Abstract
Introduction
2018 ESC/ESH guidelines have recommended 24-h ambulatory blood pressure monitoring to assess hypotensive therapy in many circumstances. Recommended target blood pressure in office blood pressure measurements is between 120/70 and 130/80 mmHg. Such targets for 24-h ambulatory blood pressure monitoring lacks.
Aim
We aimed to define target values of blood pressure in 24-h ambulatory blood pressure monitoring in hypertensive patients.
Methods
Office blood pressure measurements and 24-h ambulatory blood pressure monitoring data were collected from 1313 hypertensive patients and sorted following increasing systolic (SBP)/diastolic (DBP) blood pressure in office blood pressure measurements. The corresponding 24-h ambulatory blood pressure monitoring to office blood pressure measurements values were calculated.
Results
Values 130/80 mmHg in office blood pressure measurements correspond in 24-h ambulatory blood pressure monitoring: night-time SBP/DBP mean: 113.74/66.95 mmHg; daytime SBP/DBP mean: 135.02/81.78 mmHg and 24-h SBP/DBP mean: 130.24/78.73 mmHg. Values 120/70 mmHg in office blood pressure measurements correspond in 24-h ambulatory blood pressure monitoring: night-time SBP/DBP mean: 109.50/63.43 mmHg; daytime SBP/DBP mean: 131.01/78.47 mmHg and 24-h SBP/DBP mean: 126.36/75.31 mmHg.
Conclusions
The proposed blood pressure target values in 24-h ambulatory blood pressure monitoring complement the therapeutic target indicated in the ESC/ESH recommendations and improves 24-h ambulatory blood pressure monitoring usefulness in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Arterial hypertension (AH) is the most common civilizational disease and a crucial factor for cardiovascular (CV) risk for morbidity and mortality. In 2015, the global prevalence of AH was 1.13 billion, accounting for 24% and 20% of AH cases in men and women, respectively [1].
According to the 2018 ESC/ESH guidelines, AH is diagnosed when office blood pressure (OBPM) measurements values ≥ 140/90 mmHg twice on two separated visits; when home blood pressure measurements (HBPM) average values ≥ 135/85 mmHg (mean of all blood pressure readings, taken technically correct twice in the morning and the evening for at least 3–7 consecutive days). AH can also be diagnosed based on ambulatory blood pressure monitoring (ABPM), which measures blood pressure (BP) values during the day and the night in 24-h period. The AH is diagnosed when ABPM 24h readings average ≥ 130/80 mmHg, daytime average ≥ 135/85 mmHg, and night-time average ≥ 120/70 mmHg [2].
According to the European guidelines, target BP values in patients treated due to AH should be less than 140/90 mmHg. Providing the therapy is well-tolerated, the following point in most patients is lowering the BP values below 130/80 mmHg. One of the exceptions is elderly patients over 65 years old, in which target values of systolic blood pressure (SBP) are between 130 and 140 mmHg, and diastolic blood pressure (DBP) should not be less than 80 mmHg. It is not recommended to reduce BP below 120/70 mmHg [2, 3]. This threshold was established due to the higher incidence rate of hospital admissions caused by heart failure and increased cardiovascular and all-cause mortality in patients achieving SBP below 120 mmHg or DBP below 70 mmHg during hypotensive treatment [3].
The actual ESH guidelines recommended BP monitoring with ABPM but did not provide clear target values in ABPM for well-treated AH. There are groups of patients for whom ABPM is a specially recommended form of assessment of BP, e.g., white coat hypertension (WCH); masked hypertension (MH); AH in pregnancy, children, adolescents and elderly, high-risk patients; nocturnal AH or endocrine AH [2, 4, 5]. The lack of objective criteria for BP monitoring in ABPM may lead to underestimate the necessary therapy, increasing the risk of chronic complications in the future.
The study aimed to define the BP control values specified for measurements performed at ABPM according to the 2018 ESH/ESC guidelines.
2 Methods
The OBPM and ABPM data used in the study were collected from consecutive hypertensive patients treated in the Department of Hypertensiology. Patients that are not yet treated were excluded. Enrolled patients had three conventional office blood pressure measurements and ABPM.
Measurements were made by the same appropriately validated devices for all patients. The selection of an appropriate cuff size depended on the arm circumference of each individual. We used a standard cuff (12–13 cm wide, 35 cm long) for most patients. Larger and smaller cuffs for larger (arm circumference > 32 cm) and thinner arms were available.
