Abstract
Objectives
We aimed to synthesise knowledge on the relative social value of child and adult health.
Methods
Quantitative and qualitative studies that evaluated the willingness of the public to prioritise treatments for children over adults were included. A search to September 2023 was undertaken. Completeness of reporting was assessed using a checklist derived from Johnston et al. Findings were tabulated by study type (matching/person trade-off, discrete choice experiment, willingness to pay, opinion survey or qualitative). Evidence in favour of children was considered in total, by length or quality of life, methodology and respondent characteristics.
Results
Eighty-eight studies were included; willingness to pay (n = 9), matching/person trade-off (n = 12), discrete choice experiments (n = 29), opinion surveys (n = 22) and qualitative (n = 16), with one study simultaneously included as an opinion survey. From 88 studies, 81 results could be ascertained. Across all studies irrespective of method or other characteristics, 42 findings supported prioritising children, while 12 provided evidence favouring adults in preference to children. The remainder supported equal prioritisation or found diverse or unclear views. Of those studies considering prioritisation within the under 18 years of age group, nine findings favoured older children over younger children (including for life saving interventions), six favoured younger children and five found diverse views.
Conclusions
The balance of evidence suggests the general public favours prioritising children over adults, but this view was not found across all studies. There are research gaps in understanding the public’s views on the value of health gains to very young children and the motivation behind the public’s views on the value of child relative to adult health gains.
Clinical Trial Registration
The review is registered at PROSPERO number: CRD42021244593. There were two amendments to the protocol: (1) some additional search terms were added to the search strategy prior to screening to ensure coverage and (2) a more formal quality assessment was added to the process at the data extraction stage. This assessment had not been identified at the protocol writing stage.
Similar content being viewed by others
This systematic review of the evidence exploring the relative value of child to adult health found some public support for giving greater weight to the identical health gain for children, but this pro-child preference was not found across all studies. |
Evidence based on parents’ willingness to pay for their own child’s health relative to their own and from responses to trade-off questions with clearly described and measured health gain find greater relative value for child health than identified in opinion surveys. The latter tend to use more general questions about prioritisation and access and find more egalitarian views. |
Future research that seeks to understand the public’s motivation for their views on the values of health gain across different ages, including infants, would be of value. This may help shed light on the variability in results by study method, and the extent of public support for implementing pro-child healthcare prioritisation. |
1 Introduction
Economic evaluations typically adopt welfarist or extra-welfarist frameworks, usually assigning the same value to each unit of health regardless of the recipient. [1]. The possibility that the social value of health gain varies with characteristics such as age, health-related lifestyle and social role has been explored in preference elicitation studies [2]. As noted by Nord, “any procedure for estimating the social value of a health care outcome … must reflect community views on the trade-offs between treating different groups of patients.” [3].
We use the term social value to mean judgement about “what is good for society” [4]. This covers three uses: (i) an individual’s judgement of the relative importance of outcomes for society taking into consideration their equity concerns over efficiency; (ii) a decision-maker’s aggregation of individual social judgements; and (iii) A decision-maker’s aggregation of judgements by individuals about what is good for themselves or their families, where aggregation could allow for distributional concerns.
Differences in age-related social value potentially arise through both equity (fairness/justice) and efficiency considerations [5]. Equity-based claims typically draw on achieving equal health outcomes across the life course, or a ‘fair innings’ [6], and on children’s vulnerability [7]. Efficiency-based claims draw upon such factors as the effect that the health of a child may have on family members, age-based differences in current and future productivity, and in the capacity to benefit from treatment. These motivations are described in Table 1.
Decision-making agencies (e.g. Australia’s Pharmaceutical Benefits Advisory Committee, England’s National Institute for Health and Care Excellence, and the Canadian Agency for Drugs and Technologies in Health) typically assess the strength and relevance of evidence on the social value of health gains and public concerns around equity [8]. Some decision-making agencies explicitly weight health gain to certain groups based, for example, on condition severity (e.g. Norway [9], England [10] and the Netherlands [11, 12]). Severity weights, particularly when derived based on absolute health shortfall, are more likely to be operationalised in considerations that affect younger patients [13]. Agencies also use implicit means to incorporate equity considerations into funding and reimbursement decisions [14].
Whilst no decision-making agencies explicitly apply different weights to health gains for children, whether the intervention is targeted at children may be a deliberative factor [15,16,17]. The case has been made that the public values health gains to children more than adults [18]. Conducting health technology assessments (HTAs) relevant to children is acknowledged to be challenging [19], with tension between respecting equality legislation and pro-child preferences. Greater clarity on public views on the social value of child relative to adult health gains, the methods used to identify those views, and the relationship between methods and identified public views are important to supporting HTA deliberations and methods development.
The purpose of this review was to synthesise knowledge around the social value for health gains for children (aged less than 18 years) compared to adults, drawing on evidence from the health economics literature and fields such as transport and environment economics. The inclusion of the latter two fields is pertinent to our review given their overlap to public health interventions and because empirical studies in these fields often define health gains in generic terms such as length and quality of life. Values derived from comparing context-specific gains (e.g. the relative value of improving the safety of a child compared with an adult cyclist) would be considered independently. Evidence spans a range of methods assessing the relative value for changes in children’s health versus adults and includes length of life and health-related quality of life (HRQoL). As noted by Devlin et al. [20], it is the role of decision makers not instrument developers or health economists “to make the necessary value judgements” when considering what approach to take in valuing child health. Therefore, the scope of the review was developed to identify and synthesise evidence relevant to HTA bodies when considering how the social values of health gains should be accommodated. Statements are often made that the public values child health gains more than adult health gains; however, importantly the review aims to place this in the context of heterogeneous views.
This review asked five questions:
-
1.
Do individuals give different weights to the same health gain when received by a child compared to an adult?
-
2.
Does the estimated value of child to adult health vary by methodology?
-
3.
Does the estimated value of child to adult health differ for extensions of length of life versus improvements in HRQoL and across different HRQoL domains?
-
4.
Does the estimated value of child to adult health differ among the public, decision makers, patients, parents or according to specific respondent characteristics?
-
5.
Does the estimated value of child health vary by the age of the child?
2 Methods
A protocol outlining the systematic search strategy for studies reporting data on the relative value of the health of children compared to adults, and within children of different ages, was developed and registered with the Prospective Register of Systematic Reviews (CRD42021244593). Reporting has followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [21]. The analysis of qualitative data used a thematic synthesis [22].
2.1 Eligibility Criteria
Original empirical studies (not a review, commentary, protocol, abstract or book review), published in English, and with an empirical method that assessed the value of health of children compared to adults, or within children of different ages, were eligible. Study types included were: direct trade-offs or choices between health gains/losses to children versus adults; comparison between the value given to child health (HRQoL and/or years of life) relative to the value given to adult health in terms of another attribute (e.g. money or own time); public opinion surveys on the extent to which different age groups should be prioritised within healthcare; and qualitative studies eliciting views, opinions and reasons for different values on child health relative to adults. Opinion surveys on healthcare prioritisation that discussed saving lives were included as these can contextualise other empirical work rather than provide a weighting. Studies that analysed data from another study were excluded unless they included additional data or analyses related to the research question of this review.
Stated or revealed preference studies were excluded if they only included the relative value for a prevented fatality. Prevented fatalities combine the expected future number of years to be lived and the value of time spent in different health states over that period, and for different people; it is difficult to disentangle the value of healthy and less-healthy time from unobserved assumptions about life expectancy. All population samples were included: general public, patients, clinicians, decision makers, specific age groups, parents and students.
2.2 Information Sources
Five databases were searched to 8 December, 2021: Ovid MEDLINE, Ovid EMBASE, Ovid Transport Database, EconLit and Web of Science Social Science Citation. Additionally, the grey literature was searched using the Canadian Agency for Drugs and Technologies in Health’s Grey Matters: A Practical Tool for Searching Health-Related Grey Literature [23]. All agencies listed under HTAs and health economics were searched using keyword searches. Additional material was identified through reference lists of retrieved articles, citation searches on studies that met inclusion criteria, contact with review authors and collaborators, and scanning reviews in related topics.
