Abstract
Participation in ultra-endurance running (UER) events continues to grow across ages, including youth athletes. The 50- and 100-km are the most popular distances among youth athletes. Most youth athletes are between 16–18 years; however, some runners younger than 12 years have successfully completed UER events. Parents, athletes, coaches, race directors, and medical professionals often seek advice regarding the safety of youth athletes participating in these events, especially with regard to potential short and long-term health consequences. UER may impact key organ systems during growth and development. We propose a decision-making process, based on current knowledge and the experience of the consensus group that addresses age regulations, medical and psychological well-being, training status and race-specific factors (such as distance, elevation change, remoteness, ambient temperatures, level of medical assistance, and type of provisions provided by the race organizers) to use until evidence of long-term consequences of UER in youth athletes is available. These recommendations are aimed at safe participation in UER events for youth athletes with a proper and individualized assessment.

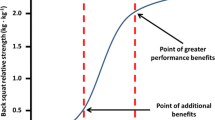
reproduced from Scheer et al. [6], with permission from Edizioni Minerva Medica)

Similar content being viewed by others
References
Scheer V, Basset P, Giovanelli N, Vernillo G, Millet GP, Costa RJS. Defining off-road running: a position statement from the Ultra Sports Science Foundation. Int J Sports Med. 2020;41:275–84.
Knechtle B, Rüst CA, Rosemann T, Lepers R. Age-related changes in 100-km ultra-marathon running performance. Age (Dordrecht). 2012;34:1033–45.
da Fonseca-Engelhardt K, Knechtle B, Rüst CA, Knechtle P, Lepers R, Rosemann T. Participation and performance trends in ultra-endurance running races under extreme conditions—“Spartathlon” versus “Badwater.” Extrem Physiol Med. 2013;2:15.
Cejka N, Rüst CA, Lepers R, Onywera V, Rosemann T, Knechtle B. Participation and performance trends in 100-km ultra-marathons worldwide. J Sports Sci. 2014;32:354–66.
Scheer V. Participation trends of ultra endurance events. Sports Med Arthrosc Rev. 2019;27:3–7.
Scheer V, Hoffman MD. Too much too early? An analysis of worldwide childhood ultramarathon participation and attrition in adulthood. J Sports Med Phys Fit. 2019;59:1363–8.
Scheer V, Di Gangi S, Villiger E, Nikolaidis PT, Rosemann T, Knechtle B. Age-related participation and performance trends of children and adolescents in ultramarathon running. Res Sports Med. 2020;23:1–11.
Scheer V, Di Gangi S, Villiger E, Rosemann T, Nikolaidis PT, Knechtle B. Participation and performance analysis in children and adolescents competing in time-limited ultra-endurance running events. Int J Environ Res Public Health. 2020;17:1628.
Scheer V, Hoffman MD. Should children be running ultramarathons? Curr Sports Med Rep. 2018;17:282.
Knoth C, Knechtle B, Rüst CA, Rosemann T, Lepers R. Participation and performance trends in multistage ultramarathons-the “Marathon des Sables” 2003–2012. Extreme Physiol Med. 2012;1:13.
Scheer BV, Murray DA. Ultramarathon running injuries. In: Doral MN, Karlsson J, editors. Sports injuries. Berlin: Springer; 2015.
Scheer V, Sousa CV, Valero D, Knechtle B, Nikolaidis PT, Valero E. A descriptive study on health, training and social aspects of adults that participated in ultra endurance running as youth athletes. J Sports Med Phys Fit. 2020. https://doi.org/10.23736/S0022-4707.20.11198-8.
Roberts WO. Can children and adolescents run marathons? Sports Med. 2007;37:299–301.
Roberts WO, Nicholson WG. Youth marathon runners and race day medical risk over 26 years. Clin J Sport Med. 2010;20:318–21.
Rice SG, Waniewski S. Children and marathoning: how young is too young? Clin J Sport Med. 2003;13:369–73.