All patients gave informed consent to archive their data in the database. The study has the approval of the ethics committee. The patients' BP was measured according to the ESC/ESH guidelines and OBPM was measured on the same visit before starting ABPM (no more than 24 h of distance) [2, 6].
2.1 Office Blood Pressure Measurement
BP was measured thrice every 1–2 min with Omron M300 (HEM-7121-D) by physician. All readings were measured with the same device. The BP value was calculated as the average of the last two readings.
2.2 Ambulatory Blood Pressure Measurement
The device (A&D TM-2430) was set to measure and record the BP every 15 min between 6:00 AM to 9:59 PM and every 30 min between 10:00 PM to 5:59 AM. Wake time and sleep time were based on the patient's declaration. At least 70% of measurements and at least 20 valid readings while awake with at least two valid readings per hour and at least seven valid readings while asleep with at least one valid reading per hour had to be performed technically correct to declare the ABPM examination valid. The final data were presented as daytime mean, night-time mean and 24-h mean.
Patient data were sorted in accordance with increasing SBP or DBP in OBPM and divided into intervals of 5 ± 2.5 mmHg, i.e., measurement equal 127.3/79.2 mmHg was assigned to the interval 125±2.5 mmHg for SBP and 80 ± 2.5 mmHg for DBP. The selected patients' data were compiled in bigger groups if fewer than 50 patients were in the interval. Corresponding ABPM values for each compartment in OBPM were calculated as the arithmetic mean. The calculations were made in Microsoft Excel.
Due to the lack of distribution normality, the Spearman correlation coefficient was determined between OBPM and ABPM (Statistica Software).
3 Results
The study group comprised 1313 patients, including 589 women (44.9%) and 724 men (55.1%).
The mean age for the patients was: 54.86 ± 15.31. Patients were overweight (body mass index: 28.44 ± 5.22 kg/m2). The mean SBP/DBP in OBPM were respectively: 138.66 ± 18.47/81.36±11.92 mmHg. The mean SBP/DBP in ABPM were respectively: 138.88 ± 14.57/83.24 ± 9.36 mmHg (daytime mean); 117.73 ± 16.01/68.45 ± 10.29 mmHg (night-time mean); 134.4 ± 13.82/80.13 ± 8.93 mmHg (24-h mean).
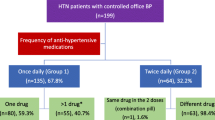
All patients were taking hypotensive drugs. An average equals three drugs per patient. 20% of patients used monotherapy. More than half of the patients had been taking angiotensin-converting enzyme inhibitors (59%), beta-blockers (55%) and calcium channel inhibitors (50%). 49% of patients were taking diuretics, 29%—angiotensin receptor blockers and 17%—the other hypotensive drugs.
Every second patient suffered from hyperlipidemia (54%); one fifth had thyroid disease (18%) or diabetes (22%); every eighth patient was diagnosed with ischemic heart disease (12%), arrhythmia (12%) or peripheral vascular disease (13%). Less than 5% of patients were diagnosed with chronic kidney disease, heart failure, glaucoma, stroke or transient ischemic attack. The population division is respectively: 36.9% for MH and 14.2% for WCH. The characteristics of the study groups are presented in Supplement 1.
The OBPM and corresponding mean BP values in ABPM according to intervals were compared. Obtained results are presented in Table 1. Office BP intervals increased with values corresponding to those in ABPM. This relationship was visible both in SBP and DBP. Deviations from this relationship are visible at extreme values. This is due to the small number of measurements in a given interval.
We demonstrated a statistically significant correlations (p < 0.01) between OBPM and ABPM values. The Spearman correlation coefficient was determined, which amounted to r = 0.59 (SBP OBPM and SBP 24-h mean) and r = 0.64 (DBP OBPM and DBP 24-h mean), r = 0.4 (SBP OBPM and SBP daytime mean) and r = 0.61 (DBP OBPM and DBP daytime mean), r = 0.49 (SBP OBPM and SBP night-time mean) and r = 0.64 (DBP OBPM and DBP night-time mean).