2.3 Search Strategy
A search strategy was developed iteratively. Twelve “pearl” papers provided the initial list of keywords [24]. Search terms were developed to cover: age, priority setting, context (e.g. HTA, healthcare) and method (e.g. willingness to pay [WTP], discrete choice experiment [DCE], person trade-off [PTO]). Search terms are provided in the Tables A and B of the Electronic Supplementary Material (ESM). Searches were limited to papers indexed from 1990 onwards. Extraction, assessment, and synthesis of quantitative and qualitative studies were undertaken separately.
2.4 Selection Process
Titles and abstracts were screened followed by full papers. One reviewer (TP) conducted the initial screen, with 20% of title/abstracts and full papers blind screened by MS and RR. Disagreements and queries arising were discussed and agreed.
2.5 Data Items
Four reviewers (TP, MH, AS, RR) extracted quantitative data and one reviewer (MS) extracted qualitative data using standardised extraction forms appropriate to study type. Two studies in each quantitative study type were independently extracted by two reviewers to ensure comparability. Data extracted included study characteristics, sample population details, study methods (recruitment, mode of administration, perspective, type of health gain, analysis) and study results (summary of findings including weights for health or length of life gain by age for identical health loss).
2.6 Reporting Quality
Quantitative studies were assessed using a checklist derived from Johnston et al. [25] covering best-practice recommendations for stated preference studies intended to inform decision making. Of the 23 recommendations, eight focus on reporting guidelines and recommendations for conducting work [25]. The remainder were re-formatted as a 15-item checklist with a simple scoring system: 1 (Yes, high quality), 2 (Probably or unclear), 3 (No, low quality) or NA (not applicable to the study type). The checklist was applied to all studies, accepting that some criteria were less relevant to some study types. The checklist is included in Table C of the ESM. Four reviewers (TP, MH, AS, RR) conducted the assessments. Two studies in each type were independently extracted by two reviewers to ensure comparability. No formal quality assessment was conducted on the qualitative studies. Given the nature of the review, reporting bias was not able to be assessed.
2.7 Presenting Study Outcomes
Where possible, findings were presented as a ratio of relative weight attributed to children or adolescents compared to adults. For some studies, this required calculation of the ratio using reported results. To address the review questions, the findings from the quantitative studies were given two classifications, first, whether they provide evidence for children of any age compared to adults and second, whether they provide evidence between different childhood age groups. For the childhood age groups, for clarity of meaning we have assigned age ranges to the descriptions; however, some studies only used descriptors. The categories used to classify findings are listed below.
Provides evidence of relative weight of children compared to adults:
-
(a)
Favouring a ‘child’ over an adult (where the age of child is not specified, or age groups overlap);
-
(b)
Favouring infants and very young children (aged 0–5 years) over adults;
-
(c)
Favouring children (aged 5–18 years) over adults;
-
(d)
Evidence for different child ages (e.g. specific ages such as 5, 10 and 15 years, or different age groups, such as very young children aged less than 5 years);
-
(e)
Favouring younger adults (aged 18–35 years) over children of any age;
-
(f)
Favouring adults over children (where the age of the adult is not clearly defined, for example as ‘working age’);
-
(g)
Equal priority between adults and children;
-
(h)
Diverse or inconclusive views;
-
(i)
Evidence relating to life saving;
-
(j)
Unclear or difficult to interpret.
Findings relating to within childhood age categories:
-
(a)
Favouring older children (aged 12 years and older) over younger children (aged less than 12 years);
-
(b)
Favouring younger children (aged less than 12 years) over older (aged 12 years and older) children;
-
(c)
No evidence for age-related preferences within childhood age groups.
Results reported for multiple age groups within a single study have been classified appropriate to the findings for each age group.
Classification was based on decision rules developed and agreed a priori by the research team and applied by each reviewer (described in Table F of the ESM) with ambiguities discussed within the team. Statistically significant findings are highlighted in the tables and figures. All findings were reported irrespective of statistical significance, as we aimed to be inclusive and identify trends.
More than one ‘finding’ per study was included where different questions (e.g. using different methods) or different types of health gain (e.g. extending life vs HRQoL) were addressed. Multiple results within a category (e.g. different types of health condition, or different number of years of extended life) and different sub-groups (e.g. young or old responders) were not treated as separate findings.
2.8 Synthesis Methods
Results were tabulated by study type. We aimed to consider consistency (within and between study types) and explore explanations for divergence of findings. Findings were considered as providing evidence for prioritising children (classification 1a–1c above), evidence against doing so (1d–1g) or not providing clear evidence (1h–1j). The percentage providing evidence in favour of prioritising children was considered in total (review question 1), across different research methods (review question 2), across different types of health gain (review question 3) and across different respondents (review question 4). To address the final review question, we considered the number of findings favouring younger children over older children (2a and b). Counting of findings does not consider the precision or magnitude of the results, nor study quality. These are addressed within the results section as a reflection on the overall body of evidence. Weighting findings was not undertaken because of the variability in age comparisons within and across studies, the heterogeneity of results (e.g. between means and medians) and the different study methods, which do not lend themselves to comparable estimates of precision. Furthermore, even within single-study types, the range of settings and conditions (i.e. disease specific and generic) is highly variable.
For qualitative studies, consistent with thematic synthesis guidelines [21], participant quotations and text under the results/findings or conclusion/discussion sections were imported into NVivo Plus (version 12; QSR International, Burlington, MA, USA) software. One investigator (MS) performed line-by-line coding of the findings from studies generated by the database search, and inductively identified concepts about participants’ experiences and perspectives on HTA and policy for children compared to adults. Similar concepts were then grouped into themes. Following this, and in consultation with TP, MH and RR, a coding structure was developed to capture the concepts about participants’ experiences and perspectives on prioritisation for children compared to adults. To ensure that coding captured all relevant issues and reflected primary data, researcher triangulation was used, with four reviewers (MS, TP, MH, RR) independently reviewing the preliminary themes and analytical framework and discussing the addition or revision of themes.
3 Results
This section describes included studies, the results from the quality assessment and study findings. A summary of results extracted from individual studies is shown in Table F of the ESM. Findings on the associations with respondent characteristics are in Table H of the ESM.
3.1 Study Selection
We identified 4135 articles, of which 181 full texts were reviewed with 71 quantitative and 14 qualitative papers meeting the inclusion criteria (one paper [26] included in both). A PRISMA flow diagram is shown in Fig. 1. No additional studies were identified from the grey literature that were not also found as published articles in the citation databases. A list of all 102 excluded studies and the reason for their exclusion can be found in Table E of the ESM.
Study identification and selection. The study by Werntof et al. [27] is included in opinion survey and qualitative studies, hence the number of studies within each classification does not sum to the total. DCE discrete choice experiment, GTO gain trade off, PTO person trade-off, VSL value of a statistical life, WTP willingness to pay
Quantitative research methods included: matching (PTO or health gain trade-off), sometimes referred to as benefit trade-off or equivalence studies), DCE, WTP and opinion survey. Categorisation was based on the definitions shown in Table D of the ESM. In some cases, the method category was not clear or more than one method was included. Two studies (Prosser 2005, 2011) [27, 28] included time trade-off questions asking adults their willingness to give up time at the end of their life both to avoid illness for themselves and a hypothetical child, in addition to WTP; for simplicity these are included under WTP. Additionally, some studies reported different components of the study or different subgroups in more than one article.
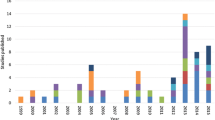
3.2 Study Characteristics
Study characteristics are summarised in Table 2 and details of individual studies in Table F of the ESM. Of the 88 studies, 33% were DCEs, 25% opinion surveys, 18% qualitative, 14% matching/PTO and 10% WTP. The majority were European (55%) followed by North American (20%) with 65% published since 2011. Of the 29 studies that used DCEs, 87% were published after 2011, with only opinion surveys, matching/PTO and qualitative studies published before 2000. Sample size ranged from less than 50 to more than 1000, with 27% having more than 1000 participants. Participants in 65 (74%) of the studies included either the general population or other groups of adults, with only seven (8%) including parents as a specified sub-group. The majority (56%) asked participants to take the perspective of a decision maker with only a small number (9%) seeking a ‘self’ perspective. Most of the studies (86%) considered generic conditions being defined in terms of severity, function or length/quality of life.