Roberts WO. Children and running: at what distance safe? Clin J Sport Med. 2005;15:109–10 (author reply 110–111).
Krabak BJ, Roberts WO, Tenforde AS, Ackerman KE, Adami P, Baggish A, et al. Youth running consensus statement: minimizing risks of injury and illness in youth runners. Br J Sports Med. 2020. https://doi.org/10.1136/bjsports-2020-102518.
Knechtle B, Scheer V, Nikolaidis PT, Sousa CV. Participation and performance trends in the oldest 100-km ultramarathon in the world. Int J Environ Res Public Health. 2020;17:1719.
UTMB. 2020 Regulations. 2020. https://www.utmbmontblanc.com/en/page/16/Regulations.html. Accessed 15 Jan 2020.
Comrades Marathon. 2018. https://www.comrades.com. Accessed Feb 18 2018.
Ebell MH, Siwek J, Weiss BD, Woolf SH, Susman J, Ewigman B, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Am Board Fam Pract. 2004;17:59–67.
Donnelly JE, Hillman CH, Castelli D, Etnier JL, Lee S, Tomporowski P, et al. Physical activity, fitness, cognitive function, and academic achievement in children: a systematic review. Med Sci Sports Exerc. 2016;48:1197.
Tiller NB, Stewart GM, Illidi CR, Levine BD. Exercise is medicine? The cardiorespiratory implications of ultra-marathon. Curr Sports Med Rep. 2020;19:290–7.
Traiperm N, Gatterer H, Wille M, Burtscher M. Cardiac troponins in young marathon runners. Am J Cardiol. 2012;110:594–8.
Maufrais C, Millet GP, Schuster I, Rupp T, Nottin S. Progressive and biphasic cardiac responses during extreme mountain ultramarathon. Am J Physiol Heart Circ Physiol. 2016;310:H1340–8.
McClean G, Riding NR, Ardern CL, Farooq A, Pieles GE, Watt V, et al. Electrical and structural adaptations of the paediatric athlete’s heart: a systematic review with meta-analysis. Br J Sports Med. 2018;52:230.
Pieles GE, Stuart AG. The adolescent athlete’s heart; a miniature adult or grown-up child? Clin Cardiol. 2020;43:852–62.
Sharma S, Maron BJ, Whyte G, Firoozi S, Elliott PM, McKenna WJ. Physiologic limits of left ventricular hypertrophy in elite junior athletes. J Am Coll Cardiol. 2002;40:1431–6.
Makan J, Sharma S, Firoozi S, Whyte G, Jackson PG, McKenna WJ. Physiological upper limits of ventricular cavity size in highly trained adolescent athletes. Heart. 2005;91:495–9.
Claessen G, La Gerche A. Exercise-induced cardiac fatigue: the need for speed: perspectives. J Physiol. 2016;594:2781–2.
Wundersitz D, Williamson J, Nadurata V, Nolan K, Lavie C, Kingsley M. The impact of a 21-day ultra-endurance ride on the heart in young, adult and older adult recreational cyclists. Int J Cardiol. 2019;286:137–42.
Andersen K, Farahmand B, Ahlbom A, Held C, Ljunghall S, Michaëlsson K, et al. Risk of arrhythmias in 52 755 long-distance cross-country skiers: a cohort study. Eur Heart J. 2013;34:3624–31.
Tso J, Kim JH. Master endurance athletes and cardiovascular controversies. Curr Sports Med Rep. 2020;19:113–8.
Garnvik LE, Malmo V, Janszky I, Wisløff U, Loennechen JP, Nes BM. Estimated cardiorespiratory fitness and risk of atrial fibrillation: the Nord-Trøndelag Health Study. Med Sci Sports Exerc. 2019;51:2491–7.
Drca N, Wolk A, Jensen-Urstad M, Larsson SC. Atrial fibrillation is associated with different levels of physical activity levels at different ages in men. Heart. 2014;100:1037–42.