4 Discussion
4.1 BP Targets for Hypotensive Therapy
2018 ESH/ESC guidelines define appropriate BP targets in OBPM during hypotensive therapy. However, these values are not the same in all AH patients. European guidelines recommend lowering OBPM, in the general population of patients with AH, below 140/90 mmHg, and if tolerating therapy to below 130/80 mmHg, but not less than 120/70 mmHg. For patients with type 2 diabetes or coronary artery disease, it is recommended to achieve SBP values below 130 mmHg but not less than 120 mmHg. In the group of patients with AH ≥ 65 years of age, SBP values should be between 130 and 139 mmHg and DBP between 80 and 70 mmHg. Therefore, the guidelines recommend different values of well-controlled AH in OBPM in different patient groups [2]. The criteria for controlled AH in the ESH guidelines were based on “hard” endpoints from studies evaluating office BP only [2, 7]. There are no similar studies based on ABPM [2]. The diagnosis limit of AH for ABPM was based on a study comparing office BP with ABPM [5, 8,9,10]. We performed a comparison of these two types of measurements in a large group, pointing to values that have been identified as targets.
Therefore, the study aimed to define the BP control values performed at ABPM. According to the 2018 ESC/ESH guidelines, we established values in ABPM that correspond to treated AH in OBPM [2]. Values 130/80 mmHg in OBPM correspond in ABPM: night-time SBP/DBP mean: 113.74/66.95 mmHg; daytime SBP/DBP mean: 135.02/81.78 mmHg and 24-h SBP/DBP mean: 130.24/78.73 mmHg. Values 120/70 mmHg in OBPM correspond in ABPM: night-time SBP/DBP mean: 109.50/63.43 mmHg; daytime SBP/DBP mean: 131.01/78.47 mmHg and 24-h SBP/DBP mean: 126.36/75.31 mmHg.
American Heart Association 2017 guidelines (2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults) are one of the few that suggest the values of well-treated AH in ABPM corresponding to a specific BP value in OBPM and HBPM. These guidelines define the target BPs for ABPM corresponding to the value’s of 130/70 mmHg in OBPM, which are night-time SBP/DBP mean, respectively: 110/65 mmHg; daytime SBP/DBP mean: 130/80 mmHg and 24-h SBP/DBP mean: 125/75 mmHg. There are no corresponding values for OBPM 120/70 mmHg [11]. Therefore, in the case of 130/80 mmHg values, the target values in ABPM proposed by the AHA are relatively similar to those obtained in the present study. Differences may be due to a different calculation method. American guidelines target ABPM values were based on CV risk [9,10,11,12].
Kario et al. in Expert panel consensus recommendations for ambulatory blood pressure monitoring in Asia: The HOPE Asia Network set strict ABPM thresholds for AH based on 2017 AHA guidelines (Class of recommendation: IIa, level of evidence: C). The authors believe that the only way to achieve BP targets is regularly repeating ABPM. When the patient reaches well-controlled BP, experts recommend repeat ABPM. The higher the cardiovascular risk, the more frequent control [13].
4.2 Special Subtypes of AH Patients
OBPM is an accessible, cheap and simple method to assess AH. However, as experts emphasized, the measurements were often not appropriately done, resulting in misdiagnosis of AH and the unnecessary treatment of patients. ABPM is the more expensive and difficult method to diagnose and assess AH. However, there are groups of patients with AH for whom OBPM is insufficient and ABPM is essential for objective assessment of BP control [2].
A special group are those with the WCH (where OBPM are higher than those in HBPM or ABPM) and AH patients with MH (where OBPM are correct, but not in HBPM and ABPM), AH in pregnancy or elderly patients. During antihypertensive therapy, assessing BP values based on ABPM is indispensable, particularly in the groups above [2, 5, 6, 14]. Perhaps this group should include patients with diabetes in whom achieving adequate BP control seems particularly difficult [15].