3.3 Reporting Quality
The quality of reporting assessment scores by study type is shown in Fig. 2. Details of assessments across each criterion for each paper are shown in the ESM.
Quality assessments. Assessment questions: 1. SCENARIO DESCRIPTION. 2. QUALITATIVE TESTING, 3. EXPERIMENTAL DESIGN, 4. MODE OF DATA COLLECTION, 5. CHOICE BETWEEN WILLINGNESS TO PAY (WTP) AND WILLINGNESS TO ACCEPT (WTA), 6. INCENTIVE-COMPATIBLE RESPONSE FORMATS, 7. NO-ANSWER OPTION, 8. PAYMENT VEHICLE, 9. HYPOTHETICAL BIAS, 10. ECONOMETRIC ESTIMATOR SELECTION, 11. HETEROGENEITY, 12. RESPONSE ANOMALIES, 13. GENERALISABILITY, 14. INTERNAL VALIDITY, 15. TRANSPARENCY IN REPORTING. Scoring 1 = Yes (high quality/low risk of bias), 2 = Probably or unclear, 3 = No (low quality/high risk of bias), NA = not applicable for the study types. DCE discrete choice experiment, WTP willingness to pay
There were some areas of concern regarding reporting, particularly in relation to generalisability and ensuring that the scenarios and questions were understood for example through reported qualitative pilot work. An overview for each criterion across the study types is summarised in the Table G of the ESM.
3.4 Overall Synthesis
A detailed summary by study method can be found in the ESM.
3.4.1 Quantitative Studies
From 71 quantitative studies, 80 separate ‘findings’ were identified; of which 42 support prioritising children over adults, 12 provide evidence that responders favour treating adults in preference to children, seven support equal prioritisation and 13 report diverse views. In total, 12 studies included comparisons of different childhood age groups (Table F of the ESM), given the heterogeneity in age groups considered, the findings have not been able to be synthesised in Table 3. Table F of the ESM also includes the estimates of ratios or odds ratios between age groups for the matching studies, DCEs and WTP. These have been used to identify findings that favour age groups; however, further synthesis has not been undertaken given the heterogeneity of study types and key characteristics such as health states considered, perspective and participants. Table 3 shows the percentage of quantitative findings supporting favouring children over adults, disaggregated by study characteristics. Figure 3a–c provide a schematic of the findings of each study by research method. There was a high degree of heterogeneity in age categories for children and adults across the studies including descriptive terms (e.g. ‘child’, ‘adult’), broad and narrow age ranges, and discrete ages. This variation is captured in Fig. 3a–c and the age or age ranges considered in each study and those most favoured. Of those studies that included different childhood age groups, four (33%) favoured older children over those aged less than 5 years, two (16%) showed no difference, while six (50%) favoured young children (aged 5 years or younger) over older children. Of note, of the six studies that favoured young children, all but one were for specific conditions including organ transplant [29], asthma [30] and influenza vaccination [27, 31, 32]. Given the heterogeneity of study types and characteristics including age groups, health conditions and perspectives, a meta-analysis of the quantitative findings was not possible. Studies exploring the interaction between age and severity of health states (described either as a percentage of quality of life [33, 34] or as life expectancy without treatment [35]) do not find a consistent pattern.
a Summary of matching/person trade-off findings showing included and preferred ages. Red squares and bars indicate when an age or age range was preferred over others included in the study. Black diamonds indicate discrete ages that were included in the study but not preferred and black lines with arrows indicate age ranges that were included in the study but not preferred. Studies that reported no age preference are indicated by having all black lines and diamonds for all ages [18, 47, 58, 63, 65, 69,70,71,72,73,74,75]. Note the Petrou et al. [18] results shows only a sample of their results based on children (5-year differences) compared to adults aged 40 years. ext. extension, phys. physical, QoL quality of life, yr years. b Summary of willingness-to-pay (WTP) findings showing included and preferred ages. Red squares and bars indicate when an age or age range was preferred. Black diamonds indicate discrete ages that were included in the study but not preferred and black lines with arrows indicate age ranges that were included in the study but not preferred. Studies that reported no age preference are indicated by having all black lines and diamonds for all ages [27, 28, 30, 68, 76,77,78,79]. gastrointest. gastrointestinal, QoL quality of life, TTO time trade-off. c Summary of discrete choice experiment findings showing included and preferred ages. Red squares and bars indicate when an age or age range was preferred. Black diamonds indicate discrete ages that were included in the study but not preferred and black lines with arrows indicate age ranges that were included in the study but not preferred. Studies that reported no age preference are indicated by having all black lines and diamonds for all ages [29, 31, 32, 60, 80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103]
3.4.2 Qualitative Studies
Sixteen articles published from 1995 to 2023, involving at least 1260 people from ten countries were identified (Fig. 1). Characteristics of the included studies are summarised in Table 1, with the details of each study provided in the Table I of the ESM. No study included children or young people as respondents, 11 included members of the public and six reported the inclusion of parents. Five included policy makers, or public health professionals, four decision makers and five health professionals. Thematic synthesis identified two major themes with regard to prioritising treatment in children compared to adults: maximising health and social gains and navigating ethical and moral concerns.
3.4.2.1 Maximising Health and Social Gains
Participants discussed age in the context of wanting to maximise health gains but some considered age to be an imperfect indicator of capacity to benefit from treatment over a life course. Some policymakers and administrators believed that deviating from existing HTA frameworks was not warranted because cost-effectiveness and health-loss criteria could be seen to already “favour the young over the old” believing we should not deviate from standardised principles, such as it relates to “efficiency and equity across age groups” [33]. For example, they felt that clinical guidelines already account for age-related factors relevant to treatment success and, therefore, the effects of age were already part of decision making. At the societal level, however, age was also deemed relevant to the quality of life and well-being of carers and some professionals questioned current economic evaluations underpinning value assessments for child health technologies [34].
Relatedly, some people felt the health system and economy would likely benefit from prioritising younger people in the long term by preventing chronic diseases that burden the health system and having improved market participation. Similarly, some participants also believed the benefits of prioritising children may extend to other social benefits and these other benefits should be accounted for in HTAs, including impacts on the family unit (e.g. well-being and productivity) [34,35,36]. “So that’s lost income for our family and it’s also lost tax dollars.” [36]
3.4.2.2 Moral and Ethical Concerns
Participants in the majority of studies believed children should be prioritised from a fair innings perspective [33, 34, 36,37,38,39,40]. The perception was that it is fair and morally appropriate to prioritise young people to enable experience of the lifespan and recognition that a lifespan needs to end at some point [34, 36, 41]. Similarly, participants from one study referred to children as a “distinct” population from a sociocultural perspective and, therefore, held the view that there was a moral obligation to prioritise children’s health [34]. Children were considered disadvantaged as they lacked a voice in society and there are significant barriers in developing and accessing child-specific drugs [34]. In addition, some health professionals felt this normative distinction meant society should accept a “higher [cost effectiveness] threshold when dealing with children than with adults” [34, 36]. Participants from other studies highlighted other vulnerable and disadvantaged groups they believed should be prioritised, including socioeconomically disadvantaged individuals [33, 39], women [42], and elderly individuals. It was felt that society should consider the relative disadvantage of a population beyond the value assessment in economic evaluations. In addition, some of the public believed a medical urgency should take precedence over age, and the “sickest” should be “rescued” [43] regardless of age [44].
