Abstract
Introduction
Hyperuricemia is related to health issues among children and adolescents, once the uric acid concentration is associated with metabolic syndrome, hypertension, insulin resistance, obesity, and dyslipidemia. However, few studies are addressing uric acid levels and food uptake in this age group.
Aim
To verify the association between food consumption and uric acid in children and adolescents.
Methods
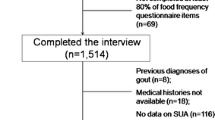
This is a cross-sectional study developed with 2335 children and adolescents of both genders aged 6–17 years old. Blood collection was performed after 12 h of fasting. Uric acid values were classified according to tertiles, in which the highest tertile was considered as hyperuricemia. Food consumption was evaluated by weekly consumption frequency questionnaire. Pearson correlation and logistic binary regressions were used for statistical analysis. Models were adjusted for age, systolic blood pressure, body mass index (BMI), and skin color/ethnicity.
Results
It was found an association between red meat consumption and hyperuricemia only in boys in the crude model (OR = 1.56; 95% CI 1.12; 2.18). Also, there was an association between pasta (OR = 1.52; 95% CI 1.11; 2.10) with hyperuricemia in boys, when adjusted age, systolic blood pressure, BMI, and skin color/ethnicity.
Conclusion
The knowledge of food patterns which are predisposing factors for the increase in serum uric acid levels is important for the implementation of strategies and public health policies for health promotion among children and adolescents.
Similar content being viewed by others
Data availability
The dataset analyzed during the current study is available from the corresponding author on a reasonable request.
References
Ford ES, Choi HK. Associations between concentrations of uric acid with concentrations of vitamin A and beta-carotene among adults in the United States. Nutr Res. 2013;33(12):995–1002. https://doi.org/10.1016/j.nutres.2013.08.008.
Schmidt JA, Crowe FL, Appleby PN, Key TJ, Travis RC. Serum uric acid concentrations in meat eaters, fish eaters, vegetarians and vegans: a cross-sectional analysis in the EPIC-Oxford cohort. PLoS ONE. 2013;8(2):e56339. https://doi.org/10.1371/journal.pone.0056339.
Liu D, Jiang L, Gan L, Su Y, Li F. Association between serum uric acid level and body mass index in sex—and age-specific groups in southwestern China. Endocr Pract. 2019;25(5):438–45. https://doi.org/10.4158/EP-2018-0426.
Batt C, Phipps-Green AJ, Black MA, Cadzow M, Merriman ME, Topless R, et al. Sugar-sweetened beverage consumption: a risk factor for prevalent gout with SLC2A9 genotype-specific effects on serum urate and risk of gout. Ann Rheum Dis. 2014;73(12):2101–6. https://doi.org/10.1136/annrheumdis-2013-203600.
Genoni G, Menegon V, Secco GG, Sonzini M, Martelli M, Castagno M, et al. Insulin resistance, serum uric acid and metabolic syndrome are linked to cardiovascular dysfunction in pediatric obesity. Int J Cardiol. 2017;249:366–71. https://doi.org/10.1016/j.ijcard.2017.09.031.
Liu Z, Chen T, Niu H, Ren W, Li X, Cui L, et al. The establishment and characteristics of rat model of atherosclerosis induced by hyperuricemia. Stem Cells Int. 2016;2016:1–7. https://doi.org/10.1155/2016/1365257.
Falsetti P, Acciai C. Oral vitamin C supplementation and serum uric acid: Comment on the article by Juraschek et al. Arthritis Care Res. 2012;64(6):941–4. https://doi.org/10.1002/acr.21614.
Tsai Y-T, Liu J-P, Tu Y-K, Lee M-S, Chen P-R, Hsu H-C, et al. Relationship between dietary patterns and serum uric acid concentrations among ethnic Chinese adults in Taiwan. Asia Pac J Clin Nutr. 2012;21(2):263–70.
Zykova SN, Storhaug HM, Toft I, Chadban SJ, Jenssen TG, White SL. Cross-sectional analysis of nutrition and serum uric acid in two Caucasian cohorts: the AusDiab Study and the Tromsø study. Nutr J. 2015;14(1):1–11. https://doi.org/10.1186/s12937-015-0032-1.
Jia G, Aroor AR, Whaley-Connell AT, Sowers JR. Fructose and uric acid: is there a role in endothelial function? Curr Hypertens Rep. 2014;16(6):434. https://doi.org/10.1007/s11906-014-0434-z.
Nguyen S, Choi HK, Lustig RH, Hsu C. Sugar-sweetened beverages, serum uric acid, and blood pressure in adolescents. J Pediatr. 2009;154(6):807–13. https://doi.org/10.1016/j.jpeds.2009.01.015.
Mosca A, Nobili V, De Vito R, Crudele A, Scorletti E, Villani A, et al. Serum uric acid concentrations and fructose consumption are independently associated with NASH in children and adolescents. J Hepatol. 2017;66(5):1031–6. https://doi.org/10.1016/j.jhep.2016.12.025.