There are few studies in which ABPM was used to monitor BP values during hypotensive therapy. In the RAMBLER study, which assessed the role of ABPM in routine clinical practice, more than 30% of AH patients achieved BP target with ABPM compared with 12% of patients with OBPM [16]. Nsutebu et al. assessed the use of ABPM in BP monitoring and modifying hypotensive therapy. About 52% of treated AH patients had changed their treatment after BP control in ABPM. The hypotensive therapy did not change or was reduced in the groups of patients with white-coat uncontrolled AH and sustained controlled AH. Therapy was intensified in the groups of patients with masked uncontrolled AH and true uncontrolled AH. The authors showed that using ABPM in patients with AH, including masked uncontrolled AH and WCH, helped in making therapeutic decisions and obtaining better control of BP values [17]. Banegas et al. assessed the use of ABPM in assessing AH treatment in the elderly population (≥ 60 years old). The use of ABPM reduced the number of older patients who needed hypotensive therapy and increased the number of patients with well-controlled AH. Penny et al. compared, in a group of over 300 pregnant women with AH, the use of OBPM versus ABPM as a predictor of severe AH. ABPM was a better tool for prognosing the course of pregnancy than OBPM. Using ABPM improved SBP sensitivity from 14 to 27% and DBP from 7 to 39% [4]. Youssef et al. assessed prevalence and predictors for masked uncontrolled AH. More than 30% of patients with apparently well-controlled AH (OBPM < 140/90 mmHg) had an abnormal BP in ABPM, which allowed researchers to recognize masked uncontrolled AH. In most cases, the abnormal ABPM was due to higher BP values at night than during the day (57.3 vs 27.1%, p < 0.001) [18]. OBPM is an insufficient method to assess the control of AH treatment in this group of patients, and ABPM is needed to confirm proper BP control during the day and night. Neither OBPM nor HBPM will assess BP while sleep-time, which gives a significant advantage to ABPM as a method for assessing AH treatment [2].
In the general group of treated AH patients, about 30% have MH [19, 20]. WCH is also common, observed in 30–40% of AH patients (> 50% in the elderly) [2]. WCH is uncommon in patients with resistant AH (6.5%) [4]. Based on data from the SPRINT (Systolic Blood Pressure Intervention Trial), the incidence of WCH in treated AH patients was approximately 10% [21]. In another study, the prevalence of WCH was 31–35% in primary AH patients [22].
The diagnosis and control treatment of MH/WCH patients by ABPM seems to be particularly important considering the presence of organ damage and increased cardiovascular (CV) risk in long-term follow-up. It is not certain whether WCH is a clinically significant phenomenon [23]. Asymptomatic organ damage was often observed in WCH patients [24,25,26]. Additionally, an increased CV risk is observed in long-term follow-up [27, 28].
MH patients characterise with more frequent diabetes mellitus, chronic kidney disease and high CV risk [29]. Few studies assessed hard endpoints in the MH group. Considering high CV risk profile, ESH/ESC guidelines recommends intensifying hypotensive treatment in these group [2].
The diagnosis of MH or WCH is essential for hypotensive management adjustment. Basing on OBPM, WCH patients may receive higher doses of hypotensive drugs, leading to lower BP values in HBPM. On the other side, MH patients may have abnormal BP in HBPM due to insufficient therapy [30].
The population division in our study is respectively: 36.9% for MH and 14.2% for WCH. The incidence of WCH and MH in the study population is consistent with the frequency reported in the literature. The results of NATPOL 2011 study showed that patients with AH were overweight like in presented study. Body mass index for men and women was: 27.2 and 26.1 kg/m2 [31]. The proposed study BP targets can be recognized as universal for the entire AH patient population.
4.3 Comparison with the Other Studies
Head et al. showed ABPM equivalents to clinic BP thresholds for diagnosis and AH treatment. The authors calculate ABPM equivalents for OBPM using product linear regression equations. The daytime mean in ABPM for clinical 140/90 mmHg was 4/3 mmHg lower than the clinic values. For clinical 130/80 mmHg, the daytime mean in ABPM was 2/2 mmHg lower, and for clinical 125/75 mmHg, the daytime mean in ABPM was 1/1 mmHg lower. The difference between OBPM and ABPM was higher when the patients had more elevated OBPM. Ambulatory values were lower for women versus men (SBP/DBP: 1/2 mmHg) and lower in people ≥ 65 years (SBP/DBP: 3/1 mmHg) [32].