Drezner JA, O’Connor FG, Harmon KG, Fields KB, Asplund CA, Asif IM, et al. AMSSM position statement on cardiovascular preparticipation screening in athletes: current evidence, knowledge gaps, recommendations and future directions. Br J Sports Med. 2017;51:153–67.
McKinney J, Johri AM, Poirier P, Fournier A, Goodman JM, Moulson N, et al. Canadian cardiovascular society cardiovascular screening of competitive athletes: the utility of the screening electrocardiogram to predict sudden cardiac death. Can J Cardiol. 2019;35:1557–66.
Corrado D, Pelliccia A, Bjørnstad HH, Vanhees L, Biffi A, Borjesson M, et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Eur Heart J. 2005;26:516–24.
Quanjer PH, Stanojevic S, Stocks J, Hall GL, Prasad KVV, Cole TJ, et al. Changes in the FEV1/FVC ratio during childhood and adolescence: an intercontinental study. Eur Respir J. 2010;36:1391–9.
Del Giacco SR, Firinu D, Bjermer L, Carlsen K-H. Exercise and asthma: an overview. European Clin Resp J. 2015;2:27984.
Maat RC, Røksund OD, Halvorsen T, Skadberg BT, Olofsson J, Ellingsen TA, et al. Audiovisual assessment of exercise-induced laryngeal obstruction: reliability and validity of observations. Eur Arch Otorhinolaryngol. 2009;266:1929–36.
MacKelvie KJ. Is there a critical period for bone response to weight-bearing exercise in children and adolescents? a systematic review * Commentary. Br J Sports Med. 2002;36:250–7.
Lloyd RS, Oliver JL, Faigenbaum AD, Myer GD, De Ste Croix MBA. Chronological age vs. biological maturation: implications for exercise programming in youth. J Strength Cond Res. 2014;28:1454–64.
Faulkner RA, Davison KS, Bailey DA, Mirwald RL, Baxter-Jones AD. Size-corrected BMD decreases during peak linear growth: implications for fracture incidence during adolescence. J Bone Miner Res. 2006;21:1864–70.
Brenner JS. Council on sports medicine and fitness. Sports specialization and intensive training in young athletes. Pediatrics. 2016;138:e20162148.
Krabak BJ, Tenforde AS, Davis IS, Fredericson M, Harrast MA, d’Hemecourt P, et al. Youth distance running: strategies for training and injury reduction. Curr Sports Med Rep. 2019;18:53–9.
Tenforde AS, Sayres LC, McCurdy ML, Collado H, Sainani KL, Fredericson M. Overuse injuries in high school runners: lifetime prevalence and prevention strategies. PMR. 2011;3:125–31.
Barrack MT, Fredericson M, Tenforde AS, Nattiv A. Evidence of a cumulative effect for risk factors predicting low bone mass among male adolescent athletes. Br J Sports Med. 2017;51:200–5.
Barrack MT, Rauh MJ, Nichols JF. Prevalence of and traits associated with low BMD among female adolescent runners. Med Sci Sport Exerc. 2008;40:2015–21.
Tenforde AS, Fredericson M, Sayres LC, Cutti P, Sainani KL. Identifying sex-specific risk factors for low bone mineral density in adolescent runners. Am J Sports Med. 2015;43:1494–504.
Warden SJ, Davis IS, Fredericson M. Management and prevention of bone stress injuries in long-distance runners. J Orthop Sports Phys Ther. 2014;44:749–65.
Field AE. Prospective study of physical activity and risk of developing a stress fracture among preadolescent and adolescent girls. Arch Pediatr Adolesc Med. 2011;165:723.
Tenforde AS, Roberts WO, Krabak BJ, Davis IS, Fredericson M, Luke AC, et al. Recommendations to optimize health in youth runners. Strength Conditioning J. 2020;42:76–82.
Costa RJS, Snipe R, Camões-Costa V, Scheer V, Murray A. The impact of gastrointestinal symptoms and dermatological injuries on nutritional intake and hydration status during ultramarathon events. Sports Med Open. 2016;2:16.