Conversely, some older participants, consistent with an egalitarian framework, believed “all patients should be treated equally when interacting with the health system, and that differentiating across social groups lacked ethical or clinical justification” [33]. They felt everybody should be entitled to the healthcare they need and want, with little discussion of economic implications, “people should have the same life-saving treatment, no matter what their age” [44], “[You] can’t say a 74-year-old does not have the same rights as a 20-year-old […], you cannot say that per se.” [41]. This reluctance to engage in prioritising patients was consistent with acknowledgements from the public that they had little understanding of allocation protocols [43], found it difficult making these types of decisions and “playing god” [40] or had concerns about imposing “arbitrary” age cut-offs, believing that decision making should be based on the disease and the population experiencing regardless of age [45]. This was despite also recognising scarcity and the need to make resource allocation decisions in health, which they felt was “highly problematic” [41].
4 Discussion
Our review identified an extensive evidence base for the social value of the health of children and young people compared with adults across a range of methods, questions and perspectives. To our knowledge, this is the first comprehensive review that brings together evidence from different research methods, disciplines and countries that have explored comparisons involving child health. The review helps to create an in-depth understanding of public preferences and a better awareness of how methods and framing impact upon estimates of social value. Quality-adjusted life-years or equivalent are widely used as the basis for assessing and funding interventions. However, compared with adults, the HRQoL utilities that underpin QALYs for children and young people are subject to multiple areas of uncertainty including whether social values for children over adults should be explicitly considered in decisions [46]. We provide an overview of the evidence for each of the review questions.
4.1 Do Individuals Give a Different Weight to the Same Health Gain When Received by a Child Compared to an Adult?
Of the 39 ‘findings’ considering the same health gain (the same years of life extension or the same HRQoL improvement for the same duration), the majority (72%) support prioritising children. Whilst the balance of evidence suggests public opinion favours children over adults, this view was not always evident. There are diverse views within studies, with a small number of studies reporting little or no support for prioritising child health. This may reflect the way questions were framed (e.g. around a specific condition of situation) or the perspective participants were asked to take. There is insufficient agreement across studies to recommend specific age groups or weightings to apply to health gains in children and adults, particularly not between children and young adults. In addition, whilst with most of the quantitative studies it was possible to identify an odds ratio or equivalent measure that could be used to quantify the magnitude of favouring one age group over another, the heterogeneity of study types and key characteristics including the framing of questions and comparisons and age groups considered, limits the ability to synthesise these estimates by way of a meta-analysis or other summary of weights.
4.2 Does the Estimated Value of Child to Adult Health Vary by Research Methodology?
The evidence supporting favouring children varies by study methodology with WTP studies finding the most support (82%), followed by matching/PTO studies (71%), then DCE (63%) and lastly opinion surveys (20%). The WTP results may be due to the respondents’ own child’s health (or a hypothetical family member) generally being valued and being influenced by altruistic preferences or interdependent utility functions.
The lower support in opinion surveys relative to Matching/PTO studies replicates Nord [47] who found opinion survey respondents did not prioritise between patients on the basis of their age but in PTO interviews respondents prioritised the young even where life expectancies were the same. Nord proposed four possible explanations (1) sample difference; (2) survey framing effects between choosing between individual patients at the ‘admission level’ and matching interviews framed in a less personal context of programme budgets; (3) differences in question structure whereby surveys asked about broad age groups or general comparisons versus the PTO questions of specific numbers and ages treated. Nord suggests the PTO questions “may have made the consequences of choosing different options clearer to the respondents and hence encouraged more reflective responses” [47]; and (4) the PTO technique, which may encourage people to engage in numerical trade-offs rather than focus on principles of equal entitlement to treatment.
The slightly lower support found within for DCE studies, which allow for trade-offs over multiple variables, compared with matching/PTO, which usually only allow trade-offs with respect to age, may arise from artificially focusing respondents’ attention and hence perceived importance on age. However, no studies incorporated a design to explicitly test the impact of this focus.
The findings from qualitative studies are supportive of the overall synthesis of findings from the quantitative studies in that they identify diverse reasons for and against favouring children and young people. Moral and ethical concerns and maximising health gains underpin the appropriateness of prioritising children and young people over adults. Reasons against favouring children and young people include notions of egalitarianism, expectations that existing policies and guidelines already consider age and that age is only one aspect to consider when identifying vulnerable groups. Other methodological aspects of studies also associated with the findings include the perspective, the similarity of health gain for different age groups, and framing as health gains or losses.
4.2.1 Perspective (Decision Maker/Citizen/Individual)
Most matching/PTO and DCE study questions were framed from a ‘decision-maker’ perspective. Opinion surveys were split between ‘citizen’ and ‘decision maker’ and WTP studies mostly adopted an individual perspective with preferences on allocation within the family. The higher weight towards protecting child health in WTP studies may, in part, be due to the different perspectives.
Whether a personal perspective is appropriate for public healthcare distribution is a normative judgement. Culyer noted that this perspective may not be appropriate evidence for decisions about equity: “the source of value for making judgements about equity lies outside, or is extrinsic to, preferences ... The whole point of making a judgement about justice is so to frame it that it is (and can be seen to be) a judgement made independently of the interests of the individual making it.” [48]. If the parent, as a member of society, contributes to valuation of health through public preferences (e.g. the relative importance of depression vs pain from their own perspective), why they should not also influence the relative importance of alleviating pain in their children versus depression in themselves is noteworthy.
The influence of framing questions either as a ‘citizen’ or a ‘decision maker’ on the relative value of child versus adult health is not clear. Both tap into individual views of social value and both are recipients of healthcare, i.e. potential future beneficiaries. The extent to which personal benefit is more strongly reflected in the ‘citizen’ perspective is unclear. As questions relate to children rather than the individual themselves, this distinction is ambiguous. For example, Denburg et al. [34] describe the perspective as being from ‘a citizen advisor to a health system administrator’ as a decision maker rather than a citizen because they considered that the advice relates to treatments for a condition that responders are unlikely to have. Despite this ambiguity, it is clear that WTP for health gains of family members speaks to the equity of resource allocation within the household and not to questions of fairness for social collective resource allocation. The perspective given to responders in the text of the study is likely to matter less than whom the questions are referring to.
4.2.2 Controlling for Size of Health Gain
The review suggests that studies which ask questions about clearly identified health gains (e.g. one extra year of life, or avoiding a well-described period of illness), which are held constant between groups, are more likely to find a willingness to prioritise children. This is surprising because where the gain of health is unclear, this may be interpreted as offering a greater benefit to younger patients who have more years ahead of them therefore more years in which to benefit. More generally, studies that ask about the distribution of a quantifiable single health gain are more likely to favour children than questions implying a general move towards prioritisation of children. This could arise if respondents are cautious of longer term implications of prioritisation and the potential for moves towards something they may consider as discriminatory. For example, Tong et al. [49] note that respondents were unwilling to continue to prioritise children for receiving transplant organs if older patients would never receive a donor organ.
Some WTP and matching/PTO studies find higher values for ages with a higher risk of complications from the health condition (e.g. influenza in the very young or very old [28] and asthma control [29]). Respondents may take into consideration age-related risk factors, suggesting a need for the validation of interpretation of the health condition by age group in future studies. Additionally, respondents may interpret an identically described health state as having a different consequence on health-related quality of life for children. For example, limitations in personal care for children may be seen as being mitigated by parental support [20] . Without a better understanding of what drives responses, it is difficult to isolate a willingness to prioritise based on age per se versus perceptions of age-related clinical need or age-related judgement of the impact of the health limitation on health-related quality of life.
There is substantial revealed and stated preference work exploring the relative willingness to pay for reducing health risk or preventing a fatality to children compared with adults not included in this review because the health gain varied between children and adults. Revealed preference studies based on purchases of products with safety features (such as vehicles) report mixed results. For example, data on child-safety seats [50] estimated that the value of reducing risk to children aged under 5 years was about twice that of adults. Conversely, smaller estimates for the VSL for children compared with adults based on data on bicycle helmet sales have been reported [51]. A recent review of stated preference studies valuing avoiding mortality risks found WTP to reduce risks to children were between 1.2 and 2.8 times higher than for reducing mortality risk for adults [52]. However, this may not translate to a willingness to prioritise children for the same health gain. The extent to which VSL varies across the whole life course remains contested. Revealed preference studies based on wage-risk trade-offs have found an inverted U shape with age (e.g. Aldy and Viscusi [53] find a peak at age 46 years). Stated preference studies asking respondents’ willingness to pay for mortality risk reductions or reductions in the risk of future sick-days find inconsistent results (e.g. Alberini et al., [54], Krupnick, [55] Cameron and DeShazo [56]). Inferring relative values for children compared with adults is not possible from the wage equation literature or from studies relating to the personal demand for health based on own income as valuing children necessitates identifying other-regarding preferences.