The values calculated in our study are higher than those proposed by Head et al. However, the conclusions regarding the relationship between OBPM-ABPM are consistent. It is difficult to say which values are more appropriate. We will get the answer only after conducting an appropriately planned study evaluating hard endpoints. Differences in results may arise from several issues. Head et al. made a pervasive analysis. We made a simple calculation, which may put our work in a worse light. An important issue, is the variability of AH depending on the studied population. The group analyzed in the present study is the population of Central Europe. Head et al. analyzed data of people from Australia. Every population can have a different prevalence of WCH, MH or non-dipper patients. Head et al., in their study, compare BP values measured by medical trained staff, not by physician. Authors believe that the values measured by doctors cause the result to be inflated [32]. Perhaps a more appropriate method would be to take the mean of the doctors and other medical personnel's measurements. The calculations are valid only for the daytime; the value for the night-time is missing. The night-time is a parameter that can only be assessed using ABPM.
4.4 Limitation
Presented targets BP has limitations. The study only considers current BP in treated AH patients. Patients had BP measurements only once. Certainly, better would be to assess the presented data if we had more measurements in a few months or years. It would allow a better assessment of the patient's BP level than a single measurement. In addition, to properly examine the correspondence of OBPM to ABPM, it is necessary to have a baseline CV risk stratification, CV diseases interview assessment, as well as factors influencing these values (e.g. individual response to treatment, adverse effects). Such an assessment would be possible, among others in the SPRINT [33].
In the SPRINT study, treatment lowering clinic SBP below 120 mmHg versus below 140 mmHg, impacted significant reductions in CV events (25%) and mortality (27%). The authors suggest another stringent target BP during AH treatment. It should be remembered that the study used a less popular method of BP measurement-unattended office BP measurement [33]. The method is considered quite controversial compared to conventional BP measurement, which is more often done in clinical trials [2].
Drawz et al., in SPRINT ambulatory blood pressure ancillary study, analyzed the effect of clinic-based intensive AH treatment on ABPM. The intensification of AH treatment based on clinical measurements (SBP < 120 mmHg) significantly reduced all BP parameters in ABPM, also reduced BP variability [34]. The study group was very similar in clinical characteristics to those in the SPRINT [33]. The results of Drawz et al. strengthened the role of ABPM in AH treating. It showed the importance of appropriately selecting BP measurement techniques when we want to identify BP targets in clinical trials [34, 35].
The next problem, concerning presented results, is related to the individual variability in OBPM-ABPM difference. The prevalence of WCH and MH or non-dipper patients, definitely impact the results. As we previously wrote, every subtype of AH has different clinical prognostic significance [2].
ABPM is usually lower than OBPM [34, 35]. Our results show an inverse relationship between the values of SBP in OBPM 135 mmHg and lower. One might wonder if the OBPM in the group below office SBP < 135 mmHg were not incorrectly performed or performed by a different method. If we used the unattended office BP measurement, it would be a reasonable explanation because the measurement is 5–15 mmHg lower than OBPM [2, 33]. Analysis of the single ABPM results showed that there are relatively many patients with MH in this group, which is probably the reason for the observed relationship. Therefore in future analysis, maybe will be necessary to calculate different targets BP for patients with AH subtypes.
We were unable to present the results broken down by age and gender due to small sample sizes and inhomogeneous in particular subgroups.
5 Conclusion
Several guidelines recommend the use of ABPM to evaluate AH treatment. Although these recommendations are becoming stronger over time, the exact BP values in ABPM of well-controlled AH are still lacking [2, 5, 6, 13, 36,37,38].
In clinical practice, the values defined as well-controlled AH are often used to evaluate AH treatment in ABPM (24 h readings average ≥ 130/80 mmHg, daytime average ≥ 135/85 mmHg, and night-time average ≥ 120/70 mmHg). However, since they correspond to OBPM at 140/90 mmHg, they are not universal for all AH patients. Moreover, according to 2018 ESH guidelines, lower values defined well-controlled AH [2].
Therefore, in the case of the lower limit of OBPM, i.e., 120/70 mmHg, the ABPM should be analyzed with precise accuracy not to achieve too low BP values. If the AHA target of OBPM values were considered correct (OBPM < 130/80 mmHg or less), patients would be taking more antihypertensive drugs, resulting in a higher risk of hypotension. Lowering the BP below 120/70 mmHg could result in higher CV risk [3]. Without BPs target in ABPM in line with OBPM norms in the ESH guidelines, the ABPM becomes useless in controlling BP treatment, and its use is limited to diagnosing AH.