Costa RJS, Snipe RMJ, Kitic CM, Gibson PR. Systematic review: exercise-induced gastrointestinal syndrome-implications for health and intestinal disease. Aliment Pharmacol Ther. 2017;46:246–65.
Costa RJS, Gaskell SK, McCubbin AJ, Snipe RMJ. Exertional-heat stress-associated gastrointestinal perturbations during Olympic sports: Management strategies for athletes preparing and competing in the 2020 Tokyo Olympic Games. Temperature. 2020;7:58–88.
Gill SK, Teixeira A, Rama L, Prestes J, Rosado F, Hankey J, et al. Circulatory endotoxin concentration and cytokine profile in response to exertional-heat stress during a multi-stage ultra-marathon competition. Exerc Immunol Rev. 2015;21:114–28.
Costa RJS, Hoffman MD, Stellingwerff T. Considerations for ultra-endurance activities: part 1—nutrition. Res Sports Med. 2019;27:166–81.
Costa RJS, Knechtle B, Tarnopolsky M, Hoffman MD. Nutrition for ultramarathon running: trail, track, and road. Int J Sport Nutr Exerc Metab. 2019;2:130–40.
Costa RJS, Oliver SJ, Laing SJ, Walters R, Bilzon JLJ, Walsh NP. Influence of timing of postexercise carbohydrate-protein ingestion on selected immune indices. Int J Sport Nutr Exerc Metab. 2009;19:366–84.
Walsh NP, Gleeson M, Shephard RJ, Gleeson M, Woods JA, Bishop NC, et al. Position statement. Part one: immune function and exercise. Exerc Immunol Rev. 2011;17:6–63.
Robson-Ansley P, Howatson G, Tallent J, Mitcheson K, Walshe I, Toms C, et al. Prevalence of allergy and upper respiratory tract symptoms in runners of the London marathon. Med Sci Sports Exerc. 2012;44:999–1004.
Walsh NP, Gleeson M, Pyne DB, Nieman DC, Dhabhar FS, Shephard RJ, et al. Position statement. Part two: maintaining immune health. Exerc Immunol Rev. 2011;17:64–103.
Peake JM, Neubauer O, Walsh NP, Simpson RJ. Recovery of the immune system after exercise. J Appl Physiol. 2017;122:1077–87.
Desbrow B, McCormack J, Burke LM, Cox GR, Fallon K, Hislop M, et al. Sports Dietitians Australia position statement: sports nutrition for the adolescent athlete. Int J Sport Nutr Exerc Metab. 2014;24:570–84.
Thomas DT, Erdman KA, Burke LM. American College of Sports Medicine joint position statement. Nutrition and athletic performance. Med Sci Sports Exerc. 2016;48:543–68.
Rauh MJ, Margherita AJ, Rice SG, Koepsell TD, Rivara FP. High school cross country running injuries: a longitudinal study. Clin J Sport Med. 2000;10:110–6.
Tirabassi J, Brou L, Khodaee M, Lefort R, Fields SK, Comstock RD. Epidemiology of high school sports-related injuries resulting in medical disqualification: 2005–2006 through 2013–2014 academic years. Am J Sports Med. 2016;44:2925–32.
Beachy G, Rauh M. Middle school injuries: a 20-year (1988–2008) multisport evaluation. J Athl Train. 2014;49:493–506.
Changstrom B, Brill J, Hecht S. Severe exercise-associated hyponatremia in a collegiate American football player. Curr Sports Med Rep. 2017;16:343–5.
Noakes TD, Myburgh KH, Schall R. Peak treadmill running velocity during the VO2 max test predicts running performance. J Sports Sci. 1990;8:35–45.
Fornasiero A, Savoldelli A, Fruet D, Boccia G, Pellegrini B, Schena F. Physiological intensity profile, exercise load and performance predictors of a 65-km mountain ultra-marathon. J Sports Sci. 2017;36(11):1287–95. https://doi.org/10.1080/02640414.2017.1374707.