4.2.3 Framing as Health Gain or Loss
One possible explanation for differences according to the study method is if respondents feel differently about favouring one age group over another when the question is framed in terms of gains or losses. Li et al. [57] found that when a vaccine intervention was framed as ‘lives saved’ (for 2 years of life gain) the age of beneficiaries was not considered relevant to prioritisation, yet when framed as ‘lives lost’ (with the same remaining life expectancy) respondents chose to prioritise the young. For most studies, it is difficult to know whether respondents interpret the intervention or health state as a gain or a loss. For example, if the question is described as ‘avoiding an illness’, this could be interpreted as either framing. The importance of the way questions are framed remains an important methodological factor that impacts on study findings in ways that are unable to be quantified.
4.3 Does the Estimated Value of Child to Adult Health Differ for Extensions of Length of Life Versus Improvements in HRQoL and Across Different HRQoL Domains?
The proportion of studies generating evidence for a greater weight on health gains by children varied by the type of health gain. For length of life, 54% favoured children; for HRQoL improvement, 72% favoured children; combined length of life and HRQoL (mostly DCEs), 67% favoured children; and where health gain was ‘unclear’, only 36% favoured children (63% from opinion surveys). Two matching/PTO studies included different types of health gain within the same study [47, 58], enabling a more direct comparison. However, neither found a clear difference in weights given to children and adults for the different types of health gain.
The evidence does not provide a clear distinction in age weighting between HRQoL compared with length of life. Very little evidence explored the distinction between different aspects of HRQoL.
4.4 Does the Estimated Value of Child to Adult Health Differ Among the Public, Decision Makers, Patients, Parents and Other Respondent Characteristics?
Details of the association between responder characteristics and study findings are shown in Table H of the ESM. The characteristic tested most frequently was age (n = 26) with half finding this to be non-significant. More studies (n = 10) concluded that older responders were less willing to prioritise children than younger responders compared with those concluding the opposite (n = 3). The reason for the variation in views by respondent age is not known. Thirteen studies assessed sex, with most finding no significant effect. Parent status was tested in nine studies of which six found that parents were more likely to favour children. Of the four studies including only parents as responders, all found support for favouring children; however, these were all WTP studies with a personal rather than social perspective.
There was no clear difference in opinions between different groups of responders. Although parents report greater willingness to favour their own children over themselves, it is not clear if this generalises to a social preference in favour of children. There is some suggestion that older responders are less willing to favour children.
4.5 Does the Estimated Value of Child Health Vary from Newborn to Late Adolescence?
Of those studies considering prioritisation within the under 18 years of age group, nine findings favoured older children over younger (including for life-saving interventions), six favoured younger children and five found diverse views. Charney et al. [59] conducted interviews with 54 respondents as part of a pilot study for a larger study that explored reasoning for responses. These interviews revealed that some respondents preferred to save an 8-year-old rather than a two-year-old because “the eight-year-old is more aware of its situation, is more of a ‘person’ and has had a much greater investment of parental effort and emotion.”
Of the 42 findings favouring children over adults, 20 provided evidence only for children 5 years of age and older. Only three of the studies favouring children framed the question for children under 5 years of age; and all found greater weight was given to the under 5 years of age group compared with adults [31, 60] or all other ages [61]. The remainder spanned age groups or referred to ‘children/child’ without clear reference to age. Overall, given the slight weight of evidence in favour of older versus younger children, we cannot assume that the evidence for children aged between 5 and 18 years compared to adults can be applied to children under the age of 5 years. Of note in those studies where young children (< 5 years of age) were favoured over older children all, except for one, addressed specific rather than generic health conditions such as vaccination where elderly individuals were also favoured over younger adults. This is consistent with a view that vulnerability to a condition is also relevant to determining whether one group should be favoured over another.
5 Limitations Within the Included Studies
Despite the extensive number of papers identified, there are some important evidence gaps.
5.1 Evidence Not Available on the Views of All Age Groups
Most studies did not recruit respondents under 18 years of age and the youngest were 15 years of age. Similarly, many do not capture the views of very old individuals [49, 62,63,64]. Many WTP studies focus only on people with young children at home who are likely to be younger adults.
5.2 Health Gain Between Age Groups is not Constant in Some Studies
Of the 80 findings identified, 39 (49%) included questions in which health gain was constant between age groups; while for 35 (44%) this was unclear. This may not be a limitation if different study types and descriptions of health gain tap into different resource allocation considerations.
5.3 Evidence Across Different Childhood Age Groups is Limited
Most studies included only one age group for children defined by a range or a single age. Very few included age groups that would allow the assessment of variation between adolescents and younger children, and even fewer included very young age groups (<5 years).
5.4 Evidence on the Effect of Different Health Conditions/States is Limited
It is expected that framing, description, and focus of the health conditions being addressed will influence stated preferences including age-related preferences. However, the review did not identify studies specifically addressing these questions, and study heterogeneity does not allow any meaningful conclusions to be drawn.
5.5 Minimal Understanding of Respondent Interpretation and Motivation
Few studies report the rationale for respondent choices. When pilot studies were conducted, they were generally poorly reported. Respondents may perceive the health gain to differ between age groups, and this can be the case even where years of life gain are constant [65] or the treatment intervention is the same (e.g. avoiding influenza or dialysis). It is not possible to identify the extent to which the possible motivations outlined in Table 1 are driving results. Furthermore, respondents may base responses on considerations that could be incorporated into benefit measurement such as parental productivity or other spillover effects. Failure to understand respondent motivation risks double counting of benefits.
6 Limitations of the Review
The search strategy was limited to papers that included terms relating to age and children within the abstract/key words. This enabled a sensitive search; however, studies exploring healthcare prioritisation more broadly may have evidence relating to the relative value of child versus adult health may be missed. This may mean that some studies where adult versus child health gains are a secondary consideration have been excluded. As with any search of this type, there are trade-offs between sensitivity, specificity and the yield of citations. The body of evidence on relative preferences for improving HRQoL between children and adults relies heavily on responses to questions that use a limited number of sample health conditions (such as influenza and asthma control) and questions about prioritisation for donor organs. Relative priorities for these may not generalise to other health interventions.
The review only included evidence published in English. Synthesising evidence from different cultures is problematic because the relative value of health gains for children compared to adults is culturally influenced, hence global evidence on average weights may not be generalisable. However, combining international evidence enables an evaluation of the impact of study methodology.
Most of the evidence is drawn from static questions relating to a single trade-off. However, respondents may hold views on the more dynamic nature of prioritisation. The study by Tong et al. [49] found that whilst responders were willing to prioritise children for transplant, they also wished to see a constraint on this if it led to a restriction on access to transplant for older aged recipients. The evidence identified here merges questions about measuring value with questions of access. The apparent inconsistency across methods may arise if individuals acknowledge greater gain from treating children yet also give weight to equity of access, and different question styles tap more or less strongly into these different concerns.
On balance, the evidence suggests a willingness to prioritise children. However, many studies do not demonstrate that respondents have good awareness that prioritising children would “not produce winners only” (Bobinac et al.) [66]. The zero-sum nature of prioritisation is often opaque, and without explicitly drawing attention to this and confirming preferences with this understanding there is a danger that opinions and preferences are a response to the framing of survey questions. The broad scope of the review has not allowed a meta-analysis of quantitative findings to be undertaken. This limits the ability to identify the magnitude of weights, if any, that could be justified for cost-effectiveness assessments of interventions specific to children and young people. Whilst there are a few studies of similar design where results could be combined, they present only a small fraction of the evidence on the research questions and if reported would provide undue emphasis.