Defining objective criteria for BP monitoring in ABPM would improve the assessment of the need for implementing or modifying of hypotensive treatment. Such an approach will reduce the risk of long-term complications of AH. We propose ABPM's target values that should be reached in patients with AH. The above calculations do not include the correlation with CV risk. To confirm the validity of the above values, it is necessary to conduct a large clinical trial evaluating “hard” endpoints in patients on hypotensive therapy.
References
Zhou B, Bentham J, Cesare M, Bixby H, Danaei G, Cowan M, Paciorek C, Singh G, Hajifathalian K, Bennett J, Taddei C, Bilano V, Carrillo-Larco R, Djalalinia S, Khatibzadeh S, Lugero C, Peykari N, Zhang W, Lu Y, Stevens G, Riley L, Bovet P, Elliott P, Gu D, Ikeda N, Jackson R, Joffres M, Kengne A, Laatikainen T, Lam T, Laxmaiah A, Liu J, Miranda J, Mondo C, Neuhauser H, Sundström J, Smeeth L, Soric M, Woodward M, Ezzati M. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017. https://doi.org/10.1016/S0140-6736(16)31919-5.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement D, Coca Ade Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen S, Kreutz R, Laurent S, Lip G, McManus R, Narkiewicz K, Ruschitzka F, Schmieder R, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I. ESC/ESH guidelines for the management of arterial hypertension. The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018. https://doi.org/10.1093/EURHEARTJ/EHY339.
Böhm M, Schumacher H, Teo KK, Lonn EM, Mahfoud F, Mann JFE, Mancia G, Redon J, Schmieder RE, Sliwa K, Weber MA, Williams B, Yusuf S. Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Lancet. 2017. https://doi.org/10.1016/S0140-6736(17)30754-7.
Siddiqui M, Judd EK, Oparil S, Calhoun DA. White coat effect is uncommon in patients with refractory hypertension. Hypertension. 2017. https://doi.org/10.1161/HYPERTENSIONAHA.117.09464.
Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, Clement D, De La Sierra A, De Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, Van Montfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y. European society of hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014. https://doi.org/10.1097/HJH.0000000000000221.
Stergiou GS, Palatini P, Parati G, O’Brien E, Januszewicz A, Lurbe E, Persu A, Mancia G, Kreutz R. European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021. https://doi.org/10.1097/HJH.0000000000002843.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 7. Effects of more vs. less intensive blood pressure lowering and different achieved blood pressure levels—updated overview and meta-analyses of randomized trials. J Hypertens. 2016. https://doi.org/10.1097/HJH.0000000000000881.
Pickering TG, White WB. ASH position paper: home and ambulatory blood pressure monitoring. When and how to use self (Home) and ambulatory blood pressure monitoring. J Clin Hypertens. 2008. https://doi.org/10.1111/J.1751-7176.2008.00043.X.
Hansen TW, Kikuya M, Thijs L, Björklund-Bodegård K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Jeppesen J, Ibsen H, Imai Y, Staessen JA. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J Hypertens. 2007. https://doi.org/10.1097/HJH.0B013E3281C49DA5.
Kikuya M, Hansen TW, Thijs L, Björklund-Bodegård K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Staessen JA. Diagnostic thresholds for ambulatory blood pressure monitoring based on 10-year cardiovascular risk. Circulation. 2007. https://doi.org/10.1161/CIRCULATIONAHA.106.662254.
Whelton P, Carey R, Aronow W, Casey D, Collins K, Dennison Himmelfarb C, DePalma S, Gidding S, Jamerson K, Jones D, MacLaughlin E, Muntner P, Ovbiagele B, Smith S, Spencer C, Stafford R, Taler S, Thomas R, Williams K, Williamson J, Wright J. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2017. https://doi.org/10.1161/HYP.0000000000000065.
Ravenell J, Shimbo D, Booth JN, Sarpong DF, Agyemang C, Moody DLB, Abdalla M, Spruill TM, Shallcross AJ, Bress AP, Muntner P, Ogedegbe G. Thresholds for ambulatory blood pressure among African Americans in the Jackson Heart Study. Circulation. 2017. https://doi.org/10.1161/CIRCULATIONAHA.116.027051.