Rowland TW. Developmental aspects of physiological function relating to aerobic exercise in children. Sports Med. 1990;10:255–66.
Kemper HCG, Verschuur R. Longitudinal study of maximal aerobic power in teenagers. Ann Hum Biol. 1987;14:435–44.
Bouchard C, An P, Rice T, Skinner JS, Wilmore JH, Gagnon J, et al. Familial aggregation of Vo2max response to exercise training: results from the HERITAGE Family Study. J Appl Physiol. 1999;87:1003–8.
Larsen HB, Nolan T, Borch C, Sondergaard H. Training response of adolescent Kenyan town and village boys to endurance running. Scand J Med Sci Sports. 2005;15:48–57.
Mccann DJ, Adams WC. The size-independent oxygen cost of running. Med Sci Sports Exerc. 2003;35:1049–56.
Daniels J, Oldridge N, Nagle F, White B. Differences and changes in VO2 among young runners 10 to 18 years of age. Med Sci Sports. 1978;10:200–3.
Krahenbuhl G, Morgan D, Pangrazi R. Longitudinal changes in distance-running performance of young males. Int J Sports Med. 1989;10:92–6.
Tan PL, Tan FH, Bosch AN. Assessment of differences in the anthropometric, physiological and training characteristics of finishers and non-finishers in a tropical 161-km ultra-marathon. Int J Exerc Sci. 2017;10:465–78.
Krouse RZ, Ransdell LB, Lucas SM, Pritchard ME. Motivation, goal orientation, coaching, and training habits of women ultrarunners. J Strength Conditioning Res. 2011;25:2835–42.
O’Loughlin E, Nikolaidis PT, Rosemann T, Knechtle B. Different predictor variables for women and men in ultra-marathon running—the Wellington Urban Ultramarathon 2018. Int J Environ Res Public Health. 2019;16(10):1844. https://doi.org/10.3390/ijerph16101844.
Kłapcińska B, Waśkiewicz Z, Chrapusta SJ, Sadowska-Krępa E, Czuba M, Langfort J. Metabolic responses to a 48-h ultra-marathon run in middle-aged male amateur runners. Eur J Appl Physiol. 2013;113:2781–93.
Huxley DJ, O’Connor D, Healey PA. An examination of the training profiles and injuries in elite youth track and field athletes. Eur J Sport Sci. 2014;14:185–92.
Sawyer SM, Afifi RA, Bearinger LH, Blakemore S-J, Dick B, Ezeh AC, et al. Adolescence: a foundation for future health. Lancet. 2012;379:1630–40.
Loucks AB. Low energy availability in the marathon and other endurance sports. Sports Med. 2007;37:348–52.
Lewis NA, Collins D, Pedlar CR, Rogers JP. Can clinicians and scientists explain and prevent unexplained underperformance syndrome in elite athletes: an interdisciplinary perspective and 2016 update. BMJ Open Sport Exerc Med. 2015;1:e000063.
Mountjoy M, Sundgot-Borgen JK, Burke LM, Ackerman KE, Blauwet C, Constantini N, et al. IOC consensus statement on relative energy deficiency in sport (RED-S): 2018 update. Br J Sports Med. 2018;52:687–97.
Soligard T, Schwellnus M, Alonso J-M, Bahr R, Clarsen B, Dijkstra HP, et al. How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br J Sports Med. 2016;50:1030–41.
Schwellnus M, Soligard T, Alonso J-M, Bahr R, Clarsen B, Dijkstra HP, et al. How much is too much? (Part 2) International Olympic Committee consensus statement on load in sport and risk of illness. Br J Sports Med. 2016;50:1043–52.
Drinkwater BL, Kupprat IC, Denton JE, Crist JL, Horvath SM. Response of prepubertal girls and college women to work in the heat. J Appl Physiol. 1977;43:1046–53.
Shibasaki M, Inoue Y, Kondo N, Iwata A. Thermoregulatory responses of prepubertal boys and young men during moderate exercise. Eur J Appl Physiol. 1997;75:212–8.