Finally, we focused on the social value of child health gains versus adults. We did not include other considerations of decision making including the difficulty of generating cost-effectiveness evidence across patient age groups. The challenges of generating the same certainty of evidence for children arose as a theme within the qualitative studies, although was not discussed here.
7 Future Research
Our research has identified key areas for future research.
7.1 Methodological Considerations
There are several key methodological considerations that continue to contribute to the uncertainties in quantifying social preferences. Of particular importance is the influence of question framing, the specificity of the health condition and the contextual detail provided to respondents. This is not limited to positive and negative framing but also the extent to which concepts of opportunity costs and trade-offs between equity and efficiency are captured and understood.
7.2 Views on Prioritisation for Under 5-Year-Olds and Between Adolescents and Younger Children
There is little evidence on valuing quality and length of life gains for children under the age of five or between children of different age groups.
7.3 Influence of Cultural and Social Perspectives
Most of the evidence is from North America and Europe and there is little understanding of the role that differing cultural backgrounds or healthcare settings may play in social values and priorities.
7.4 Motivation for Preferences Remains Underexplored
There is a need to understand the motivation for peoples’ preferences. This is true for those who see a greater gain in treating children and those who see saving the lives of children to have no less value than saving the lives of elderly individuals. There remains uncertainty in understanding public views on fairness and particularly why equity of health across individuals at a single moment in time differs to considerations of equity over a lifetime. Furthermore, the extent to which pro-child preferences may be driven by spillover effects is uncertain.
7.5 Understanding How People Feel About Prioritising Age Groups in Practice
There is limited understanding of how people view the relative value of child to adult health in the context of real-world decision making. Individuals who give greater weight to children in PTO or DCE questions may or may not support the use of different cost-effective thresholds for HTAs.
7.6 WTP Comparisons Between Another Adult and Child
The only WTP study to compare third person adult (rather than self) to a third person child found a substantially lower ratio of WTP between children and adults; however, this study relied upon a WTP for a very small reduction in risk of ill-health. Future research which values both a child and a third person adult within the household and ask questions about health loss with certainty to avoid the additional complexity of asking about a reduction in the risk of health loss.
8 Conclusions
The balance of evidence included in this review suggests public opinion favours prioritising children over adults, but there is variation in this view reflecting different study methods, framing, perspective and other underlying concepts. Studies that ask about distribution of a quantifiable single health gain between children and adults (particularly older adults) are more likely to result in favouring children than questions implying a general move towards prioritisation of children.
The evidence was not able to distinguish between the value of life extensions versus improvements in HRQoL for children and adults, nor between the views of different groups of responders. Whilst there was a tendency for parents to give greater weight to children and older respondents less weight, this was not tested systematically across different empirical methods.
The evidence on the relative value of infants' health relative to the health of older children or adults is limited, but where within-childhood age comparisons were made, slightly more studies found responders were willing to prioritise older children over infants. There are outstanding research gaps in understanding the public’s views on the value of health gains to infants and the motivation behind the public’s views on the relative value of child relative to adult health gains.
Finally, the review identifies important implications relevant to the formulation of policy and decision frameworks for funding of interventions aimed at children and young people. Whilst a social value or weight in favour of children and young people is evident on average, the review found diversity of opinion both within and between studies. It needs to be recognised that there are many factors, including the health condition being evaluated, that influence both the direction and magnitude of the social value of the health of children and young people compared to adults.
References
Wailoo A, Tsuchiya A, McCabe C. Weighting must wait. Pharmacoeconomics. 2009;27(12):983–9.
Schwappach DLB. Resource allocation, social values and the QALY: a review of the debate and empirical evidence. Health Expect. 2002;5(3):210–22.
Nord E. The person-trade-off approach to valuing health care programs. Med Decis Making. 1995;15(3):201–8.
Culyer A. Social values in health and social care. The King's Fund: Commision on the Future of Health and Social Care in England; 2014.
Tsuchiya A. Age-related preferences and age weighting health benefits. Soc Sci Med. 1999;48(2):267–76.
Williams A. Intergenerational equity: an exploration of the ‘fair innings’ argument. Health Econ. 1997;6(2):117–32.
Culyer A. Commodities, characteristics of commodities, characteristics of people, utilities and the quality of life. In: Baldwin S, editor. The quality of life: perspectives and policies. London: Routledge; 1990.
Ghijben P, Gu Y, Lancsar E, Zavarsek S. Revealed and stated preferences of decision makers for priority setting in health technology assessment: a systematic review. Pharmacoeconomics. 2018;36(3):323–40.
Norwegian Medicines Agency. Guidelines for the submission of documentation for single technology assessment (STA) of pharmaceuticals. 2021. https://legemiddelverket.no/english/public-funding-and-pricing/documentation-for-sta/guidelines-for-the-submission-of-documentation-for-single-technology-assessment-sta-of-pharmaceuticals. Accessed 24 Oct 2023.
National Institute for Health and Care Excellence. Health technology evaluations: the manual. National Institute for Health and Care Excellence; 2022.
Dutch National Health Care Institute. Cost-effectiveness in practice [in Dutch]. 2015. https://www.zorginstituutnederland.nl/publicaties/rapport/2015/06/26/kosteneffectiviteit-in-de-praktijk. Accessed 24 Oct 2023.
Dutch National Healthcare Institute (Zorginstituut Nederland [ZIN]). Disease burden in practice [in Dutch]. 2018. https://www.zorginstituutnederland.nl/publicaties/rapport/2018/05/07/ziektelast-in-de-praktijk. Accessed 5 Sep 2023.
Skedgel C, Henderson N, Towse A, Mott D, Green C. Considering severity in health technology assessment: can we do better? Value Health. 2022;25(8):1399–403.
Zhang K, Garau M. International cost-effectiveness thresholds and modifiers for HTA decision making. Office of Health Economics. 2020. https://www.ohe.org/publications/international-cost-effectiveness-thresholds-and-modifiers-hta-decision-making. Accessed 24 Oct 2023.
Dakin H, Devlin N, Feng Y, Rice N, O’Neill P, Parkin D. The influence of cost-effectiveness and other factors on NICE decisions. Health Econ. 2015;24(10):1256–71.
Rawlins M, Barnett D, Stevens A. Pharmacoeconomics: NICE’s approach to decision-making. Br J Clin Pharmacol. 2010;70(3):346–9.
Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee (Version 5.0). Canberra: Commonwealth of Australia, Department of Health; 2016.
Petrou S, Kandala N-B, Robinson A, Baker R. A person trade-off study to estimate age-related weights for health gains in economic evaluation. Pharmacoeconomics. 2013;31(10):893–907.
Ungar WJ, Prosser LA, Burnett HF. Values and evidence colliding: health technology assessment in child health. Expert Rev Pharmacoeconomic Outcomes Res. 2013;13(4):417–9.
Devlin NJ, Pan T, Sculpher M, Jit M, Stolk E, Rowen D, et al. Using age-specific values for pediatric HRQoL in cost-effectiveness analysis: is there a problem to be solved? If so, how? Pharmacoeconomics. 2023;41(10):1165–74.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45.
Canadian Agency for Drugs and Technologies in Health. Grey matters: a practical tool for searching health-related grey literature. Ottawa: CADTH; 2019.
Schlosser RW, Wendt O, Bhavnani S, Nail-Chiwetalu B. Use of information-seeking strategies for developing systematic reviews and engaging in evidence-based practice: the application of traditional and comprehensive pearl growing: a review. Int J Language Commun Disord. 2006;41(5):567–82.
Johnston RJ, Boyle KJ, Adamowicz W, Bennett J, Brouwer R, Cameron TA, et al. Contemporary guidance for stated preference studies. J Assoc Environ Res Economists. 2017;4(2):319–405.
Werntoft E, Hallberg IR, Elmstahl S, Edberg A-K. Older people’s views of prioritization in health care. Aging Clin Exp Res. 2005;17(5):402–11.
Prosser LA, Bridges CB, Uyeki TM, Rego VH, Ray GT, Meltzer MI, et al. Values for preventing influenza-related morbidity and vaccine adverse events in children. Health Qual Life Outcomes. 2005;3:18.