Kario K, Shin J, Chen CH, Buranakitjaroen P, Chia YC, Divinagracia R, Nailes J, Hoshide S, Siddique S, Sison J, Soenarta AA, Sogunuru GP, Tay JC, Teo BW, Turana Y, Zhang Y, Park S, Van Minh H, Wang JG. Expert panel consensus recommendations for ambulatory blood pressure monitoring in Asia: the HOPE Asia Network. J Clin Hypertens. 2019. https://doi.org/10.1111/JCH.13652.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M, Wainford RD, Williams B, Schutte AE. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020. https://doi.org/10.1161/HYPERTENSIONAHA.120.15026.
De Feo M, Del Pinto R, Pagliacci S, Grassi D, Ferri C, Grassi G, Muiesan ML, Salvetti M, Sechi L, Cicero AFG, Iaccarino G, Minuz P, Mulatero P, Mulè G, Pucci G, Savoia C, Borghi C, Volpe M. Real-world hypertension prevalence, awareness, treatment, and control in adult diabetic individuals: an Italian Nationwide Epidemiological Survey. High Blood Press Cardiovasc Prev. 2021. https://doi.org/10.1007/S40292-021-00449-7.
Uallachain GN, Murphy G, Avalos G. The RAMBLER study: the role of ambulatory blood pressure measurement in routine clinical practice: a cross-sectional study-PubMed. Ir Med J. 2006;99:276–9.
Nsutebu NS, Owusu IK, Buabeng KO, Bonsu KO. Ambulatory blood pressure monitoring and management of hypertension at a cardiac clinic in Kumasi Metropolis, Ghana. J Clin Hypertens. 2020. https://doi.org/10.1111/JCH.13822.
Youssef G, Nagy S, El-gengehe A, Abdel Aal A, Hamid MA. Masked uncontrolled hypertension: prevalence and predictors. Egypt Hear J. 2018. https://doi.org/10.1016/J.EHJ.2018.10.001.
Banegas JR, Ruilope LM, De La Sierra A, De La Cruz JJ, Gorostidi M, Segura J, Martell N, García-Puig J, Deanfield J, Williams B. High prevalence of masked uncontrolled hypertension in people with treated hypertension. Eur Heart J. 2014. https://doi.org/10.1093/EURHEARTJ/EHU016.
Naser N, Dzubur A, Durak A, Kulic M, Naser N. Blood pressure control in hypertensive patients, cardiovascular risk profile and the prevalence of masked uncontrolled hypertension (MUCH). Med Arch. 2016. https://doi.org/10.5455/MEDARH.2016.70.274-279.
Ghazi L, Cohen LP, Muntner P, Shimbo D, Drawz PE. Effects of intensive versus standard office-based hypertension treatment strategy on white-coat effect and masked uncontrolled hypertension: from the SPRINT ABPM ancillary study. Hypertension. 2020. https://doi.org/10.1161/HYPERTENSIONAHA.120.15300.
Zhu N, Bu M, Chen D, Li T, Qian J, Yu Q, Chen Q, Wan C, Qu H, Zhu M, Zou X. A study of the white-coat phenomenon in patients with primary hypertension. Hypertens Res. 2008. https://doi.org/10.1291/hypres.31.37.
Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension. 2006. https://doi.org/10.1161/01.HYP.0000215363.69793.BB.
Høegholm A, Bang LE, Kristensen KS, Nielsen JW, Holm J. Microalbuminuria in 411 untreated individuals with established hypertension, white coat hypertension, and normotension. Hypertension. 1994. https://doi.org/10.1161/01.HYP.24.1.101.
Kario K, Shimada K, Schwartz JE, Matsuo T, Hoshide S, Pickering TG. Silent and clinically overt stroke in older Japanese subjects with white-coat and sustained hypertension. J Am Coll Cardiol. 2001. https://doi.org/10.1016/S0735-1097(01)01325-0.
Sega R, Trocino G, Lanzarotti A, Carugo S, Cesana G, Schiavina R, Valagussa F, Bombelli M, Giannattasio C, Zanchetti A, Mancia G. Alterations of cardiac structure in patients with isolated office, ambulatory, or home hypertension: data from the general population (Pressione Arteriose Monitorate E Loro Associazioni [PAMELA] study). Circulation. 2001. https://doi.org/10.1161/HC3701.096100.
Mancia G, Bombelli M, Facchetti R, Madotto F, Quarti-Trevano F, Friz HP, Grassi G, Sega R. Long-term risk of sustained hypertension in white-coat or masked hypertension. Hypertension. 2009. https://doi.org/10.1161/HYPERTENSIONAHA.109.129882.
