupa A, Drozd M. Assessment of pain: types, mechanism and treatment. Ann Agric Environ Med. 2013;1:2–7.
Ugolini A, Cossellu G, Farronato M, Silvestrini-Biavati A, Lanteri V. A multicenter, prospective, randomized trial of pain and discomfort during maxillary expansion: leaf expander versus hyrax expander. Int J Paediatr Dent. 2020a;30:421–8.
Ugolini A, Cossellu G, Farronato M, Silvestrini-Biavati A, Lanteri V. A multicenter, prospective, randomized trial of pain and discomfort during maxillary expansion: leaf expander versus hyrax expander. Int J Pediatr Dent. 2020b;30:421–8.
Usumez M, Uzel I. Evaluation of rapid maxillary expansion and quad-helix in the late mixed dentition period. Turk J Orthod. 2008;21:187–95.
Waldman S. Pain review: Chapter 277-thoracic sympathetic block. Philadelphia: Saunders-Elsevier; 2009.
Wang Z, Obamiyi S, Malik S, Rossouw PE, Tallents RH, Michelogiannakis D. Changes in condylar position with maxillary expansion in growing patients. A systematic review of clinical studies. Orthod Waves. 2020;79:1–10.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception, design, acquisition, data collection, analysis and interpretation of results. All authors participated in drafting the article and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any personal or financial conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Appendix
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Altuhafy, M., Jabr, L., Michelogiannakis, D. et al. Self-perceived pain in Hyrax versus other maxillary expansion orthodontic appliances: a systematic review of clinical studies. Eur Arch Paediatr Dent 24, 279–292 (2023). https://doi.org/10.1007/s40368-023-00795-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40368-023-00795-1