Zhao Y, Yu Y, Li H, Li M, Zhang D, Guo D, et al. The association between metabolic syndrome and biochemical markers in beijing adolescents. Int J Environ Res Public Health. 2019;16(22):1–10. https://doi.org/10.3390/ijerph16224557.
Kubota M. Hyperuricemia in children and adolescents: present knowledge and future directions. J Nutr Metab. 2019. https://doi.org/10.1155/2019/3480718.
Hyun LJ. Prevalence of hyperuricemia and its association with metabolic syndrome and cardiometabolic risk factors in korean children and adolescents: analysis based on the 2016–2017 korea national health and nutrition examination survey. Korean J Pediatr. 2019;62(8):317–23. https://doi.org/10.3345/kjp.2019.00444.
Mariz L, Medeiros C, Vieira C, Enders B, Coura A. Modificação na frequência alimentar de crianças e adolescentes: acompanhamento em serviço de referência. Revista Latino-Americana de Enfermagem. 2013;21(4):973–81. https://doi.org/10.1590/S0104-11692013000400020.
Ramayani ORE. Childhood hyperuricemia as risk factor of hypertension in adulthood. Indones Biomed J. 2012;4(1):12. https://doi.org/10.18585/inabj.v4i1.156.
Brasil. Agenda Nacional de Prioridades de Pesquisa em Saúde. 2. ed., 4. Brasília: Editora do Ministério da Saúde; 2015, p 68.
Barros MVG, Nahas M V. Medidas de Atividade Física: Teoria e Aplicação em Diversos Grupos Populacionais. Tópicos em Atividade Física e Saúde. 2003. p. 160.
Suttikomin W, Leelahagul P, Khamvang S, Chaimongkol C, Chaiwut N. Obesity and serum uric acid in secondary school-age students of srinagarindra the princess mother school, Phayao, Thailand. Indian J Public Health. 2018;62(2):133–7. https://doi.org/10.4103/ijph.IJPH_117_17.
Feig DI, Johnson RJ. Hyperuricemia in childhood primary hypertension. Hypertension. 2003;42(3):247–52. https://doi.org/10.1161/01.HYP.0000085858.66548.59.
Desideri G, Virdis A, Casiglia E, Borghi C, Cicero AFG, Muiesan ML, et al. Exploration into uric and cardiovascular disease: uric acid right for heArt Health (URRAH) Project, a study protocol for a retrospective observational study. High Blood Press Cardiovasc Prev. 2018;25(2):197–202. https://doi.org/10.1007/s40292-018-0250-7.
Heidemann C, Scheidt-Nave C, Richter A, Mensink GBM. Dietary patterns are associated with cardiometabolic risk factors in a representative study population of German adults. Br J Nutr. 2011;106(8):1253–62. https://doi.org/10.1017/S0007114511001504.
Li X, Song P, Li J, Wang P, Li G. Relationship between hyperuricemia and dietary risk factors in Chinese adults: a cross-sectional study. Rheumatol Int. 2015;35(12):2079–89. https://doi.org/10.1007/s00296-015-3315-0.
Stöckl D, Döring A, Thorand B, Heier M, Belcredi P, Meisinger C. Reproductive factors and serum uric acid levels in females from the general population: the KORA F4 study. PLoS ONE. 2012;7(3):e32668. https://doi.org/10.1371/journal.pone.0032668.
Kolz M, Johnson T, Sanna S, Teumer A, Vitart V, Perola M, et al. Meta-analysis of 28,141 individuals identifies common variants within five new loci that influence uric acid concentrations. PLoS Genet. 2009. https://doi.org/10.1371/journal.pgen.1000504.
Redon P, Maloberti A, Facchetti R, Redon J, Lurbe E, Bombelli M, et al. Gender-related differences in serum uric acid in treated hypertensive patients from central and east European countries: findings from the blood pressure control rate and cardiovascular risk profile study. J Hypertens. 2019;37(2):380–8. https://doi.org/10.1097/HJH.0000000000001908.
Maloberti A, Maggioni S, Occhi L, Triglione N, Panzeri F, Nava S, et al. Sex-related relationships between uric acid and target organ damage in hypertension. J Clin Hypertens. 2018;20(1):193–200. https://doi.org/10.1111/jch.13136.
Acknowledgements
We acknowledge the National Council for Scientific and Technological Development (CNPq) and Coordination for the Improvement of Higher Education Personnel (CAPES), for the granting of a scholarship that made this work possible.
Author information
Authors and Affiliations
Contributions
LNR and CPR conceptualized and designed the study. LNR, LB, CB, and CPR acquired the data, carried out the analyses, interpreted the data, and drafted the article. CB, SIRF, JDPR, ARG, and JBS critically reviewed the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University Santa Cruz do Sul (July 10, 2014).
Rights and permissions
About this article
Cite this article
Reis, L.N., Borfe, L., Brand, C. et al. Food Consumption is Associated with Hyperuricemia in Boys. High Blood Press Cardiovasc Prev 27, 409–415 (2020). https://doi.org/10.1007/s40292-020-00406-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-020-00406-w