Mancia G, Bombelli M, Facchetti R, Madotto F, Quarti-Trevano F, Grassi G, Sega R. Increased long-term risk of new-onset diabetes mellitus in white-coat and masked hypertension. J Hypertens. 2009. https://doi.org/10.1097/HJH.0B013E32832BE5F9.
Shi X, Zhang K, Wang P, Kan Q, Yang J, Wang L, Yuan H. Association of masked uncontrolled hypertension and cardiovascular diseases in treated hypertensive patients. Arch Med Sci. 2020. https://doi.org/10.5114/AOMS.2019.89218.
Pioli MR, Ritter AMV, de Faria AP, Modolo R. White coat syndrome and its variations: differences and clinical impact. Integr Blood Press Control. 2018. https://doi.org/10.2147/IBPC.S152761.
Zdrojewski T, Rutkowski M, Bandosz P, Gaciong Z, Solnica G, Drygas W, Wojtyniak B, Stokwiszewski J, Pencina MJ, Wołkiewicz E, Piwonski J, Jędrzejczyk T, Grodzicki T, Wyrzykowski B. Ocena rozpowszechnienia i kontroli czynników ryzyka chorób serca i naczyń w Polsce—adania NATPOL 1997, 2002, 2011. Epidemiologia i Prewencja Chorób Układu Krążenia, 1st edn. 2015.
Head GA, Mihailidou AS, Duggan KA, Beilin LJ, Berry N, Brown MA, Bune AJ, Cowley D, Chalmers JP, Howe PRC, Hodgson J, Ludbrook J, Mangoni AA, McGrath BP, Nelson MR, Sharman JE, Stowasser M. Definition of ambulatory blood pressure targets for diagnosis and treatment of hypertension in relation to clinic blood pressure: prospective cohort study. BMJ. 2010. https://doi.org/10.1136/BMJ.C1104.
Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC Jr, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015. https://doi.org/10.1056/NEJMOA1511939.
Drawz PE, Pajewski NM, Bates JT, Bello NA, Cushman WC, Dwyer JP, Fine LJ, Goff DC, Haley WE, Krousel-Wood M, McWilliams A, Rifkin DE, Slinin Y, Taylor A, Townsend R, Wall B, Wright JT, Rahman M. Effect of intensive versus standard clinic-based hypertension management on ambulatory blood pressure: results from the SPRINT (Systolic Blood Pressure Intervention Trial) ambulatory blood pressure study. Hypertension. 2017. https://doi.org/10.1161/HYPERTENSIONAHA.116.08076.
Parati G, Ochoa JE, Bilo G, Zanchetti A. SPRINT blood pressure. Hypertension. 2017. https://doi.org/10.1161/HYPERTENSIONAHA.116.08216.
Gabb GM, Mangoni A, Anderson CS, Cowley D, Dowden JS, Golledge J, Hankey GJ, Howes FS, Leckie L, Perkovic V, Schlaich M, Zwar NA, Medley TL, Arnolda L. Guideline for the diagnosis and management of hypertension in adults-2016. Med J Aust. 2016. https://doi.org/10.5694/MJA16.00526.
Siu AL, Bibbins-Domingo K, Grossman D, Baumann LC, Davidson KW, Ebell M, García FAR, Gillman M, Herzstein J, Kemper AR, Krist AH, Kurth AE, Owens DK, Phillips WR, Phipps MG, Pignone MP. Screening for high blood pressure in adults: US Preventive Services task force recommendation statement. Ann Intern Med. 2015. https://doi.org/10.7326/P15-9036.
Liu J. Highlights of the 2018 Chinese hypertension guidelines. Clin Hypertens. 2020;2:3. https://doi.org/10.1186/S40885-020-00141-3.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by all authors. The first draft of the manuscript was written by KL, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Funding
The whole or part of the work was not previously presented in the article. The authors did not receive support from any organization for the submitted work. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Conflict of interest
None declared.
Ethical standards
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Poznan University of Medical Sciences.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lewandowska, K., Wasiliew, S., Kukfisz, A. et al. Target Blood Pressure Values in Ambulatory Blood Pressure Monitoring. High Blood Press Cardiovasc Prev 30, 29–36 (2023). https://doi.org/10.1007/s40292-022-00552-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-022-00552-3