Prosser LA, Payne K, Rusinak D, Shi P, Uyeki T, Messonnier M. Valuing health across the lifespan: health state preferences for seasonal influenza illnesses in patients of different ages. Value Health. 2011;14(1):135–43.
Howard K, Jan S, Rose JM, Wong G, Irving M, Tong A, et al. Community preferences for the allocation of donor organs for transplantation: a discrete choice study. Transplantation. 2015;99(3):560–7.
Blomquist GC, Dickie M, O’Conor RM. Willingness to pay for improving fatality risks and asthma symptoms: values for children and adults of all ages. Res Energy Econ. 2011;33(2):410–25.
Luyten J, Kessels R, Atkins KE, Jit M, van Hoek AJ. Quantifying the public’s view on social value judgments in vaccine decision-making: a discrete choice experiment. Soc Sci Med. 2019;228:181–93.
Prosser LA, Payne K, Rusinak D, Shi P, Messonnier M. Using a discrete choice experiment to elicit time trade-off and willingness-to-pay amounts for influenza health-related quality of life at different ages. Pharmacoeconomics. 2013;31(4):305–15.
Aidem JM. Stakeholder views on criteria and processes for priority setting in Norway: a qualitative study. Health Policy. 2017;121(6):683–90.
Denburg AE, Giacomini M, Ungar W, Abelson J. Ethical and social values for paediatric health technology assessment and drug policy. Int J Health Policy Manage. 2022;11(3):374–82.
Denburg AE, Giacomini M, Ungar WJ, Abelson J. ‘The problem is small enough, the problem is big enough’: a qualitative study of health technology assessment and public policy on drug funding decisions for children. Int J Equity Health. 2020;19(1):45.
Gauvreau CL, Wight L, Subasri M, Palmer A, Hayeems R, Croker A, et al. Access to novel drugs and therapeutics for children and youth: eliciting citizens’ values to inform public funding decisions. Health Expect. 2023;26(2):715–27.
Cookson R, Dolan P. Public views on health care rationing: a group discussion study. Health Policy. 1999;49(1–2):63–74.
Kuder LB, Roeder PW. Attitudes toward age-based health care rationing: a qualitative assessment. J Aging Health. 1995;7(2):301–27.
Lasseter G, Al-Janabi H, Trotter CL, Carroll FE, Christensen H. The views of the general public on prioritising vaccination programmes against childhood diseases: a qualitative study. PLoS ONE. 2018;13(6):0197374.
Powell PA, Rowen D, Rivero-Arias O, Tsuchiya A, Brazier JE. Valuing child and adolescent health: a qualitative study on different perspectives and priorities taken by the adult general public. Health Qual Life Outcomes. 2021;19(1):222.
Schweda M, Wohlke S, Inthorn J. “Not the years in themselves count”: the role of age for European citizens’ moral attitudes towards resource allocation in modern biomedicine. J Public Health. 2015;23(3):117–26.
Fortes P, Pereira P. Patient prioritization in medical emergencies: an ethical analysis. Revista Assoc Medica Brasil (1992). 2012;58(3):335–40.
Irving MJ, Tong A, Jan S, Wong G, Cass A, Allen RD, et al. Community preferences for the allocation of deceased donor organs for transplantation: a focus group study. Nephrol Dial Transplant. 2013;28(8):2187–93.
Werntoft E, Hallberg IR, Edberg A-K. Older people’s reasoning about age-related prioritization in health care. Nurs Ethics. 2007;14(3):399–412.
Ratcliffe J, Lancsar E, Walker R, Gu Y. Understanding what matters: an exploratory study to investigate the views of the general public for priority setting criteria in health care. Health Policy. 2017;121(6):653–62.
Rowen D, Rivero-Arias O, Devlin N, Ratcliffe J. Review of valuation methods of preference-based measures of health for economic evaluation in child and adolescent populations: where are we now and where are we going? Pharmacoeconomics. 2020;38(4):325–40.
Nord E, Street A, Richardson J, Kuhse H, Singer P. The significance of age and duration of effect in social evaluation of health care. Health Care Anal. 1996;4(2):103–11.
Culyer A. The political economy of social policy. Oxford: St Martin’s Press; 1980.
Tong A, Jan S, Wong G, Craig J, Irving M, Chadban S, et al. Patient preferences for the allocation of deceased donor kidneys for transplantation: a mixed methods study. Transplantation. 2012;94(Suppl. 10S):342.
Blomquist GC, Miller TR, Levy DT. Values of risk reduction implied by motorist use of protection equipment: new evidence from different populations. J Transport Econ Policy. 1996;30(1):55–66.
Jenkins RR, Owens N, Wiggins LB. Valuing reduced risks to children: the case of bicycle safety helmets. Contemp Econ Policy. 2001;19(4):397–408.
Robinson LA, Raich WJ, Hammitt JK, O’Keeffe L. Valuing children’s fatality risk reductions. J Benefit Cost Anal. 2019;10(2):156–77.
Aldy JE, Viscusi WK. Adjusting the value of a statistical life for age and cohort effects. Rev Econ Stat. 2008;90(3):573–81.
Alberini A, Cropper M, Krupnick A, Simon NB. Does the value of a statistical life vary with age and health status? Evidence from the US and Canada. J Environ Econ Manage. 2004;48(1):769–92.
Krupnick A. Mortality-risk valuation and age: stated preference evidence. Rev Environ Econ Policy. 2007;1(2):261–82.
Cameron TA, DeShazo JR. Demand for health risk reductions. J Environ Econ Manage. 2013;65(1):87–109.
Li M, Vietri J, Galvani AP, Chapman GB. How do people value life? Psychol Sci. 2010;21(2):163–7.
Richardson J, McKie J, Iezzi A, Maxwell A. Age weights for health services derived from the relative social willingness-to-pay instrument. Med Decis Mak. 2017;37(3):239–51.
Charny MC, Lewis PA, Farrow SC. Choosing who shall not be treated in the NHS. Soc Sci Med. 1989;28(12):1331–8.
Jehu-Appiah C, Baltussen R, Acquah C, Aikins M, D’Almeida SA, Bosu WK, et al. Balancing equity and efficiency in health priorities in Ghana: the use of multicriteria decision analysis. Value Health. 2008;11(7):1081–7.
Neuberger J, Adams D, MacMaster P, Maidment A, Speed M. Assessing priorities for allocation of donor liver grafts: survey of public and clinicians. BMJ (Clin Res Ed). 1998;317(7152):172–5.
Krutli P, Rosemann T, Tornblom KY, Smieszek T. How to fairly allocate scarce medical resources: ethical argumentation under scrutiny by health professionals and lay people. PLoS ONE. 2016;11(7): e0159086.
Reckers-Droog V, van Exel J, Brouwer W. Equity weights for priority setting in healthcare: severity, age, or both? Value Health. 2019;22(12):1441–9.
Reckers-Droog V, van Exel J, Brouwer W. Willingness to pay for health-related quality of life gains in relation to disease severity and the age of patients. Value Health. 2021;24(8):1182–92.
Tsuchiya A. The value of health at different ages. York: University of York, Centre for Health Economics York; 2001.
Bobinac A, van Exel NJA, Rutten FFH, Brouwer WBF. Valuing QALY gains by applying a societal perspective. Health Econ. 2013;22(10):1272–81.
Murray C. Rethinking DALYs. In: Murray C, Lopez A, editors. The global burden of disease. Harvard: Harvard University Press; 1996.
Balmford B, Bateman IJ, Bolt K, Day B, Ferrini S. The value of statistical life for adults and children: comparisons of the contingent valuation and chained approaches. Res Energy Econ. 2019;57:68–84.
Reckers-Droog V, Van Exel J, Brouwer W. Who should receive treatment? An empirical enquiry into the relationship between societal views and preferences concerning healthcare priority setting. PLoS ONE. 2018;13(6): e0198761.