Hew-Butler T, Rosner MH, Fowkes-Godek S, Dugas JP, Hoffman MD, Lewis DP, et al. Statement of the 3rd International exercise-associated hyponatremia consensus development conference, Carlsbad, California, 2015. Br J Sports Med. 2015;49:1432–46.
Hoffman MD, Stellingwerff T, Costa RJS. Considerations for ultra-endurance activities: part 2—hydration. Res Sports Med. 2019;27:182–94.
Rowland T. Fluid replacement requirements for child athletes. Sports Med. 2011;41:279–88.
Hoffman MD, Snipe RMJ, Costa RJS. Ad libitum drinking adequately supports hydration during 2 h of running in different ambient temperatures. Eur J Appl Physiol. 2018;118:2687–97.
McCubbin AJ, Allanson BA, Caldwell Odgers JN, Cort MM, Costa RJS, Cox GR, et al. Sports dietitians Australia position statement: nutrition for exercise in hot environments. Int J Sport Nutr Exerc Metab. 2020;30:83–98.
O’Connor FG. Sports medicine: exertional heat illness. FP Essent. 2019;482:15–9.
Stevens CJ, Taylor L, Dascombe BJ. Cooling during exercise: an overlooked strategy for enhancing endurance performance in the heat. Sports Med. 2017;47:829–41.
Rodenberg RE, Gustafson S. Iron as an ergogenic aid: ironclad evidence? Curr Sports Med Rep. 2007;6:258–64.
Dempster S, Britton R, Murray A, Costa RJS. Case study: nutrition and hydration status during 4,254 km of running over 78 consecutive days. Int J Sport Nutr Exerc Metab. 2013;23:533–41.
Gropper SS, Blessing D, Dunham K, Barksdale JM. Iron status of female collegiate athletes involved in different sports. Biol Trace Elem Res. 2006;109:001–14.
Erikson E, Erikson JM. The life cycle completed: extended version. New York: Norton, WW; 1998.
Allen E, Marotz L. Development profiles pre-birth through twelve. 4th ed. Albany: Thomas Delmar Learning; 2003.
Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78.
Hoffman MD, Pasternak A, Rogers IR, Khodaee M, Hill JC, Townes DA, et al. Medical services at ultra-endurance foot races in remote environments: medical issues and consensus guidelines. Sports Med. 2014;44:1055–69.
International Trail Running Association. Medical and saftey guidline. 2020. https://itra.run/documents/security_guidelines/Security_Guidelines_ITRA_EN.pdf. Accessed 15 Jan 2020.
Scheer BV, Valero-Burgos E, Costa R. Myasthenia gravis and endurance exercise. Am J Phys Med Rehabil. 2012;91:725–7.
Hein IM, De Vries MC, Troost PW, Meynen G, Van Goudoever JB, Lindauer RJL. Informed consent instead of assent is appropriate in children from the age of twelve: policy implications of new findings on children’s competence to consent to clinical research. BMC Med Ethics. 2015;16:76.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No financial support was received for the conduct of this study, or for the preparation or publication of this manuscript.
Conflict of interests
The authors declare that there are no conflict of interests.
Availability of data and material
Not applicable.
Authors’ contribution
VS—conception and design of study, organization of consensus group, manuscript writing and editing. RC—manuscript writing and editing. SD—manuscript writing and editing. BK—manuscript writing and editing. PTN—manuscript writing and editing. WOR—manuscript writing and editing. OS—manuscript writing and editing. AT—manuscript writing and editing. BK—conception and design of study, organization of consensus group, manuscript writing and editing.
Rights and permissions
About this article
Cite this article
Scheer, V., Costa, R.J.S., Doutreleau, S. et al. Recommendations on Youth Participation in Ultra-Endurance Running Events: A Consensus Statement. Sports Med 51, 1123–1135 (2021). https://doi.org/10.1007/s40279-021-01441-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-021-01441-w