Eisenberg D, Freed GL, Davis MM, Singer D, Prosser LA. Valuing health at different ages: evidence from a nationally representative survey in the US. Appl Health Econ Health Policy. 2011;9(3):149–56.
Baker R, Bateman I, Donaldson C, Jones-Lee M, Lancsar E, Loomes G, et al. Weighting and valuing quality-adjusted life-years using stated preference methods: pPreliminary results from the social value of a QALY project. Health Technol Assess. 2010;14(27):1–162.
Maestad O, Norheim OF. Eliciting people’s preferences for the distribution of health: a procedure for a more precise estimation of distributional weights. J Health Econ. 2009;28(3):570–7.
Jelsma J, Shumba D, Kristian H, De Weerdt W, De Cock P. Preferences of urban Zimbabweans for health and life lived at different ages. Bull World Health Org. 2002;80(3):204–9.
Rodríguez E, Pinto JL. The social value of health programmes: is age a relevant factor? Health Econ. 2000;9(7):611–21.
Busschbach JJ, Hessing DJ, De Charro FT. The utility of health at different stages in life: a quantitative approach. Soc Sci Med. 1993;37(2):153–8.
Reckers-Droog V, van Exel J, Brouwer W. Willingness to pay for quality and length of life gains in end of life patients of different ages. Soc Sci Med. 2021;279: 113987.
Hammitt JK, Haninger K. Valuing nonfatal health risk as a function of illness severity and duration: benefit transfer using QALYs. J Environ Econ Manage. 2017;82:17–38.
Dickie M, Messman VL. Parental altruism and the value of avoiding acute illness: are kids worth more than parents? J Environ Econ Manage. 2004;48(3):1146–74.
Liu J-T, Hammitt JK, Wang J-D, Liu J-L. Mother’s willingness to pay for her own and her child’s health: a contingent valuation study in Taiwan. Health Econ. 2000;9(4):319–26.
Delpasand M, Olyaaeemanesh A, Jaafaripooyan E, Abdollahiasl A, Davari M, Kazemi KA. Eliciting the public preferences for pharmaceutical subsidy in Iran: a discrete choice experiment study. J Pharm Policy Pract. 2021;14(1):59.
de Andrés-Nogales F, Cruz E, Calleja MÁ, Delgado O, Gorgas MQ, Espín J, et al. A multi-stakeholder multicriteria decision analysis for the reimbursement of orphan drugs (FinMHU-MCDA study). Orphanet J Rare Dis. 2021;16(1):186.
Lancsar E, Gu Y, Gyrd-Hansen D, Butler J, Ratcliffe J, Bulfone L. The relative value of different QALY types. J Health Econ. 2020;70: 102303.
Mentzakis E, Garcia-Goni M, Sequeira AR, Paolucci F. Equity and efficiency priorities within the Spanish health system: a discrete choice experiment eliciting stakeholders preferences. Health Policy Technol. 2019;8(1):30–41.
Lopez-Bastida J, Ramos-Goni JM, Aranda-Reneo I, Trapero-Bertran M, Kanavos P, Rodriguez MB. Using a stated preference discrete choice experiment to assess societal value from the perspective of decision-makers in Europe. Does it work for rare diseases? Health Policy. 2019;123(2):152–8.
Jouyani Y, Hadiyan M, Salehi M, Souri A. Using discrete choice model to elicit preference for health-care priority setting. J Educ Health Promot. 2019;8:117.
Sullivan T, Hansen P. Determining criteria and weights for prioritizing health technologies based on the preferences of the general population: a New Zealand pilot study. Value Health. 2017;20(4):679–86.
Farmakas A, Theodorou M, Galanis P, Karayiannis G, Ghobrial S, Polyzos N, et al. Public engagement in setting healthcare priorities: a ranking exercise in Cyprus. Cost Eff Resourc Alloc. 2017;15(1):16.
Skedgel C. The prioritization preferences of pan-canadian oncology drug review members and the canadian public: a stated-preferences comparison. Curr Oncol. 2016;23(5):322–8.
Skedgel C, Wailoo A, Akehurst R. Societal preferences for distributive justice in the allocation of health care resources: a latent class discrete choice experiment. Med Decis Mak. 2015;35(1):94–105.
Baji P, Garcia-Goni M, Gulacsi L, Mentzakis E, Paolucci F. Comparative analysis of decision maker preferences for equity/efficiency attributes in reimbursement decisions in three European countries. Eur J Health Econ. 2016;17(7):791–9.
van de Wetering EJ, van Exel NJA, Rose JM, Hoefman RJ, Brouwer WBF. Are some QALYs more equal than others? Eur J Health Econ. 2016;17(2):117v27.
van de Wetering L, van Exel J, Bobinac A, Brouwer WBF. Valuing QALYs in relation to equity considerations using a discrete choice experiment. Pharmacoeconomics. 2015;33(12):1289–300.
Luyten J, Kessels R, Goos P, Beutels P. Public preferences for prioritizing preventive and curative health care interventions: a discrete choice experiment. Value Health. 2015;18(2):224–33.
Whitty JA, Ratcliffe J, Chen G, Scuffham PA. Australian public preferences for the funding of new health technologies: a comparison of discrete choice and profile case best-worst scaling methods. Med Decis Mak. 2014;34(5):638–54.
Mentzakis E, Paolucci F, Rubicko G. Priority setting in the Austrian healthcare system: results from a discrete choice experiment and implications for mental health. J Mental Health Policy Econ. 2014;17(2):61–73.
Erdem S, Thompson C. Prioritising health service innovation investments using public preferences: a discrete choice experiment. BMC Health Serv Res. 2014;14(1):1–14.
Winkelhage J, Diederich A. The relevance of personal characteristics in allocating health care resources: controversial preferences of laypersons with different educational backgrounds. Int J Environ Res Public Health. 2012;9(1):223–43.
Defechereux T, Paolucci F, Mirelman A, Youngkong S, Botten G, Hagen TP, et al. Health care priority setting in Norway a multicriteria decision analysis. BMC Health Serv Res. 2012;12:39.
Lancsar E, Wildman J, Donaldson C, Ryan M, Baker R. Deriving distributional weights for QALYs through discrete choice experiments. J Health Econ. 2011;30(2):466–78.
Mortimer D, Segal L. Is the value of a life or life-year saved context specific? Further evidence from a discrete choice experiment. Cost Eff Resour Alloc. 2008;6:8.
Tappenden P, Brazier J, Ratcliffe J, Chilcott J. A stated preference binary choice experiment to explore NICE decision making. Pharmacoeconomics. 2007;25(8):685–93.
Schwappach DLB, Strasmann TJ. “Quick and dirty numbers”? The reliability of a stated-preference technique for the measurement of preferences for resource allocation. J Health Econ. 2006;25(3):432–48.
Baltussen R, Stolk E, Chisholm D, Aikins M. Towards a multi-criteria approach for priority setting: an application to Ghana. Health Econ. 2006;15(7):689–96.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. QUOKKA is funded through the Medical Future Research Fund (Grant number: APP1200816); TORCH is funded through the Medical Future Research Fund (Grant number: APP1199902).
Conflict of interest
Tessa Peasgood, Martin Howell, Rakhee Raghunandan, Amber Salisbury, Marcus Sellars, Gang Chen, Joanna Coast, Jonathan C. Craig, Nancy J. Devlin, Kirsten Howard, Emily Lancsar, Stavros Petrou, Julie Ratcliffe, Rosalie Viney, Germaine Wong, Richard Norman and Cam Donaldson have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
Conceptualisation: ND, KH, RV, EL, TP, MH, RN, CD; methodology: TP, MH, MS, RR, AS; formal analysis and investigation: TP, MH, RR, AS, MS; writing, original draft preparation: TP, MH; writing, review and editing: ALL; funding acquisition: ND, EL, RN, JR, RV, GC, MH, SP, JC, JCC, KH, CD, GW.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Peasgood, T., Howell, M., Raghunandan, R. et al. Systematic Review of the Relative Social Value of Child and Adult Health. PharmacoEconomics 42, 177–198 (2024). https://doi.org/10.1007/s40273-023-01327-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-023-01327-x